Spinal Puncture and Myelography
Note: Myelography is described herein. As a separate procedure, spinal puncture (lumbar or cervical) is carried out identically as described for myelography, except that contrast is not administered.
Spinal needle, 22 or 25 gauge, 9 cm length.
Lidocaine, 1% (preferentially buffered with bicarbonate).
Syringe, 20 mL, with extension tubing.
Iohexol (Omnipaque) 180 or 240 or 300.
Indications.
Magnetic resonance imaging (MRI) is the primary imaging modality of the spinal canal and its contents. Myelography should be performed in patients who are unable to undergo MRI, such as those with cardiac pacemakers, certain aneurysm clips, or those who have enough steel hardware to create unacceptable artifact over the areas to be imaged. Additionally, myelography should be undertaken in patients who are unable to tolerate MRI due to their size or to claustrophobia. Certain surgeons may prefer myelography to MRI preoperatively, as it gives better information regarding bony structures.
Consent.
The main risks of the procedure include pain (possibly radicular), contrast reaction, headache, infection, or, rarely, hematoma. Seizures may occur as a very rare complication. The risk of seizure may be higher for cervical myelogram. The seizure threshold may be lowered by certain medications, including major tranquilizers, antidepressants, and central nervous system (CNS) stimulants; such medications should be discontinued 48 hours before the procedure. Diabetic patients taking metformin (Glucophage) should stop taking metformin. A blood creatinine level should be obtained 48 hours after the procedure and if this is comparable to baseline value, the patient can resume metformin. This is the general recommendation for intravenous (IV) injections. Considering the amount of contrast used for myelography and the time that it takes for contrast to enter the blood stream, this approach is probably over cautious but it is still recommended as most myelography examinations are elective.
Patient Position.
Efforts should be made to position the patient’s head to prevent contrast from reaching the basal cisterns, especially during rolling and other maneuvers potentially necessary for the procedure. If the patient remains prone, the neck should be extended.
Lumbar—prone.
The patient may be slightly oblique to optimize access to the interlaminar space.
Cervical—prone.
May also be done with patient in lateral decubitus position if lateral fluoroscopy is not available. A lumbar approach may be used if cervical access is limited. In that case, the contrast is moved to the cervical region using a tiltable myelography table or by elevating the pelvis, with the hip and knee joints.
Landmarks
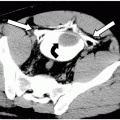
Lumbar.
The goal is to place the needle through the interlaminar space to access the subarachnoid space. In order to avoid the cord, access through the L2-3 interspace or below is recommended.
Cervical.
The posterior, superior one third of the spinal canal between C1 and C2 is the needle insertion site.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree