Nephrostomy
The role of percutaneous nephrostomy has expanded from that of a largely emergent procedure for the relief of acute supravesicular urinary tract obstruction to now include many elective indications in the initial percutaneous management of subacute or chronic upper urinary tract disease.
Indications.
In most cases, percutaneous access to the urinary tract is clearly indicated to relieve acute or subacute obstruction occurring at the level of the ureteropelvic junction (UPJ) to the ureterovesicular junction (UVJ) when accompanied by pain, azotemia, and/or urosepsis. If these findings and symptoms are absent, one must proceed more cautiously to avoid draining the collecting system of a kidney that is permanently nonfunctional due to chronic obstruction. Such concerns can often be addressed by comparing the current computed tomography (CT) or ultrasonography with previous scans and evaluating renal cortical thickness as an approximate indicator of functioning renal parenchyma. Nuclear medicine studies of differential function can be misleading because an obstructed system can show markedly reduced function that can rebound immediately after the obstruction is relieved. When bilateral obstructions are encountered, old studies are also invaluable in deciding which side to drain first by showing progression of disease and parenchymal viability of each kidney. General indications for percutaneous nephrostomy are as follows:
Relief of obstruction causing pain, azotemia, and/or urosepsis due to stone, neoplasm, blood clot, fungal ball, pyonephrosis, stricture, retroperitoneal fibrosis, or other lesion compressing the ureter. Iatrogenic causes of obstruction include inadvertant operative ligation of the ureter, complications of pyeloplasty, or postradiation fibrosis.
Temporary urinary diversion following operative ureteral laceration, urinoma formation, or ureteric fistulas.
Percutaneous access for pyeloplasty, operative or radiologic stone or foreign body removal, lithotripsy, nephroscopy, biopsy, and so on.
Diagnostic puncture for antegrade pyelography and renal Whittaker test.
Contraindications.
A significant bleeding diathesis is the only absolute contraindication to percutaneous nephrostomy. Overwhelming urosepsis is only a relative contraindication as percutaneous drainage may be lifesaving. Chronic obstruction with evidence of severe renal parenchymal loss is not an indication for percutaneous nephrostomy unless accompanied by pain, sepsis, or increasing azotemia.
Risks and Consent.
The major risk of percutaneous nephrostomy is hemorrhage, with less than 1% incidence of life-threatening bleeding and 0.2% risk of death. It is normal to have gross hematuria for 1-2 days after the procedure, but excessive or persistent bleeding may require treatment with tube tract upsizing (to tamponade the bleeding), vascular embolization, or even surgery. Septic complications range from clinically evident bacteremia and fever in 1-9% to septic shock in approximately 0.1%. Other complications include colonic perforation (0.2%), pneumothorax, urinoma, urine peritonitis, pain, catheter malfunction, and contrast allergy.
Workup. A directed workup should be obtained, including a history, physical, and pertinent laboratory data. As hemorrhage represents the most significant risk to the patient, the platelet count should be more than 50,000 and both the prothrombin time (PT) and partial thromboplastin time (PTT) should be no more than 1.3 times control. If not within acceptable limits, these values should be corrected with platelet and/or fresh frozen plasma (FFP) transfusion in every possible circumstance. A hemoglobin or hematocrit is important to establish a baseline. Blood urea nitrogen (BUN) and creatinine are important to document preprocedure renal impairment. Full urinalysis with urine cultures and, if necessary, blood cultures should be obtained before antibiotic therapy.
Antibiotics. On the basis of experience at our institution, antibiotics should always be given before percutaneous nephrostomy. Give cefotetan 1 g IV approximately 1 hour before the procedure.
Sedation. Depending on institutional policies, conscious sedation can be initiated either before or on the patient’s arrival in the case room. Continuous monitoring of oxygen saturation, cardiac rhythm, and blood pressure must be performed during conscious sedation. Midazolam 1 mg and fentanyl 50 µg IV aliquots may be administered p.r.n before and during the procedure.
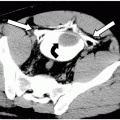
Imaging studies. Prior imaging studies that could yield anatomic information on the position of the kidney relative to the ipsilateral 12th rib, pleura, liver, spleen, and colon as well as information on variant anatomy such as malrotation, duplication, or ectopia should be reviewed and posted in the case room.
Planning the Approach.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree