Introduction
Ian Beggs
INTRODUCTION
Ultrasound is important for diagnosis and treatment in a wide range of musculoskeletal conditions and requires a firm grasp of anatomy, technique, and pathology. Ultrasound and magnetic resonance imaging (MRI) are complementary techniques. They are not competitive or mutually exclusive, and their use should be integrated. Technical advances in ultrasound1 have improved image quality and capability, resulting in better understanding of anatomy and pathology, and the development of new therapeutic techniques. A further advantage is that ultrasound has returned the radiologist to the “bedside,” providing the opportunity to examine the patient directly and garner more clinical information than is frequently available in a hastily scribbled requisition. Equally, many clinicians are beginning to perform their own specialty-specific ultrasound.
Ultrasound is best performed to answer specific questions. Symptoms that are located by a vague wave of the patient’s hand are probably better investigated by MRI. In many instances, a “targeted” ultrasound examination detects the abnormality.2 This is more likely with peripheral joints than with central joints, which benefit from a systematic examination. The shoulder is an example of a joint that should always be examined systematically. However, if the systematic approach yields no abnormality, it is worth completing the examination by reviewing the area that the patient points to as the site of pain.
Ergonomic issues are important. Repetitive strain injuries to the spine, shoulder, or wrist are common among sonologists.3,4 This is especially true in musculoskeletal ultrasound, and the examination technique should be considered carefully. Good technique also optimizes imaging. The position of both the sonologist and the patient should minimize strain on the operator. The height of the examination couch or stool should be altered accordingly. The sonologist’s arm should not be elevated or stretched, and twisting of the neck or trunk should be avoided. The transducer should be held close to its face to provide more control and reduce strain. The sonologist’s hand can rest on the patient and provide support. The transducer cable should be held in the opposite hand to reduce strain.
Copious jelly is needed. This may need to be thick for very superficial structures, but a standoff is not usually needed. The transducer should be moved slowly. Beginners frequently fail to recognize pathologic changes and even normal anatomy because they move the transducer too quickly. Fine movement may be helped by using one hand to position and angle the transducer and the other to push and pull it. Transducer pressure should be light, although increased pressure may be needed to displace superficial fat. Heavy pressure may efface a muscle hernia, or Doppler signal in synovitis or tendinosis.
Ultrasound is a dynamic examination. For example, the shoulder is examined in various positions to bring the relevant tendons into view, and the examination may be performed during abduction to look for impingement. Transducer pressure may distinguish between fluid that can be compressed and displaced and incompressible synovial hypertrophy in a swollen joint. Pressure may displace echogenic fluid and debris in rotator cuff or Achilles tendon tears and show whether the tear is complete or incomplete. Dorsiflexion and plantar flexion of the foot show whether an Achilles tendon tear is complete or partial and whether conservative or surgical management is appropriate; if the tear edges do not come together on plantar flexion, conservative management with the foot plantar flexed in a cast will be suboptimal.
Variable frequency linear array transducers in the 7 to 14 MHz range are adequate for most purposes, although small footprint and higher frequency transducers may be valuable when examining fingers or very superficial structures. There is a trade-off, however, between the better resolution of high-frequency transducers and the depth to which they can penetrate. Adjustments to gain, frequency, and focal zone are critical to optimize images.
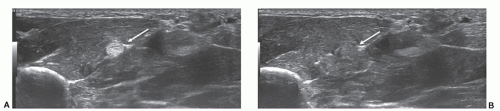
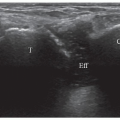
Anisotropy due to specular reflection is an artifact of major importance in musculoskeletal ultrasound. Specular reflectors reflect the ultrasound wave at the angle of insonation rather than producing a scattered reflection as, for example, does the liver. If the transducer is angled at 90° to a specular reflector, the sound is reflected back and detected; but if the ultrasound beam is not
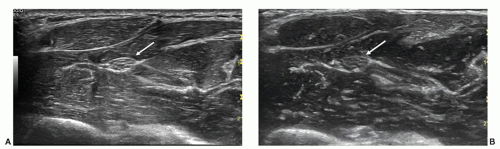
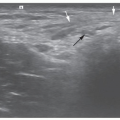
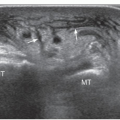
perpendicular, the sound will be reflected away from the transducer and the loss of reflected sound will result in a hypoechoic appearance. Tendons are the most important specular reflectors (Fig. 1.1), but ligaments, nerves, and muscles (Fig. 1.2) are also specular reflectors, and it is essential to ensure that the transducer is always perpendicular to these structures. Anisotropy is a particular problem with tendons that curve, for example, supraspinatus at the shoulder and tibialis posterior and the peroneal tendons at the ankle. Compound imaging produces sound waves at different angles and helps to overcome the problem of anisotropy and reduces noise and speckle.5
perpendicular, the sound will be reflected away from the transducer and the loss of reflected sound will result in a hypoechoic appearance. Tendons are the most important specular reflectors (Fig. 1.1), but ligaments, nerves, and muscles (Fig. 1.2) are also specular reflectors, and it is essential to ensure that the transducer is always perpendicular to these structures. Anisotropy is a particular problem with tendons that curve, for example, supraspinatus at the shoulder and tibialis posterior and the peroneal tendons at the ankle. Compound imaging produces sound waves at different angles and helps to overcome the problem of anisotropy and reduces noise and speckle.5
Beam steering also assists, although most experienced sonologists simply angle the transducer. Tissue harmonic imaging, which utilizes frequencies that arise within the tissue examined, helps to reduce other artifacts and improve contrast resolution.6
The effect of anisotropy can be harnessed profitably if a tendon is difficult to locate because it is surrounded by echogenic fat, for example, at the ankle. Altering transducer angulation to make the tendon hypoechoic (Fig. 1.3) will help locate the tendon. Then transducer angulation is corrected to examine the tendon.
Beam edge artifact (Fig. 1.4) is another artifact that can affect tendons, particularly large tendons. Loss of definition of the tendon edge and distal acoustic shadowing may simulate or obscure fluid in the tendon sheath.
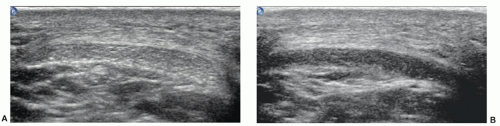
Extended field-of-view imaging (Fig. 1.5) may improve diagnostic accuracy, for example, in assessing atrophy of the rotator cuff muscles, and has a valuable role in teaching and presenting findings.
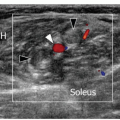
Doppler examination is essential in assessing tendinopathy7 and detecting (Fig. 1.6) or monitoring synovitis.8 Neovascularity has been correlated with pain in tendinopathy (although the relationship between tendinopathy and neovascularity is controversial) and with active synovitis in inflammatory joint disease. Power Doppler is usually employed using low pulse repetition frequency, medium persistence, small color box, low wall filter, and appropriate color velocity scale. Doppler signal (Fig. 1.7) may be reduced or abolished by pressing too hard or if a tendon is under tension; therefore, a light touch should be employed and tendons should be relaxed while being examined.
The role of contrast-enhanced ultrasound (CEUS) is yet to be established. However, CEUS improves diagnostic
sensitivity in inflammatory joint diseases, shows areas of relatively low vascularity that might predispose to tendinopathy, and demonstrates age-related changes in vascularity in the rotator cuff.9,10
sensitivity in inflammatory joint diseases, shows areas of relatively low vascularity that might predispose to tendinopathy, and demonstrates age-related changes in vascularity in the rotator cuff.9,10
Elastography (Fig. 1.8) assesses tissue softening by measuring tissue displacement before and after compression, and has shown promising results in epicondylitis at the elbow and in Achilles tendinopathy.1,11,12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree