Introduction to Chest Radiography
Chest Radiography
Radiographic examination of the chest plays an important role in the diagnosis and management of pulmonary disease.1 Chest radiographs account for the majority of radiographs taken each year. Chest radiography plays a less dominant but no less important clinical role in chiropractic practice. Although limitations exist, when combined with a thorough history and physical examination, chest radiography offers a sensitive method for detecting serious pathology of the thorax.
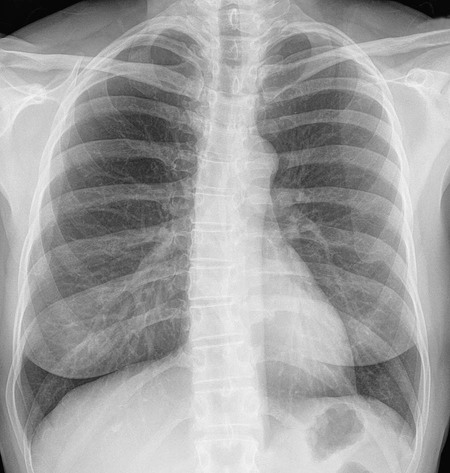
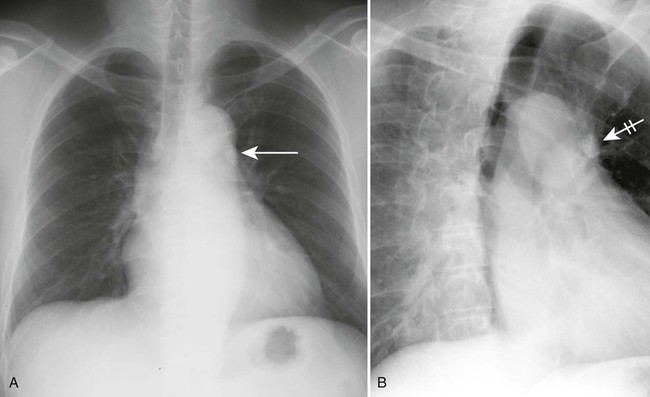
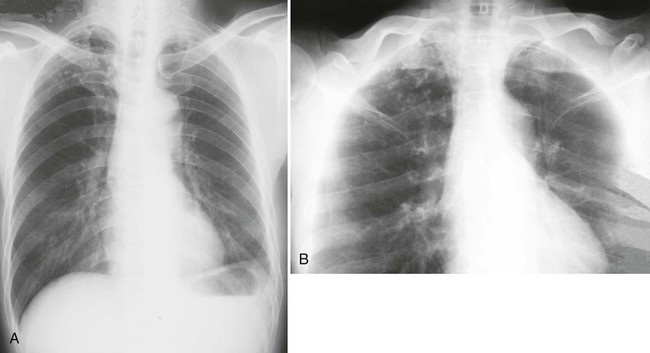
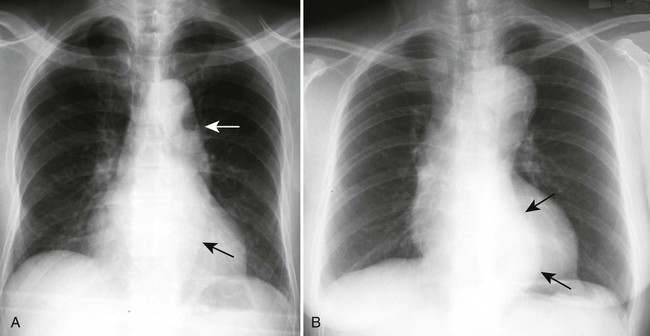
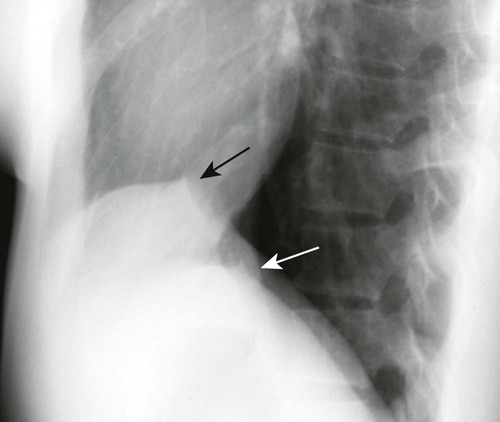
The standard radiographic examination of the chest consists of a posteroanterior (PA) and right or left lateral projection (Figs. 21-1 and 21-2). Oblique, lateral decubitus, and apical lordotic views are some of the more helpful accessory views that may augment the standard views (Figs. 21-3 and 21-4). The lateral projection adds little as a screening procedure in younger patients.11 Consequently, the PA projection alone generally is accepted as adequate screening of the thorax in young individuals who are without symptoms directly referable to the chest. All patients older than 40 years of age and patients of any age who exhibit clinical findings directly referable to the chest should have both a PA and lateral projection radiograph taken during routine evaluation.
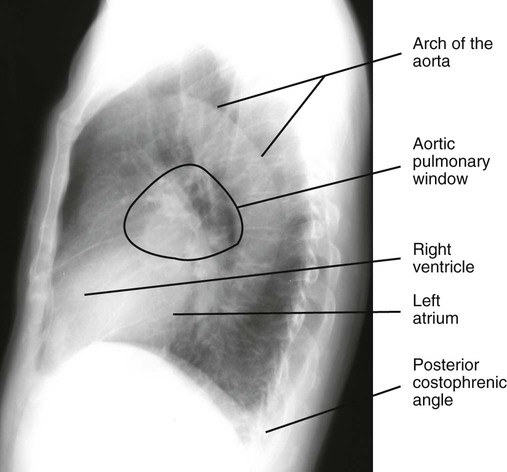
Because the side of the body closest to the film is demonstrated with better detail and much of the left lung is obscured by the heart in the frontal projection, the left side of the body is customarily positioned next to the film in the lateral projection.4 However, if pathology is known or suspected on the right, then the right side of the patient is placed next to the film to exhibit the area of concern with better detail.
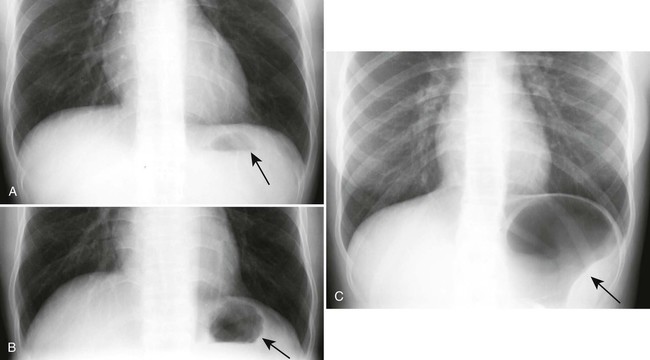
Chest radiography uses high peak kilovoltage (110–150 kVp) exposures during full patient inspiratory effort, with a focal-film distance of 72 inches. In the frontal projection, rotation is present if the clavicles are not equidistant from the patient’s midline. Although individual preferences exist, a properly exposed chest radiograph should barely outline the thoracic spine through the heart shadow. The radiograph should display the entire thorax and, importantly, the costophrenic angles on the film. Good patient inspiratory result is noted by observing the posterior portions of the first 10 ribs (or anterior portions of the first seven ribs) above the right hemidiaphragm. The right hemidiaphragm is used as a reference because the position of the left hemidiaphragm is more variable because of the subjacent gastric air bubble. Diagnostic purposes sometimes warrant taking films during patient expiration. For instance, if a “check-valve” bronchial obstruction is present, the involved lung demonstrates a pathologic state in which it remains well inflated on an expiration film.
The criteria for ordering chest films vary and often are individualized at the personal, departmental, or institutional level. Some of the more common indications include chronic cough; hemoptysis; expectoration; shortness of breath; cyanosis; clubbing of the fingers; and pain in the chest, thoracic spine, or upper extremities. Routine chest radiographs in an otherwise healthy patient population are discouraged. However, when these baseline films are available, they offer valuable comparative studies for equivocal radiographic findings on subsequent studies. Often patients exhibit residua of an old or inactive disease, such as healed granulomas, chronic obstructive pulmonary disease, and pulmonary scarring. Frequently, the availability of old films for comparison may eliminate the need for continued evaluation, limiting further cost and patient exposure. Likewise, practitioners should apply serial radiographs cautiously when following a disease process and then only at large enough intervals that overirradiation does not become an issue.
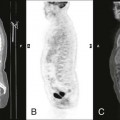
Many times it is necessary to augment the information gathered from the chest radiographs with other imaging modalities to more completely evaluate the patient. Fluoroscopy is an often overlooked but valuable procedure for localizing pulmonary nodules and evaluating diaphragmatic movement. Computed tomography (CT) is the most useful additional procedure and has all but replaced conventional tomography. CT is particularly advantageous when shadows of the chest wall, pleura, lung, hilum, or mediastinum should be better visualized when partially obstructed by overlying densities. CT is most widely used to delineate and assess neoplastic disease.
Magnetic resonance imaging (MRI) is most often used to distinguish pathology of the hilar and mediastinal lymph nodes from adjacent vascular anatomy. It has a particular advantage over CT for distinguishing mediastinal lymph node involvement from vascular masses because flowing blood has no signal on MRI and therefore appears black, readily distinguishing vessels from the high signal intensity of the lymph nodes. The ventilation and perfusion scans of lung scintigraphy are valuable in diagnosis of pulmonary embolism, although the more invasive pulmonary angiography remains the imaging standard for questionable scan results.
Although imaging examinations are valuable in the study of intrathoracic disease, they do not supplant the importance of a thorough physical examination and history. In addition, blood tests, diagnostic skin tests, sputum cultures, biopsy, and especially bronchoscopy have the ability to add a unique information perspective to the diagnostic case. The clinician is cautioned to recognize the limitations of imaging and the unique benefits provided by other diagnostic studies.
Anatomy
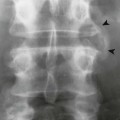
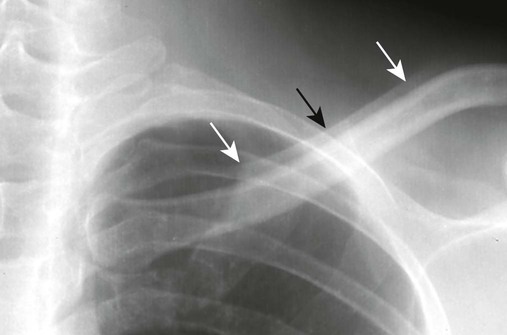
Selected normal structures on PA and lateral chest radiographs are identified in the normal anatomy chapter of this book (see Chapter 6). Some common variants and misinterpretations are presented in Figures 21-5 to 21-10. The bony thorax consists of 12 thoracic vertebrae, 12 pairs of ribs with costal cartilages, and the sternum. The scapulae and clavicles are superimposed over the thorax on the PA chest radiograph. Individual muscles of the thorax generally are not discernible on radiographs. However, absence of large muscles, such as the pectorals, appears as a region of decreased density. The intercostal arteries, veins, and nerves pass along the inferior border of the ribs; enlargements of these structures may cause a characteristic erosion deformity of the inferior rib margin.


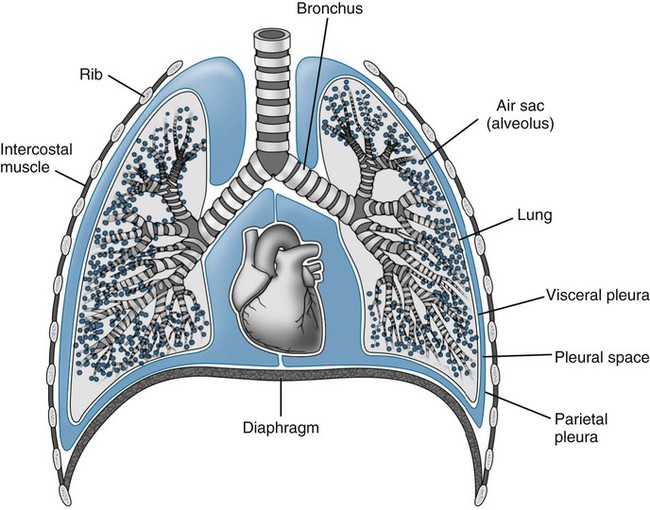
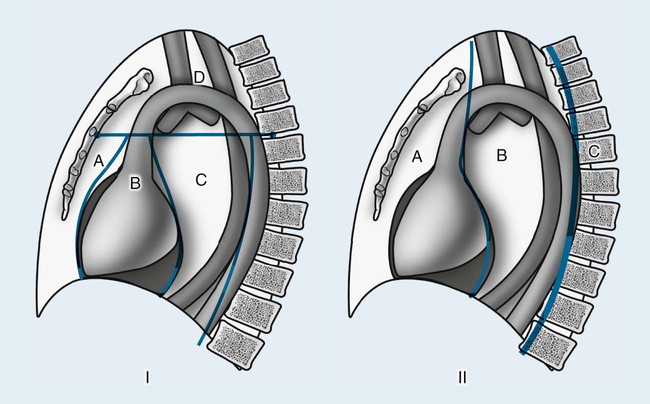
The thoracic cavity is divided into two pleural cavities surrounding a centrally located mediastinum (Fig. 21-11). The mediastinum is divided into four anatomic (superior, anterior, middle, and posterior) or three radiographic (anterior, middle, and posterior) areas, as depicted in Figure 21-12. The heart, great vessels, esophagus, thymus, and lymph tissues are all important structures contained within the mediastinum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree