Introduction to Digital Radiography and PACS
Objectives
On completion of this chapter, you should be able to:
• Define the term digital imaging.
• Explain latent image formation for conventional film/screen radiography.
• Explain what a picture archiving and communication system (PACS) is and how it is used.
• Define digital imaging and communications in medicine (DICOM).
Key Terms
Digital imaging
Direct capture digital radiography
Flat panel detector (FPD)
Indirect capture digital radiography
Photostimulable phosphor (PSP) image capture
Teleradiology
This chapter is intended to present a brief overview of digital imaging and the picture archiving and communication system (PACS); both topics are covered in depth in the chapters that follow. This chapter also presents several basic definitions, compares and contrasts digital and analog imaging, and discusses the historic development of both digital image capture and PACS. It is important to grasp the basic definitions and concepts before moving to the more involved topics because this information will be useful throughout the textbook. Bear in mind that the major focus of this text is on entry-level radiography. Although advanced modalities such as magnetic resonance imaging (MRI), computed tomography (CT), and others may be touched on, this text will not dig deeply into those areas.
Conventional Film/Screen Radiography
Before defining and discussing digital imaging, a basic understanding of conventional film/screen imaging must be established. Conventional radiography uses film and intensifying screens in its image formation process. Film is placed on one or between two intensifying screens that emit light when struck by x-rays. The light exposes the film in proportion to the amount and energy of the x-rays incident on the screen. The film is then processed with chemicals, and the manifest image appears on the sheet of film. The film is taken to a radiologist and placed on a lightbox for interpretation. For further review of how conventional radiographic images are created, please consult a radiographic imaging textbook for a more in-depth explanation of this process.
Digital Imaging
Digital imaging is a broad term. This type of imaging is what allows text, photos, drawings, animations, and video to appear on the World Wide Web. In medicine, one of the first uses of digital imaging was with the introduction of the CT scanner by Godfrey Hounsfield in the 1970s. In the decades since, all of the other imaging modalities have become digital.
The basic definition of digital imaging is any imaging acquisition process that produces an electronic image that can be viewed and manipulated on a computer. Most modern medical imaging modalities produce digital images that can be sent through a computer network to various locations.
Historical Development of Digital Imaging
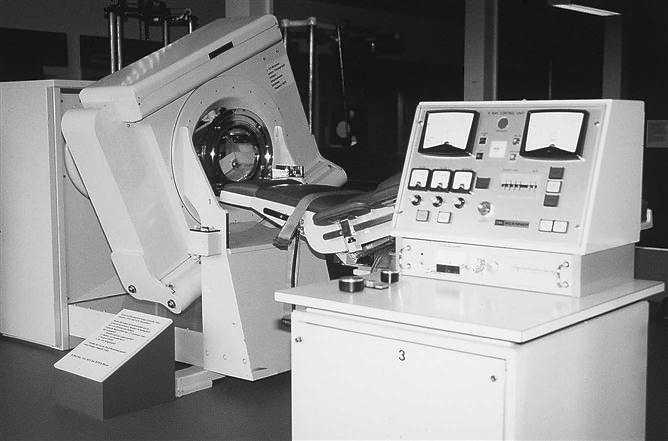
CT is second only to the discovery of the x-ray as a major milestone in medical imaging. CT brought about the coupling of the computer and imaging devices. The earliest CT unit built by Hounsfield took several hours to acquire a single slice of information. The machine then took a few days to reconstruct the raw data into a recognizable image. The first commercial CT scanners built were made to image the head only. Figure 1-1 shows one of the early CT scanners built for imaging the head.
MRI was introduced commercially for health care use in the early 1980s. Several companies began pioneering efforts in the mid to late 1970s after the publication of an article by Paul Lauterbur in 1973. Many scientists and researchers were involved in the development of the MRI as we know it today.
Fluoroscopy saw many advances during the 1970s as well thanks to developments in computer technology. Analog-to-digital converters (ADCs) made it possible to capture the images digitally; Plumbicon or Vidicon TV tubes allowed for the display of the dynamic (real-time) image on a television monitor in higher resolution and made it possible to store the frames digitally on a computer. Ultrasound and nuclear medicine were easy converts to the digital world early on because the images created in these modalities were simply frame-grabbed (the current image on the screen is captured and sent as an image file) and converted to a digital image.
Digital Radiography
The concept of moving images digitally was introduced by Albert Jutras in Canada during his experimentation with teleradiology (moving images via telephone lines to and from remote locations) in the 1950s. Early PACSs were developed by the U.S. military in an effort to move images among Veterans Administration (VA) hospitals and to send battlefield images to established hospitals. These strides were taking place in the early to mid 1980s, and without the government’s participation, this technology would not be where it is today. To provide the PACS a digital image, early analog radiographs were scanned into a computer (digitized) so that the images could be sent from computer to computer. The inherently digital modalities were sent via a PACS first, and then as projection radiography technologies advanced, they joined the digital ranks.
Photostimulable Phosphor
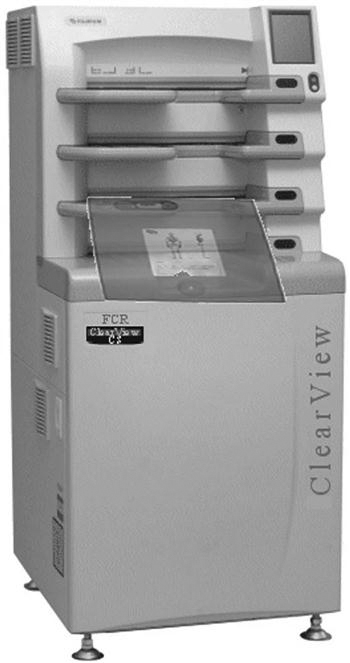
Photostimulable phosphor (PSP) image capture (previously known as computed radiography [CR]), is the digital acquisition modality that uses storage phosphor plates to produce projection images. To avoid possible confusion resulting from use of the term computed, the technology related to this type of system will be referred to as PSP because the newer systems may or may not be cassette based. PSP imaging can be used in standard radiographic rooms just like film/screen. The only new equipment that is required is the PSP and phosphor plates, the PSP readers, the technologist quality control workstation, and a means to view the images, which can be either a printer or a viewing station (Figure 1-2).
The storage phosphor plates are similar to our current intensifying screens. The biggest difference is that the storage phosphors can store a portion of the incident x-ray energy in traps within the material for later readout. More is presented on this topic in Chapter 4.
PSP imaging was first introduced commercially in the United States in 1983 by Fuji Medical Systems of Japan (Figure 1-3). The first system consisted of a phosphor storage plate, a reader, and a laser printer to print the image onto film. PSP imaging did not take off very quickly because many radiologists were reluctant to embrace the new technology. In the early 1990s, PSP imaging began to be installed at a faster rate because of the technological improvements that had occurred in the decade since its introduction. Several major vendors have PSP systems installed in hospitals throughout the United States.
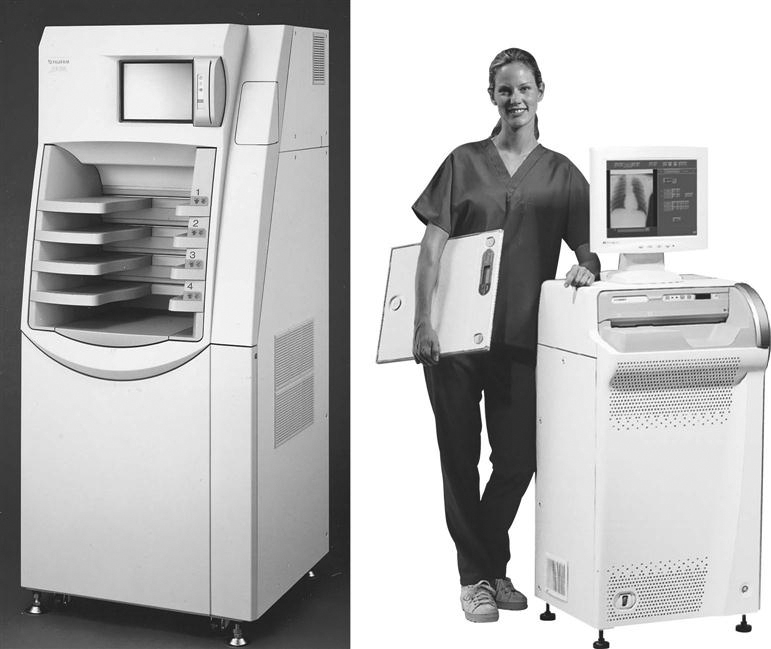
A, A high-volume reader capable of processing between 110 and 140 imaging plates per hour. B, A much smaller system designed for medical offices, surgery, or intensive care units, capable of processing 50 to 60 imaging plates per hour. (A, from Ballinger: Merrill’s atlas, ed 10, St. Louis, 2003, Mosby; B, courtesy FUJIFILM Medical Systems USA, Inc.)
Flat Panel Detectors
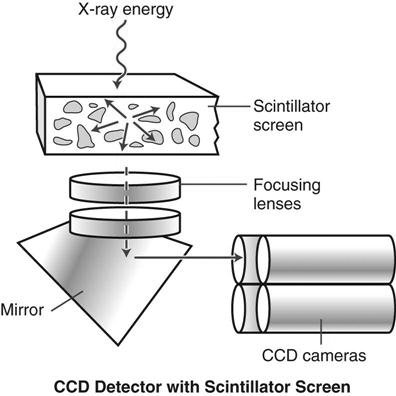
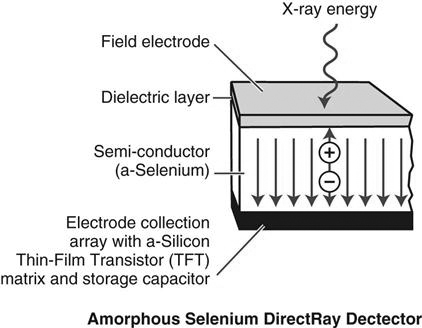
Most flat panel detector (FPD) systems use an x-ray absorber material coupled to a thin film transistor or a charge-coupled device (CCD) to form the image. Therefore an existing x-ray room needs to be retrofitted with these devices if a new FPD, TFT, or CCD room is not installed (Figure 1-4).
FPD can be divided into two categories: indirect capture and direct capture. Indirect capture digital radiography devices absorb x-rays and convert them into light. The light is then collected by an area-CCD or thin-film transistor (TFT) array and then converted into an electrical signal that is sent to the computer for processing and viewing (Figure 1-5). Direct capture digital radiography devices convert the incident x-ray energy directly into an electrical signal, typically using a photoconductor as the x-ray absorber, and send the electrical signal to a TFT and then to an ADC. The ADC signal goes to the computer for processing and viewing (Figure 1-6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree