| SKULL BASE REGION | Jugular foramen |
| HISTOPATHOLOGY | N/A |
| PRIOR SURGICAL RESECTION | No |
| PERTINENT LABORATORY FINDINGS |
|
Case description
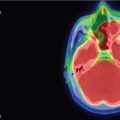
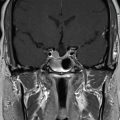
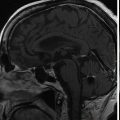
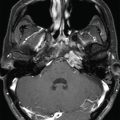
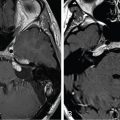
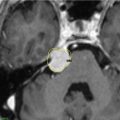
The 19-year-old patient was evaluated for left-sided pulsatile tinnitus and intermittent aural fullness as a teenager and found to have multiple paragangliomas (left jugular paraganglioma, bilateral carotid body paragangliomas, and right vagal paraganglioma) associated with familial paraganglioma syndrome (SDHD mutation) ( Figure 10.50.1 ). Initial examination did not reveal cranial neuropathies, and the patient exhibited normal hearing bilaterally. Given the large size of the left jugular paraganglaioma and the right vagal paraganglioma, which could threaten the contralateral vagus nerve, the decision was made to proceed with upfront stereotactic radiosurgery (SRS) of the left jugular paraganglioma ( Figure 10.50.2 ).
| Radiosurgery Machine | Gamma Knife |
| Radiosurgery Dose (Gy) | 16 at the 50% isodose line |
| Number of Fractions | 1 |


| Critical Structure | Dose Tolerance |
|---|---|
| Brainstem | 15 Gy maximum point dose |
| Internal carotid artery in canal | Unknown dose tolerance |
| Cochlea | 4 Gy maximum point dose (extrapolated from vestibular schwannoma literature) |
| Lower cranial nerves in foramen | Unknown dose tolerance |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree