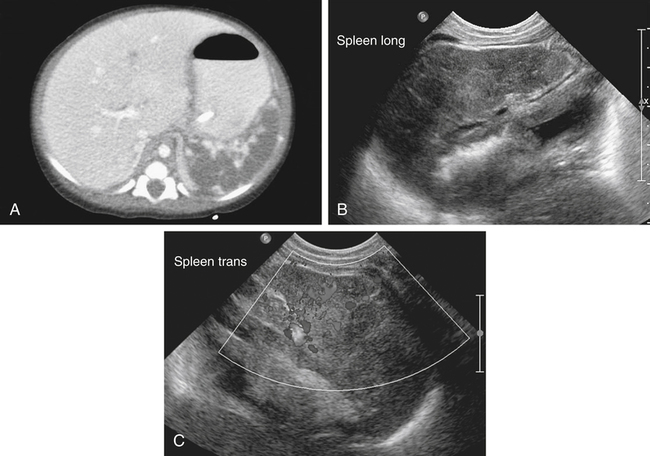
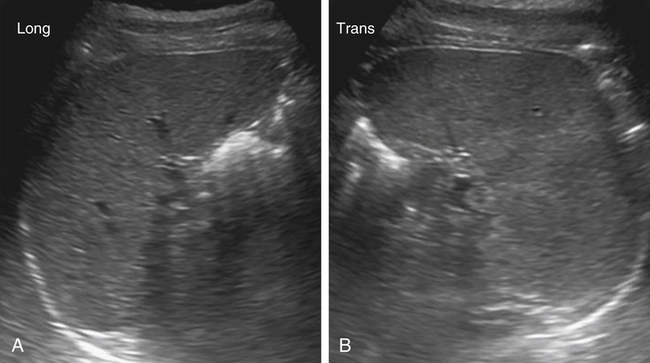
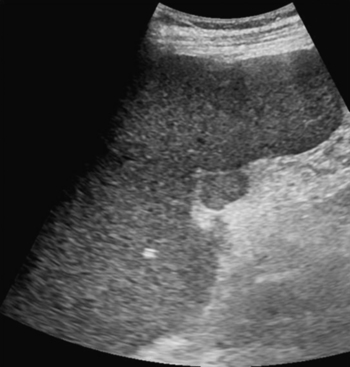
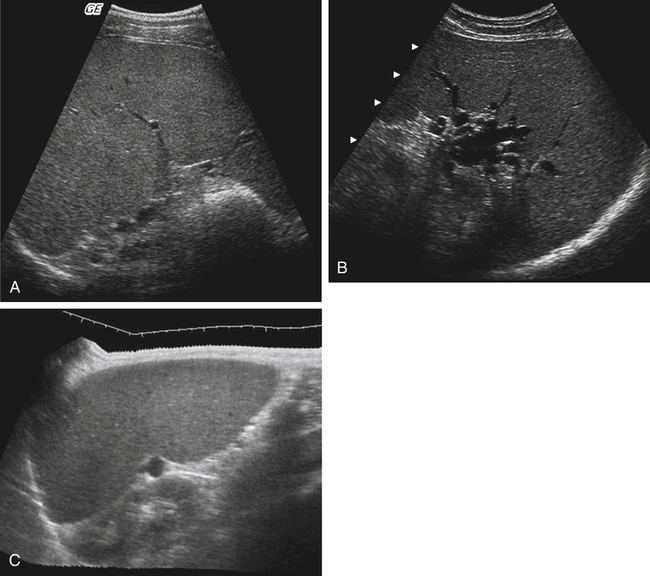
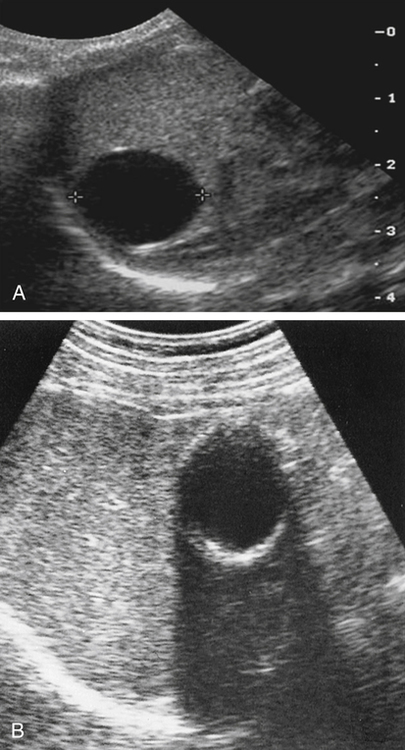
• List the basic anatomy and physiology of the spleen. • Describe the sonographic appearance of a normal spleen. • List the congenital variants of the spleen that may occur, and describe the associated sonographic appearances. • List the causes of splenomegaly. • Describe the most common benign splenic neoplasms. • Identify the sonographic findings associated with blunt trauma to the spleen. • Define the most common malignant splenic neoplasms. • Differentiate between the sonographic appearances of benign and malignant neoplasms. • List the causes of splenic infarct. • Identify Doppler findings associated with specific splenic anomalies. Lying between the ninth and eleventh left rib, the spleen is best visualized with the patient lying supine or in the left lateral decubitus position and scanning from the coronal plane. A midfrequency small footprint transducer is used. The normal sonographic appearance of the spleen is a homogeneous, comma-shaped or bean-shaped organ, with an echogenicity similar or slightly hyperechoic to the liver and equal to or slightly hyperechoic to the renal parenchyma (Fig. 8-2). Splenic size varies based on age, gender, and height; however, a length of 12 cm is considered to be at the upper limit of normal.1 Accessory spleen, or splenunculus, is the most common congenital anomaly affecting the spleen, occurring in approximately 10% of the population.2 This variant is most commonly singular and located in the splenic hilum, although it may be located elsewhere in the abdomen, with a small percentage being multiple (spleniculi). The presence of an accessory spleen is usually insignificant, but accessory spleens may rarely undergo torsion or infarction; affected patients present with acute LUQ pain. Clinical symptoms should also be considered in differentiating between probable accessory spleens, neoplasms, and lymphadenopathy, which may have a similar sonographic appearance. Asplenia is diagnosed through the absence of the splenic tissue after careful evaluation of the entire abdomen to exclude wandering spleen. The diagnosis of polysplenia can be made when multiple small spleens are identified in the LUQ (Fig. 8-4). Additional imaging of the abdomen, heart, and lungs aids in the diagnosis of asplenia or polysplenia-associated complex. Splenomegaly, or enlargement of the spleen, is one of the most common anomalies of the spleen encountered by sonographers. Numerous causes of splenomegaly exist; congestive etiologies associated with portal hypertension are the most common (Fig. 8-5, A and B). Other causes include infection, hematologic disorders, immunologic disorders, trauma, neoplasia, vascular anomalies, and storage diseases. In addition to clinical symptoms associated with the underlying disease, patients with splenomegaly may have LUQ pain. With the detection of a cyst in the LUQ, sonographic examination can be useful in identifying the origin of the cyst—arising in the spleen or arising from adjacent organs such as the adrenal gland, gastrointestinal tract, or a pancreatic pseudocyst extending into the spleen (see Chapter 4). Laboratory tests and patient history may also aid in the differentiation of cyst origin. Cysts arising in the spleen may be classified as primary or true cysts, when they have an epithelial or endothelial lining, or secondary (pseudocysts), resulting from trauma, infection, or degeneration. Cysts in the spleen are uncommon and are usually benign. Splenic cysts may be identified on sonograms in asymptomatic patients as an incidental finding, although patients may have symptoms related to the cyst size or origin and may have LUQ pain. Sonographically, a cyst should appear as a well-defined, round or ovoid, thin-walled, anechoic lesion that shows acoustic enhancement (Fig. 8-6, A). Cysts associated with infection or trauma may show calcification of the cyst wall (Fig. 8-6, B). Cysts may also show fluid-debris levels from purulent material or hemorrhage. Splenic cysts are rare; in the absence of the classic sonographic features of a cyst, additional imaging or clinical follow-up is indicated to exclude neoplasm.
Left Upper Quadrant Pain
Spleen
Normal Sonographic Anatomy
Variants and Congenital Anomalies
Accessory Spleen
Asplenia and Polysplenia
Sonographic Findings

Splenomegaly
Cysts
Sonographic Findings
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Left Upper Quadrant Pain