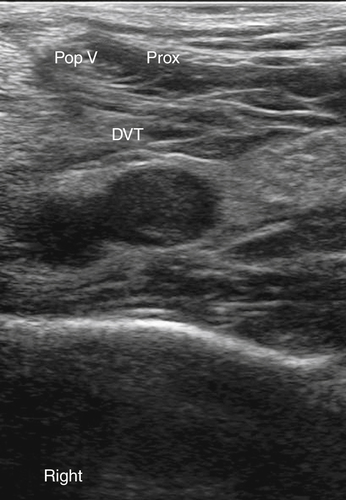
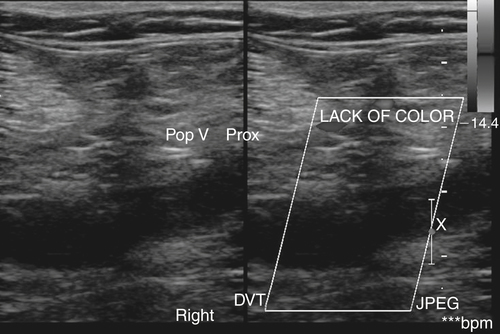
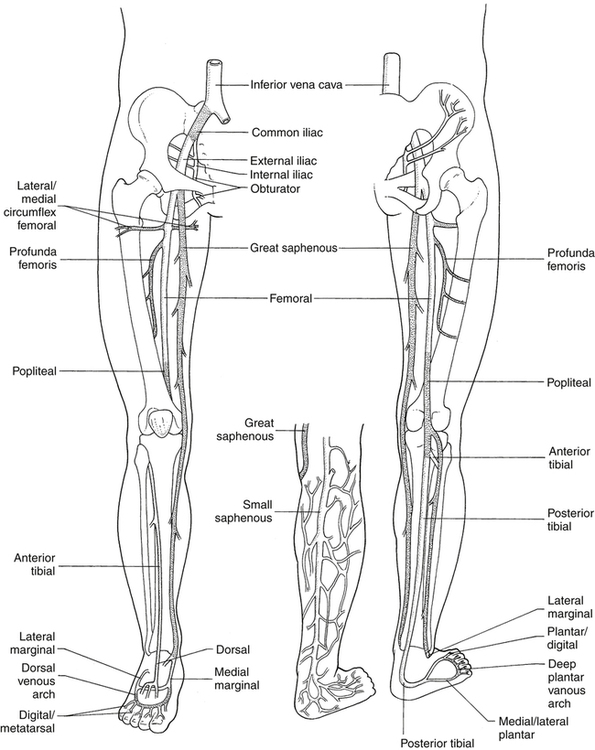
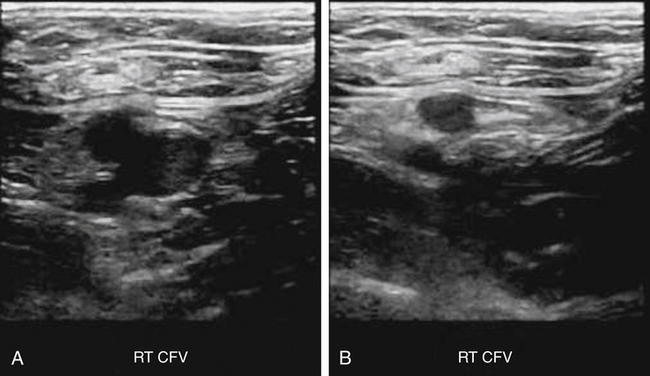
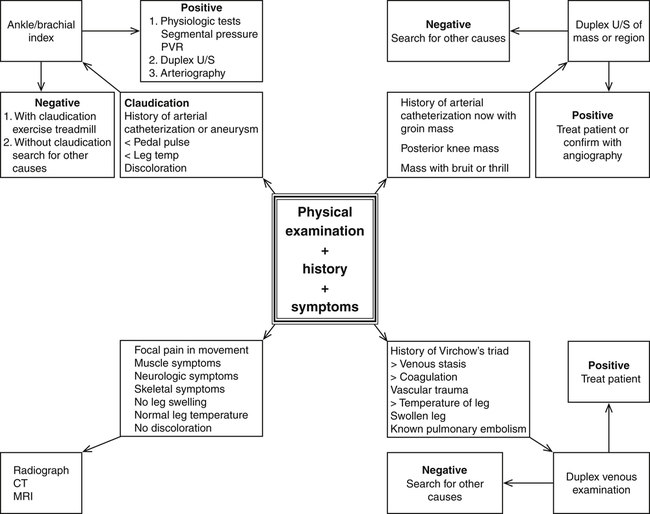
• Differentiate between the various causes of leg pain. • Describe the sonographic appearance of thrombosis of the deep venous system. • Discern the various sonographic appearances of acute and chronic thromboses. • Explain the differential diagnoses of deep vein thrombosis (DVT). • Describe the physiologic changes to the venous system that help in the diagnosis of DVT. • Explain the treatment options for DVT. • Differentiate between acute and chronic venous thrombosis. This chapter describes a variety of causes of leg pain, especially causes secondary to venous disease, and the role of sonography in diagnosis of these diseases. Protocols may vary depending on whether these examinations are performed in a radiology-based sonography department versus a dedicated vascular laboratory. This chapter focuses more on the protocols followed in a radiology department. A brief explanation of normal anatomy is included (Fig. 35-3 and Box 35-1), but the focus is on the pathology and diseases that lead to leg pain. The radiology-based sonography department concentrates primarily on the diagnosis of deep vein thrombosis (DVT) and posterior knee masses. B-mode and Doppler evaluation in the vascular laboratory can be quite useful in diagnosis of venous causes of leg pain. Bony fractures; tendinous sprains; ligamental ruptures and tears; muscle strains, tears, and ruptures; nerve impingement; and trauma are the most common sources of lower extremity pain. However, these diagnoses are left to plain film radiography, CT, and magnetic resonance imaging (MRI). Figure 35-4 shows how a physician would decide which imaging examination would best assess the patient’s condition based on history, symptoms, and physical examination. Starting at the iliac bifurcation, the veins are listed in a retrograde order (see Fig. 35-3). The two common iliac vessels branch into the inferior vena cava (IVC) and from the aorta at the level of the umbilicus. They continue to the level of the sacroiliac joints before the internal iliac (hypogastric) veins angle steeply into the pelvis draining the rectum, sigmoid, and genitals. After the internal iliacs have departed, the external iliac vein proceeds along the lateral wall of the pelvis before leaving the pelvis at the inguinal canal. After passing the inguinal ligament, the vein is called the common femoral vein (CFV). After about 4 cm, the CFV is joined by the greater saphenous vein (GSV) from an anterior medial direction. The area where the GSV becomes confluent with the CFV is known as the saphofemoral junction (SFJ). Within a few centimeters of the SFJ, the CFV branches into the femoral vein and the deep femoral vein. The deep femoral vein is also called the profunda femoris, or simply the profunda. The profunda serves the upper lateral thigh. The femoral vein continues along the anterior medial leg until it dives deep through the ligaments of the adductor muscles, known as the adductor hiatus or Hunter’s canal. The popliteal vessels are located in the popliteal fossa and can quickly start branching into other veins of various sizes, known as the trifurcation area. From the popliteal vein, moving inferiorly, the sonographer should be able to visualize the tibioperoneal trunk, from which the anterior tibial vein and peroneal (fibular) vein arise. The trifurcation is found a little more inferior after those two vessels separate. The trifurcation consists of the anterior and posterior tibial veins and the peroneal veins. Located posterior to the trifurcation are the gastrocnemius vessels. These are not usually evaluated unless they appear dilated and prominent, or the patient has pain in that area. The trifurcation should be identified by following it from the popliteal, so as to avoid mistaking it for the more posterior gastrocnemius vessels (Fig. 35-5). The anterior tibial vessels branch off anteriorly and laterally, passing through the space formed between the tibia and fibula then laterally to the tibial shaft with a single artery and paired veins. The popliteal continues for a few centimeters before the peroneal (fibular vessels) and posterior tibial veins branch off. The peroneal vessels run deeper and more laterally with a single artery and paired veins, and the posterior tibials (one artery and two paired veins) continue more medially and superficially, down to the area just posterior to the medial malleolus. Numerous assessments are useful in determining whether an extremity vessel is an artery or a vein. • The arteries maintain a round shape when viewed in cross section. • The veins change shape with patient respirations. • The veins compress much more easily than arteries. • The veins are ovoid unless distended. • The arteries pulsate with each heartbeat. • The veins dilate during a Valsalva maneuver or when the patient’s trunk is elevated in relation to the extremity. • The vein has the potential of being larger than the accompanying artery. In a thrombus-filled state, it is larger; but in a healthy patient, it may appear slightly smaller. Normal veins should appear anechoic on gray-scale imaging, be easily compressed (Fig. 35-6), show intraluminal color Doppler, and be able to demonstrate a distal augmentation on pulsed wave Doppler. On pulsed wave Doppler, the sonographer should be able to appreciate the spontaneous flow and the respiratory phasicity. Normally, when a patient inspires, that pushes the diaphragm inferiorly, increasing intraabdominal pressure on the IVC. Given that the IVC collapses during inspiration, the same occurs distally within the veins of the lower extremity. When the patient expires, that pressure is relieved, and venous flow can resume. If the venous valves are competent, that can also be demonstrated by pulsed wave Doppler by having the patient perform the Valsalva maneuver, or the sonographer can perform a proximal compression. If either technique works to cut off the Doppler signal, the valves are considered competent. Pulmonary embolism has a high rate of morbidity and mortality (600,000 hospitalizations and 200,000 deaths each year).1 The primary source of pulmonary embolism is thrombosis of the deep venous system in the lower extremities. The primary symptom of DVT of the lower extremity is a painful, swollen leg. Duplex sonography is accurate in determination of the presence or absence of venous clot. The advantages of sonography over venography in diagnosing a DVT include better patient tolerance, similar accuracy, lower risk, and lower cost. The current “gold standard” to diagnose a pulmonary embolus is pulmonary angiography. Because it is associated with a high risk of morbidity and mortality, other, less invasive and lower risk modalities usually are used for diagnosis. A nuclear medicine ventilation-perfusion scan can be performed to detect circulation of air and blood within a patient’s lung, and CT angiography of the chest can detect a pulmonary embolus. Although sometimes large emboli can be seen in the heart during an echocardiogram, sonography does not usually evaluate the presence of pulmonary emboli directly. Sonography is useful to help identify the location of the origin of the embolus and to help determine the effectiveness of thrombolytic therapy. When DVT in the lower extremity is the culprit, the origin often can be identified; however, any vein can have a DVT and embolization of the thrombus can occur, such as a central vein that is not easily seen on sonography, so not every patient with a pulmonary embolus has a positive DVT in the lower extremity.1 Certain patient populations are at increased risk for development of thrombosis in the legs. Blood that is not moving tends to clot. The combined factors of muscle contraction and venous valve action and the effects of respiration propel venous blood in the extremities. Any event that immobilizes the leg (trauma, surgery, advanced age, obesity, prolonged sitting), damages the deep venous valves (varicose veins, venous insufficiency, progression of superficial vein thrombosis [SVT]), increases a patient’s coagulability (oral contraceptive use, coagulation disorders, recent surgery, cancer), or decreases natural flow pressures (congestive heart failure [CHF]) increases the possibility of venous thrombosis. The three primary factors that lead to venous thrombosis—vessel damage, flow stasis, and hypercoagulability—are known as Virchow’s triad. The most prominent part of Virchow’s triad is venous stasis. If the erythrocytes stagnate for too long, natural clotting factors take effect and begin to clot, or stick together. This sticky lump of erythrocytes can be seen on sonographic evaluation. They appear as a swirling mobile hypoechoic mass, termed “rouleau formation.” Rouleau, a French term, means “coil” or “roll,” which is how the cells begin to appear as they all clump together—a roll. Rouleau formation is a precursor to a thrombosis. The vein fully compresses, and Doppler signals appear normal, but note should be made that slow-moving blood flow was seen.2,3 The patient should be positioned with the trunk slightly elevated, as in a reverse Trendelenburg position, with the lower extremity slightly rotated outward. Some experts suggest having the patient dangle the affected leg during examination of the calf vessels. The sonographer should start high in the groin crease, documenting the common femoral artery and CFV. The sonographer can use the SFJ or the origin of the GSV and move superiorly to begin scanning correctly in the CFV. If imaging inferior to the SFJ, the femoral vein is seen. Spectral Doppler of the veins should demonstrate phasic flow that varies with respiration, augmentation, and Valsalva maneuver. If the patient’s trunk is elevated, the vein appears distended, but there should be no evidence of thrombus within the vein. When moderate probe pressure is increased, the walls of the vein should fully coapt. Probe pressure is adequate if the accompanying artery begins to deform. (This maneuver must be done in a transverse plane and should not be done with the transducer in a longitudinal plane because it is too easy to slide off the side of the vessel in the longitudinal plane).4 The sonographer should begin moving inferiorly on the leg at close intervals to confirm the absence of intraluminal echogenic material, the continuation of phasic flow that varies with respiration, and coaptation of the vein walls. Doppler analysis can be helpful in documenting thrombus that has progressed to a size that can interrupt flow. Doppler signals that show a continuous flow pattern or lack of increased flow during distal augmentation suggest flow-restricting thrombus. If the pulsed wave Doppler demonstrates a dampened, monophasic waveform, that suggests a proximal stenosis. The most common reason for a monophasic waveform seen in an entire unilateral lower extremity is venous thrombosis in the ipsilateral iliac veins. Other causes for a monophasic waveform down an entire lower extremity include a partial thrombus in a more proximal vein; extrinsic compression, such as a fluid collection, mass, pregnancy, or ascites; intrinsic luminal narrowing owing to a hypoplastic vein; or prior thrombus. However, bilateral dampened waveforms mean that there is an issue of obstruction at the level of the IVC.4 Imaging hints include the following: • Keeping the focal zone at the level of the vessel being viewed • Imaging the vessel from an approach that is closest to the skin for that vessel at that level • Keeping the vessel in the middle of the transducer face • Carefully adjusting the gain so that soft internal plaque is visualized and not “blacked out” by incorrect gain settings • Changing the sonographic window if a compression cannot be completed because a ligament may make compression difficult
Leg Pain
Normal Vascular Anatomy
Artery or Vein?
Normal Sonographic Appearance
Venous Disease
Deep Vein Thrombosis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine