Presentation and Presenting Images
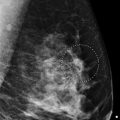
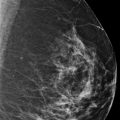
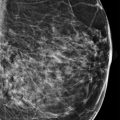
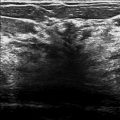
( ▶ Fig. 56.1, ▶ Fig. 56.2, ▶ Fig. 56.3, ▶ Fig. 56.4)
A 65-year-old female with a history of right breast cancer treated 6 years ago presents for screening mammography.
56.2 Key Images
( ▶ Fig. 56.5, ▶ Fig. 56.6, ▶ Fig. 56.7, ▶ Fig. 56.8, ▶ Fig. 56.9, ▶ Fig. 56.10)
56.2.1 Breast Tissue Density
The breasts are heterogeneously dense, which may obscure small masses.
56.2.2 Imaging Findings
There are grouped linear calcifications in the left breast at the 9 o’clock location in the posterior depth ( ▶ Fig. 56.7 and ▶ Fig. 56.9; DBT images ▶ Fig. 56.5 and ▶ Fig. 56.6). The synthetic mammogams can enhance the appearance of calcifications due to the reconstruction algorithms. In addition, the contrast on the synthetic mammograms is diminished, with the background fibroglandular tissue appearing more flat and thus the calcifications standing out further ( ▶ Fig. 56.8 and ▶ Fig. 56.10). A single stable coarse calcification is seen in the left breast; otherwise no other calcifications of concern are seen.
56.3 BI-RADS Classification and Action
Category 0: Mammography: Incomplete. Need additional imaging evaluation and/or prior mammograms for comparison.
56.4 Diagnostic Images
( ▶ Fig. 56.11, ▶ Fig. 56.12, ▶ Fig. 56.13, ▶ Fig. 56.14, ▶ Fig. 56.15)
56.4.1 Imaging Findings
The diagnostic imaging confirms the segmental fine linear pleomorphic calcifications spanning an area of 0.8 × 3.2 × 0.8 cm at 10 o’clock in the middle depth ( ▶ Fig. 56.14). The craniocaudal (CC) view tomosynthesis also suggests that there may be an asymmetry associated with the more coarse calcification ( ▶ Fig. 56.5). This is also suggested on the CC spot magnification image ( ▶ Fig. 56.14). A correlate is not seen on the mediolateral oblique (MLO) images likely due to being obscured by the dense overlapping tissue. If further evaluation was required, a spot digital breast tomosynthesis (DBT) could have been performed; however, this area was already assessed as needing a biopsy. The area of segmental calcifications underwent stereotactic biopsy. The specimens from the posterior extent of this area are shown in ▶ Fig. 56.15.
56.5 BI-RADS Classification and Action:
Category 5: Highly suggestive of malignancy
56.6 Differential Diagnosis
Grade 2 invasive ductal carcinoma (grade 2 IDC) with intermediate grade ductal carcinoma in situ (DCIS): Invasive cancers can present as calcifications. On pathologic assessment, the IDC measured 7 mm. In this case, there is a suggestion of an asymmetry on DBT. However, if this asymmetry was not associated with the calcifications, it likely would not have been of interest in recalling the patient.
Ductal carcinoma in situ (DCIS):The morphology and linear distribution of these calcifications is highly suspicious for DCIS. This would be a concordant image-guided biopsy result.
Atypical ductal hyperplasia (ADH): A biopsy of these calcifications yielding ADH would likely be upgraded to DCIS or IDC.
56.7 Essential Facts
The calcifications in this case are easily seen on the conventional mammogram. The DBT imaging may have alerted the reader to a possible asymmetry associated with the calcifications. This observation led to performing biopsies at the extent of the calcifications to possibly identify an associated invasive component.
The diagnosis of an invasive component of a breast cancer will dictate and influence the surgical and oncological treatment.
Early studies suggest that the synthetic mammogram (a two-dimensional mammogram constructed from DBT images) combined with DBT images is comparable to full-field digital mammography (FFDM) alone or in combination with DBT.
56.8 Management and Digital Breast Tomosynthesis Principles
The elimination of the routine FFDM during routine mammography, substituting a synthetic mammogram, will decrease the radiation exposure.
It is estimated that using the synthetic two-dimensional (2D) images has an estimated dose reduction of 45% compared to a FFDM plus DBT.
There is a significant learning curve for radiologists to add DBT image interpretation to FFDM interpretation. There will be an additional learning curve for the radiologist if and as they convert from the use and interpretation of FFDM to that of synthetic 2D mammograms. Training for this needs to be developed.
There is not uniform insurance coverage for DBT with FFDM or for synthetic 2D mammograms instead of FFDM. There will be an additional learning curve for the radiologist if they convert from the interpretation of FFDM to synthetic 2D mammograms.
56.9 Further Reading
[1] Skaane P, Bandos AI, Eben EB, et al. Two-view digital breast tomosynthesis screening with synthetically reconstructed projection images: comparison with digital breast tomosynthesis with full-field digital mammographic images. Radiology. 2014; 271(3): 655‐663 PubMed
[2] Zuley ML, Guo B, Catullo VJ, et al. Comparison of two-dimensional synthesized mammograms versus original digital mammograms alone and in combination with tomosynthesis images. Radiology. 2014; 271(3): 664‐671 PubMed

Fig. 56.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree