A. Radiation therapy
B. Total parenteral nutrition
C. Hepatorenal syndrome
D. Iodine deposition
For patients in questions 3 to 7, select the most likely diagnosis (A to F) for the hepatic masses. Each option may be used once, more than once, or not at all.
A. Cavernous hemangioma
B. Hepatocellular adenoma
C. Focal nodular hyperplasia
D. Hepatocellular carcinoma
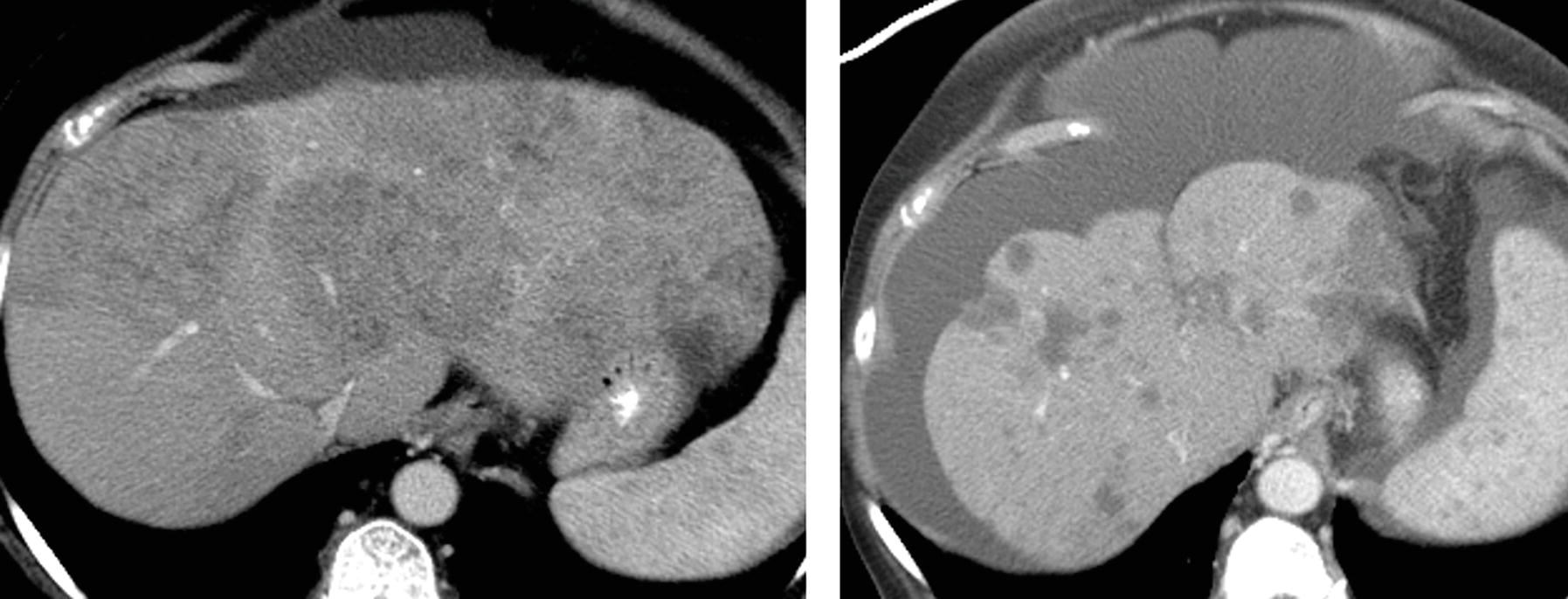
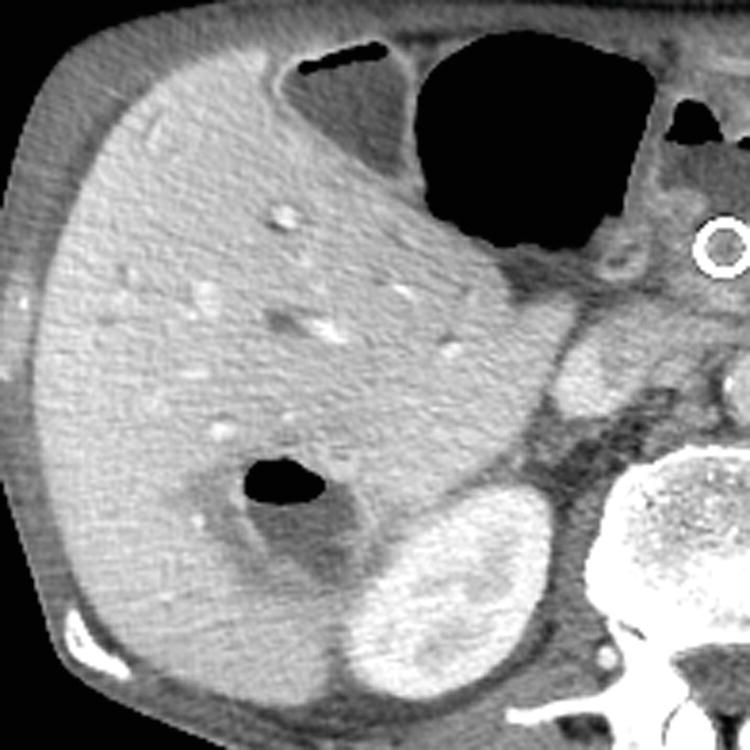
E. Cholangiocarcinoma
F. Abscess
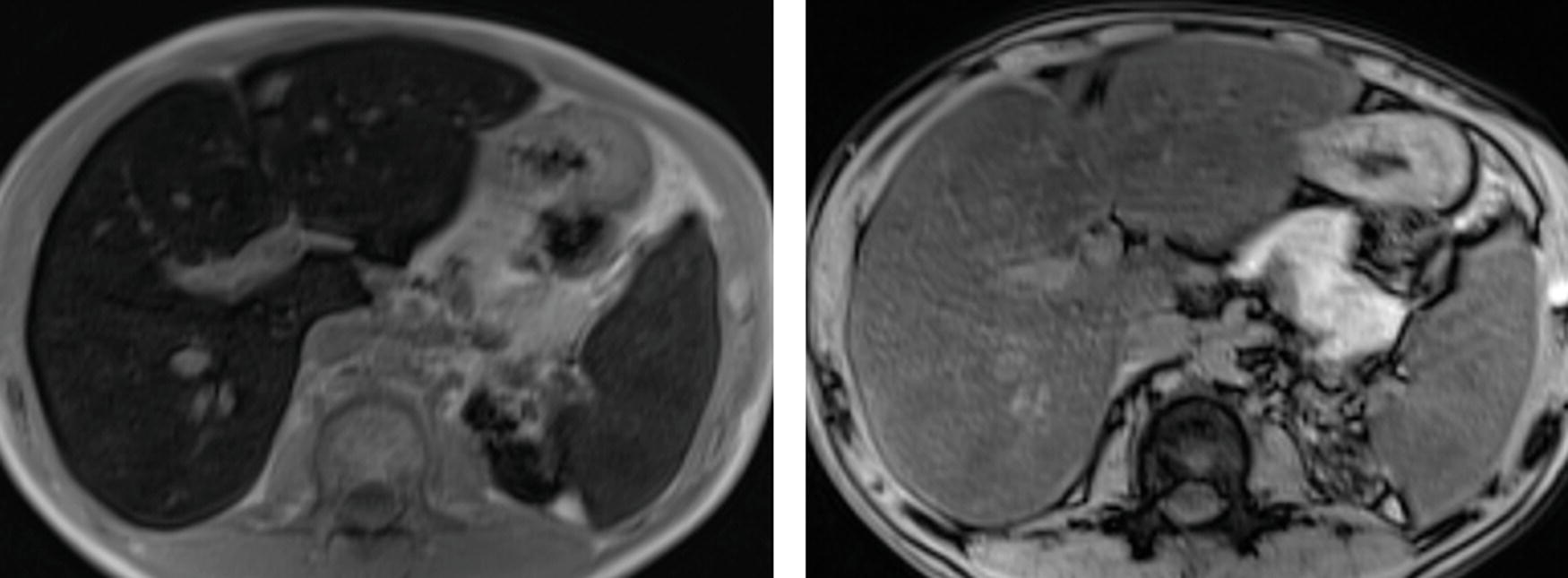
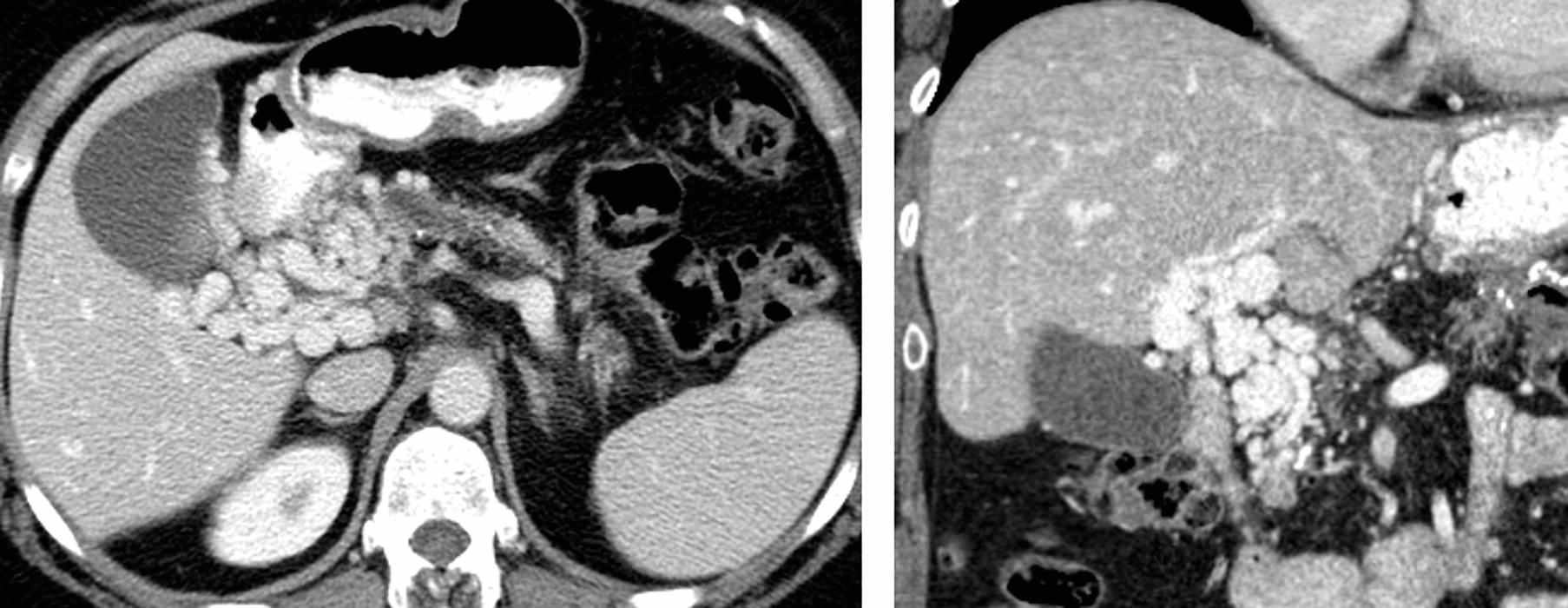
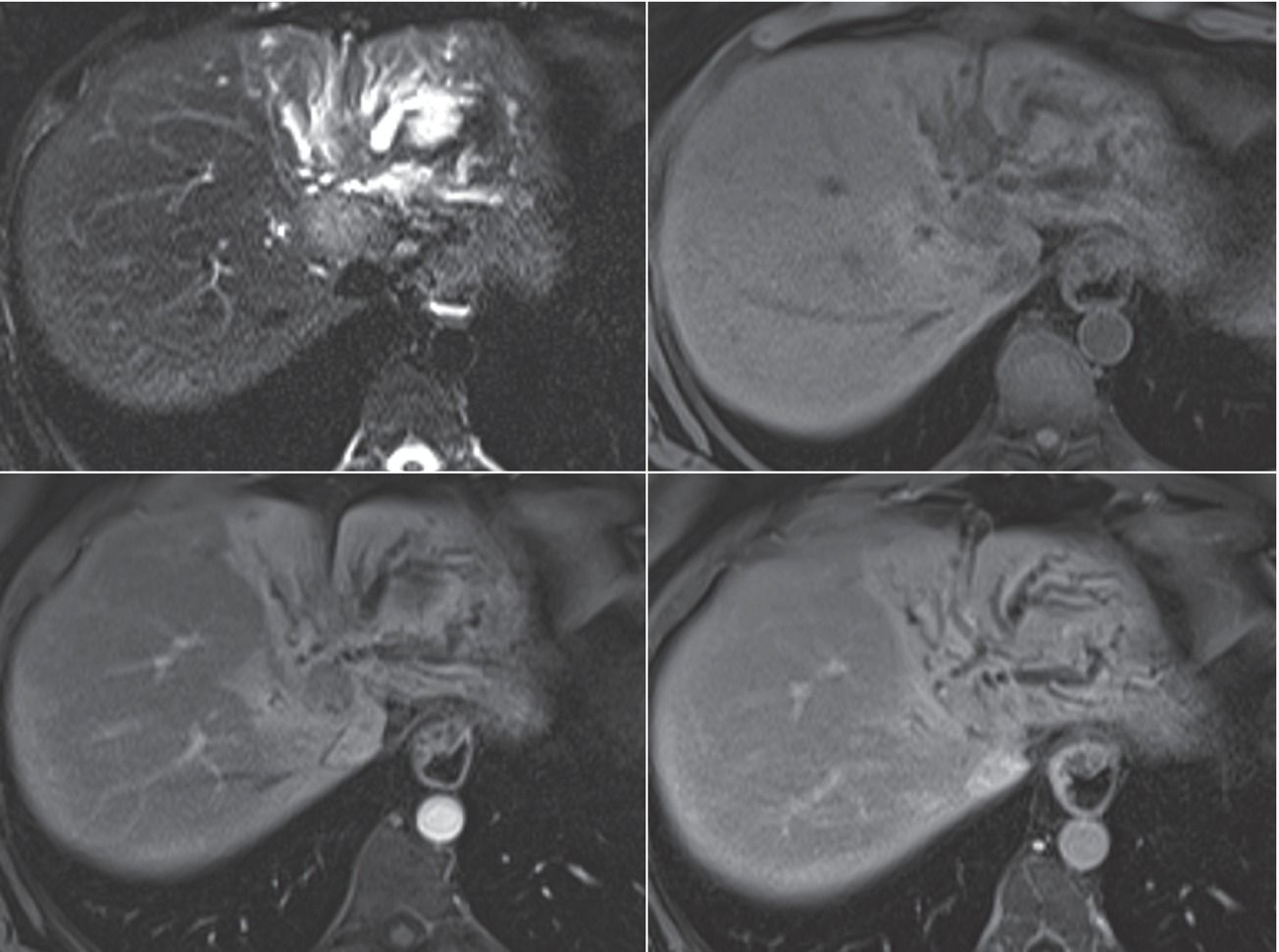
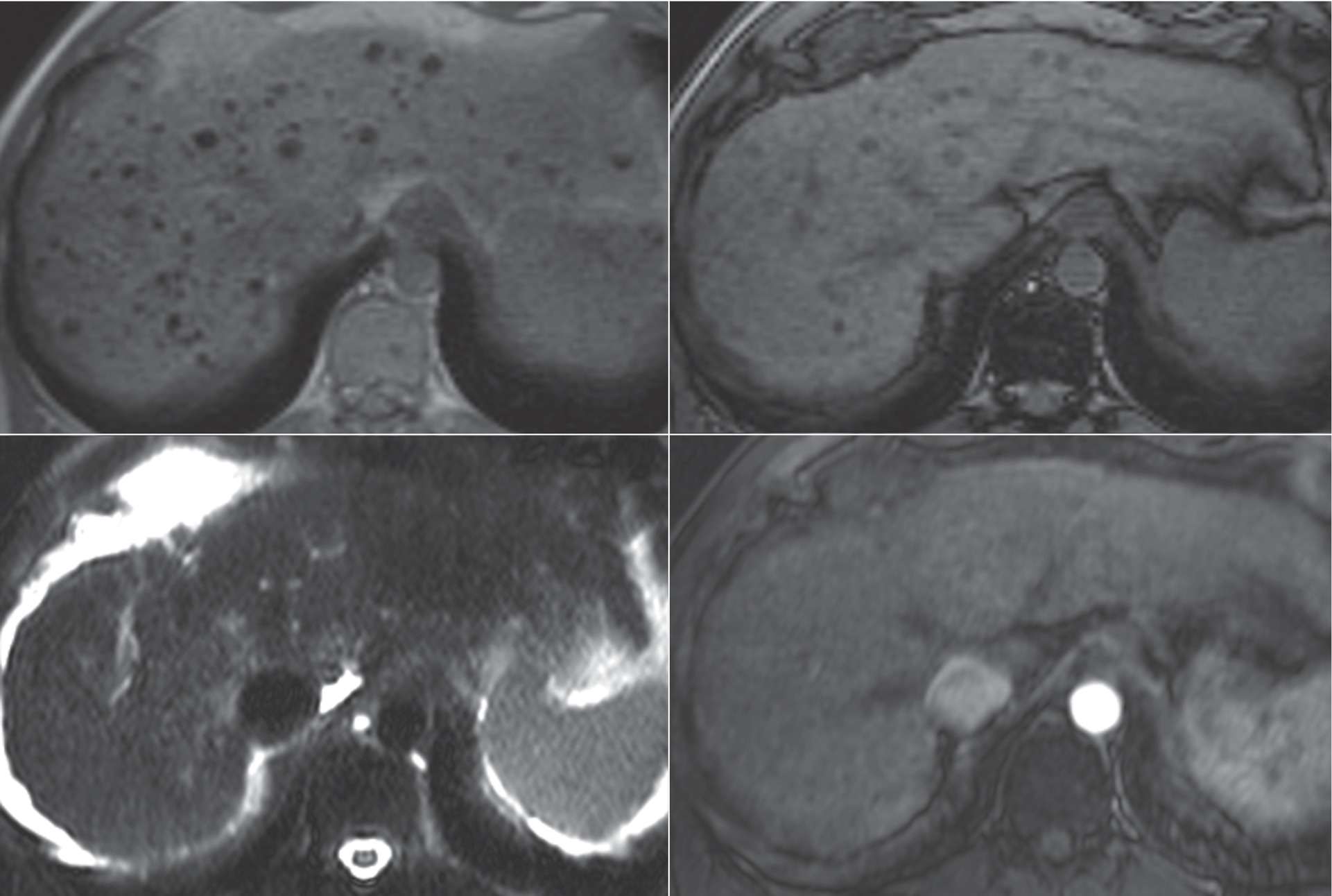
3 A 63-year-old woman with right upper quadrant pain and a liver finding noted on ultrasound. Images are from an MRI using conventional extracellular gadolinium contrast.
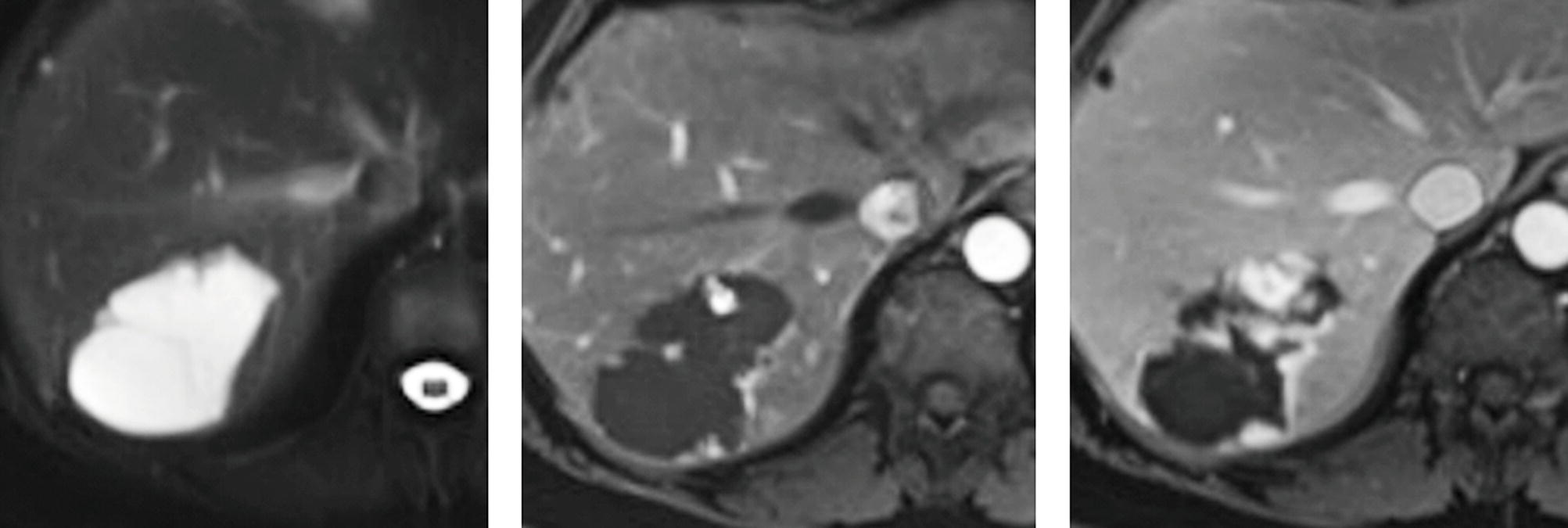
FS T2W, arterial phase T1W+gad, and delayed phase T1W+gad.
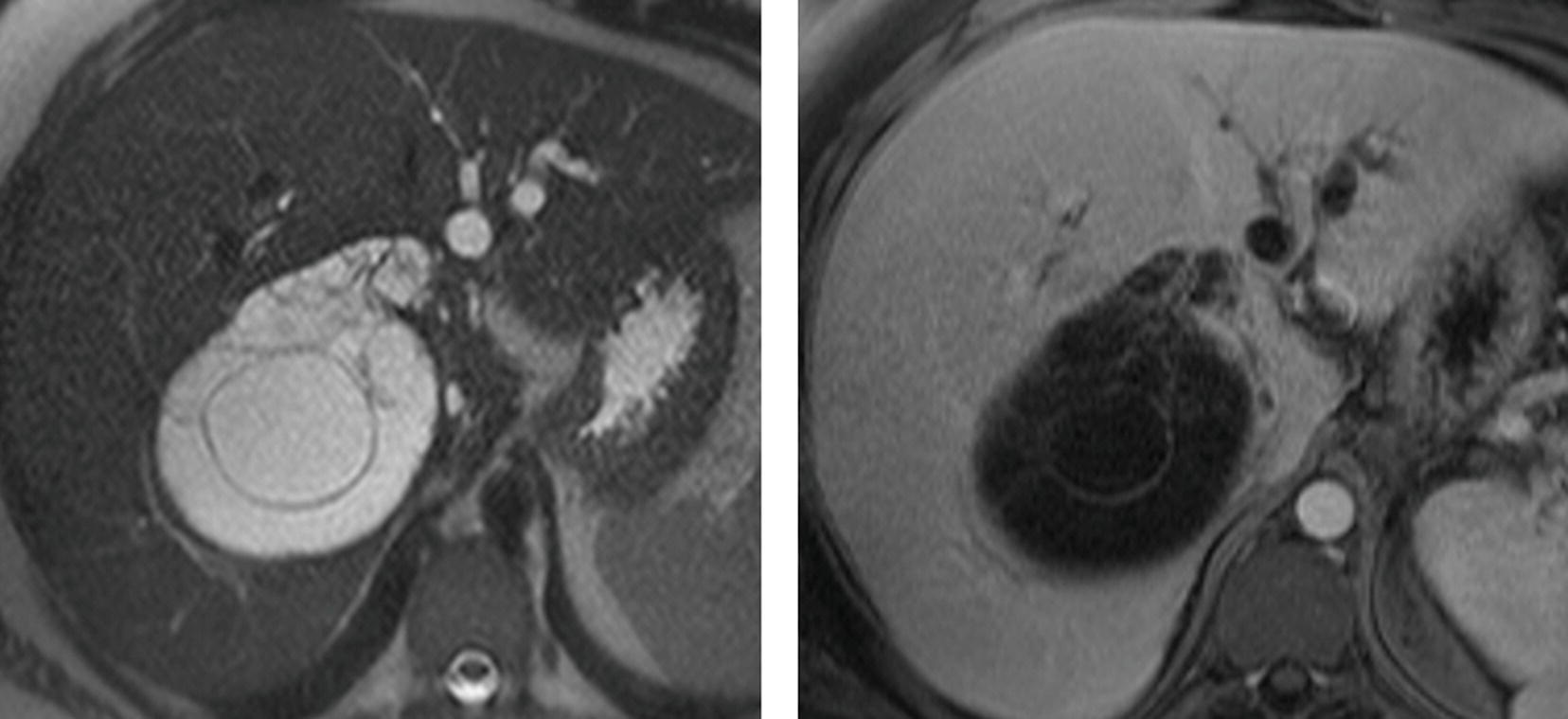
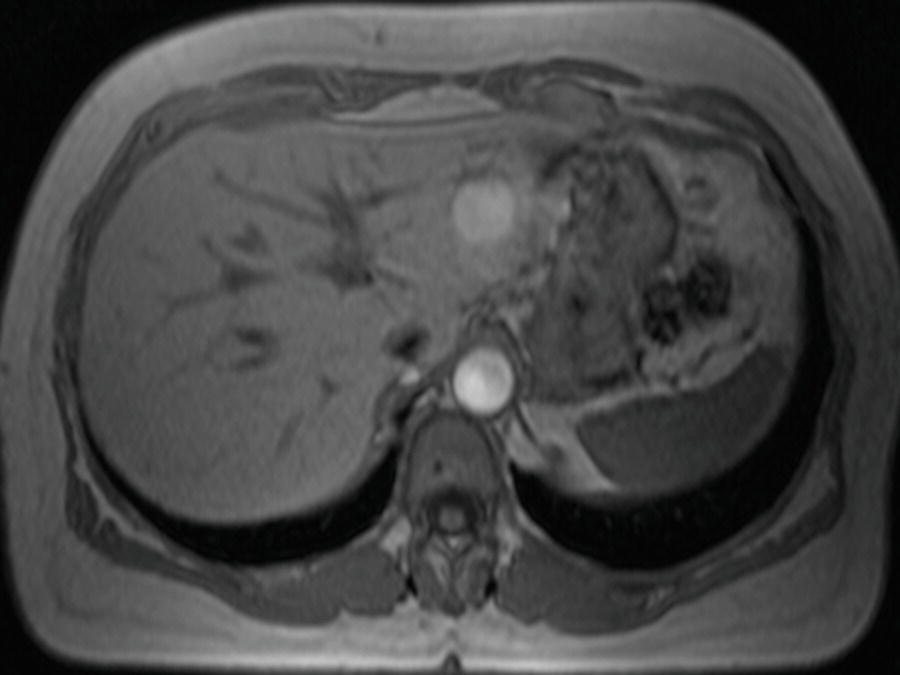
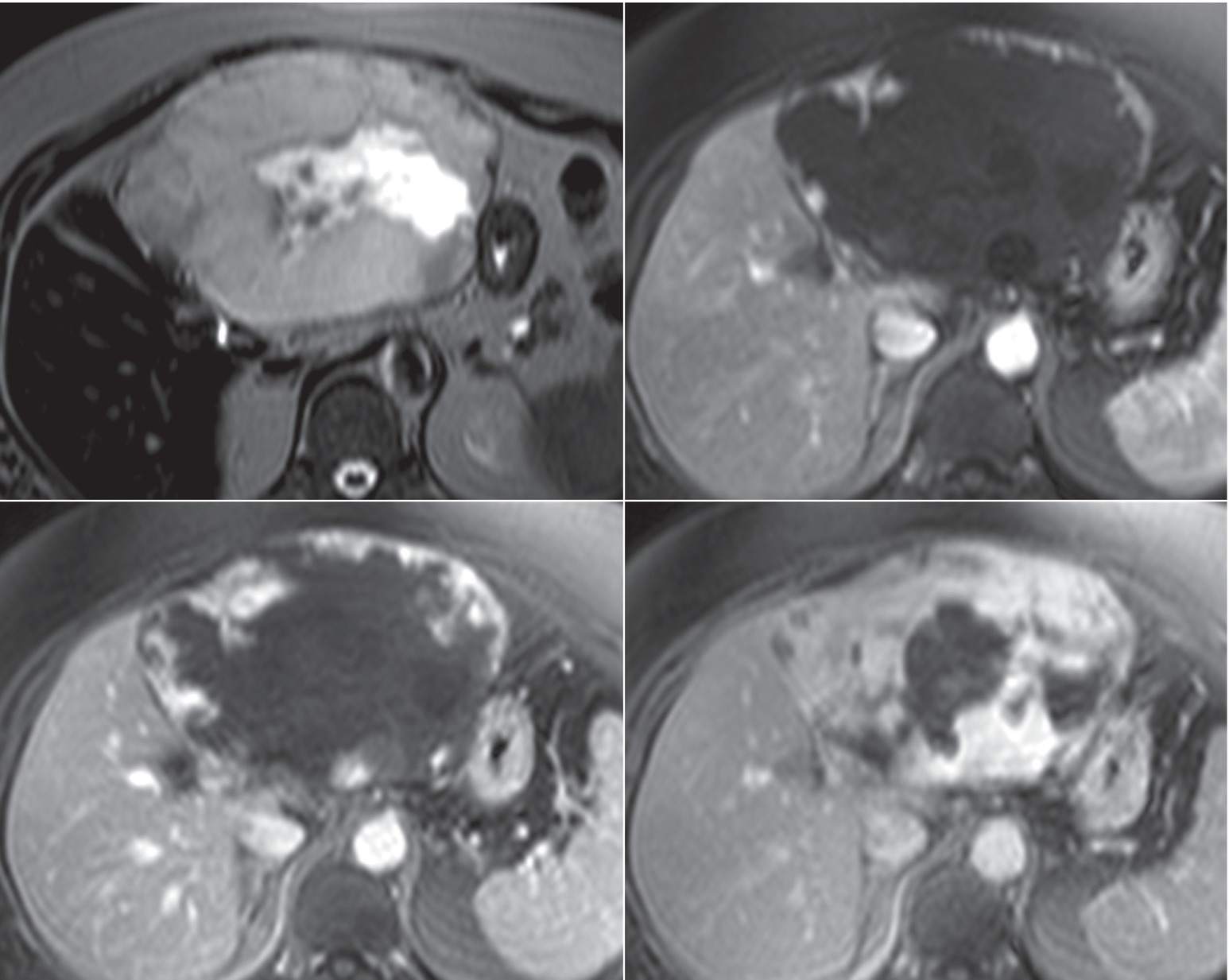
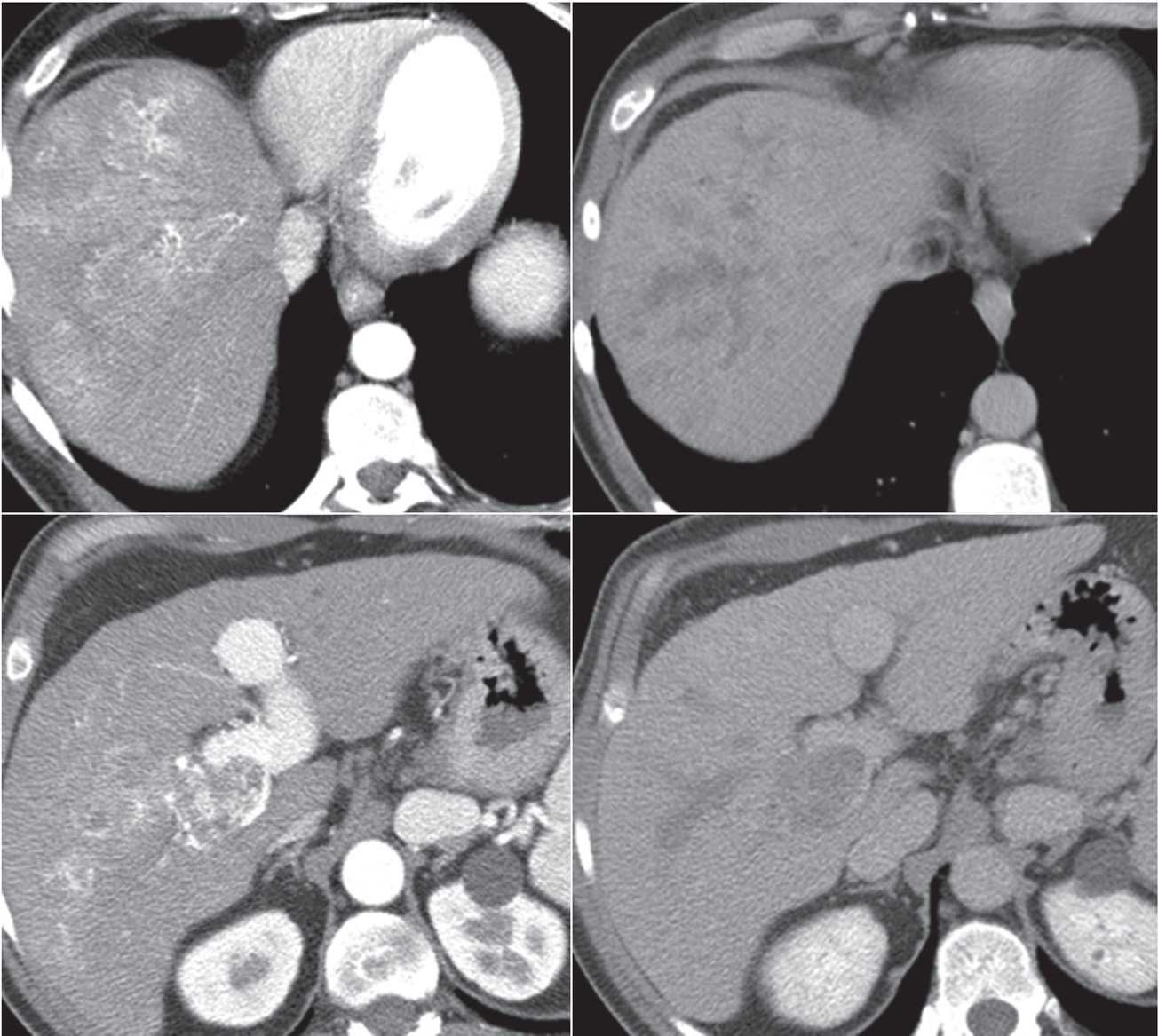
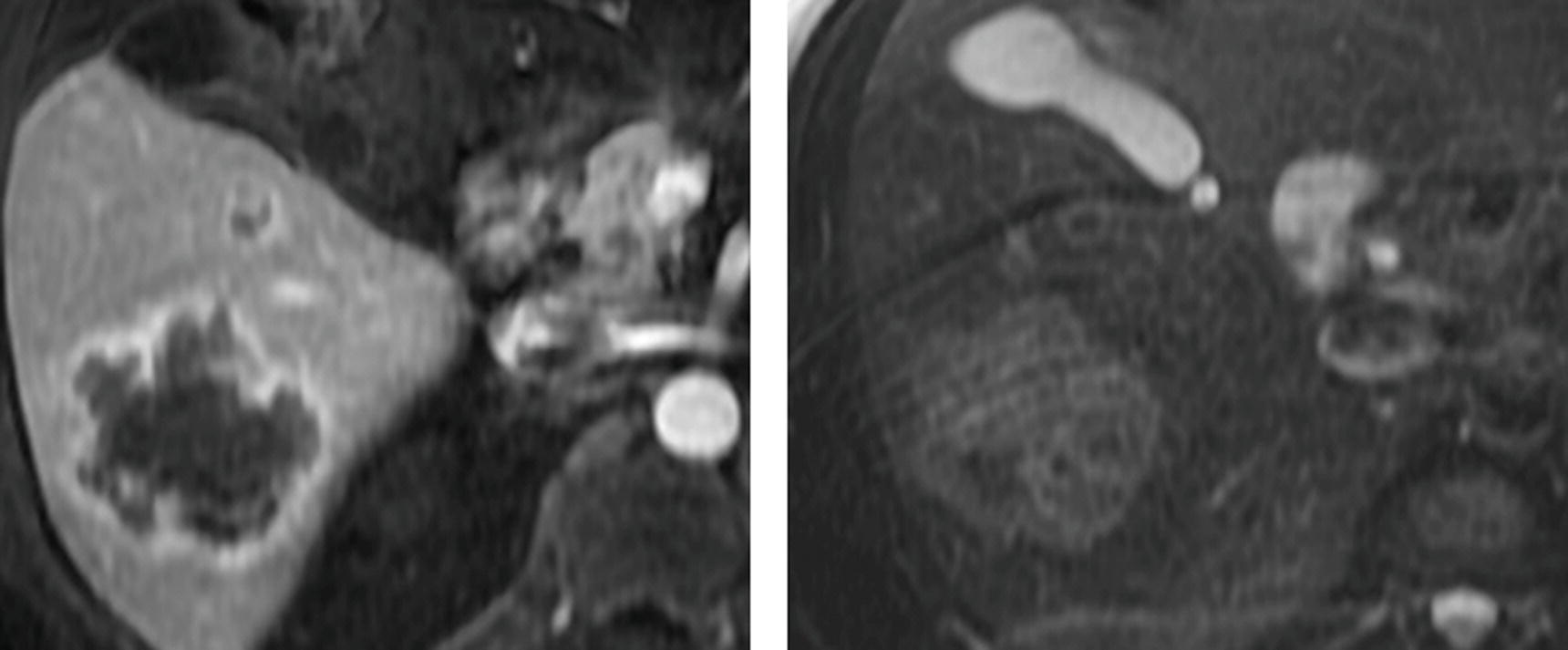
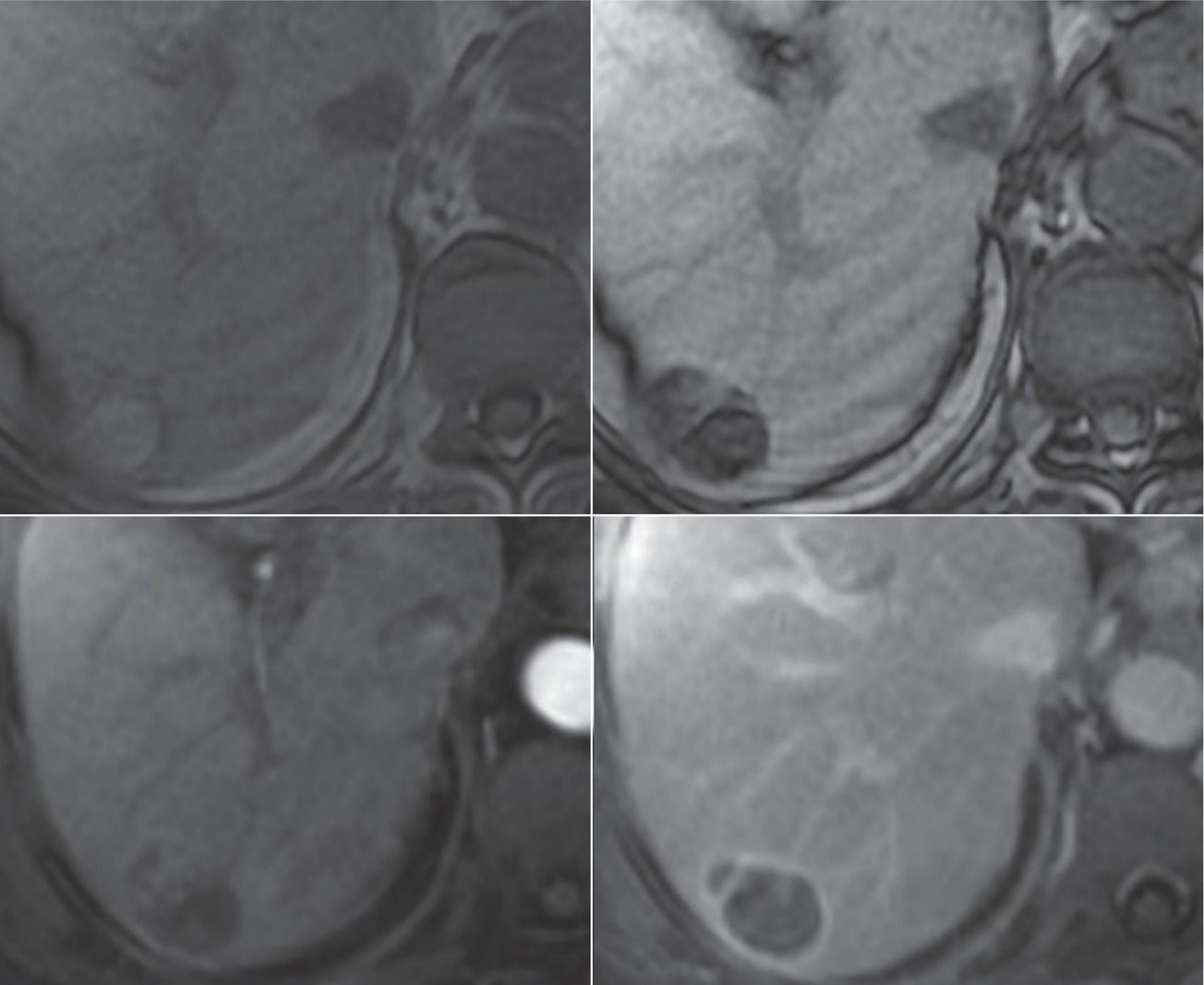
4 A 47-year-old woman with cirrhosis secondary to hepatitis C. Images from an MRI performed with conventional extracellular gadolinium contrast are shown.
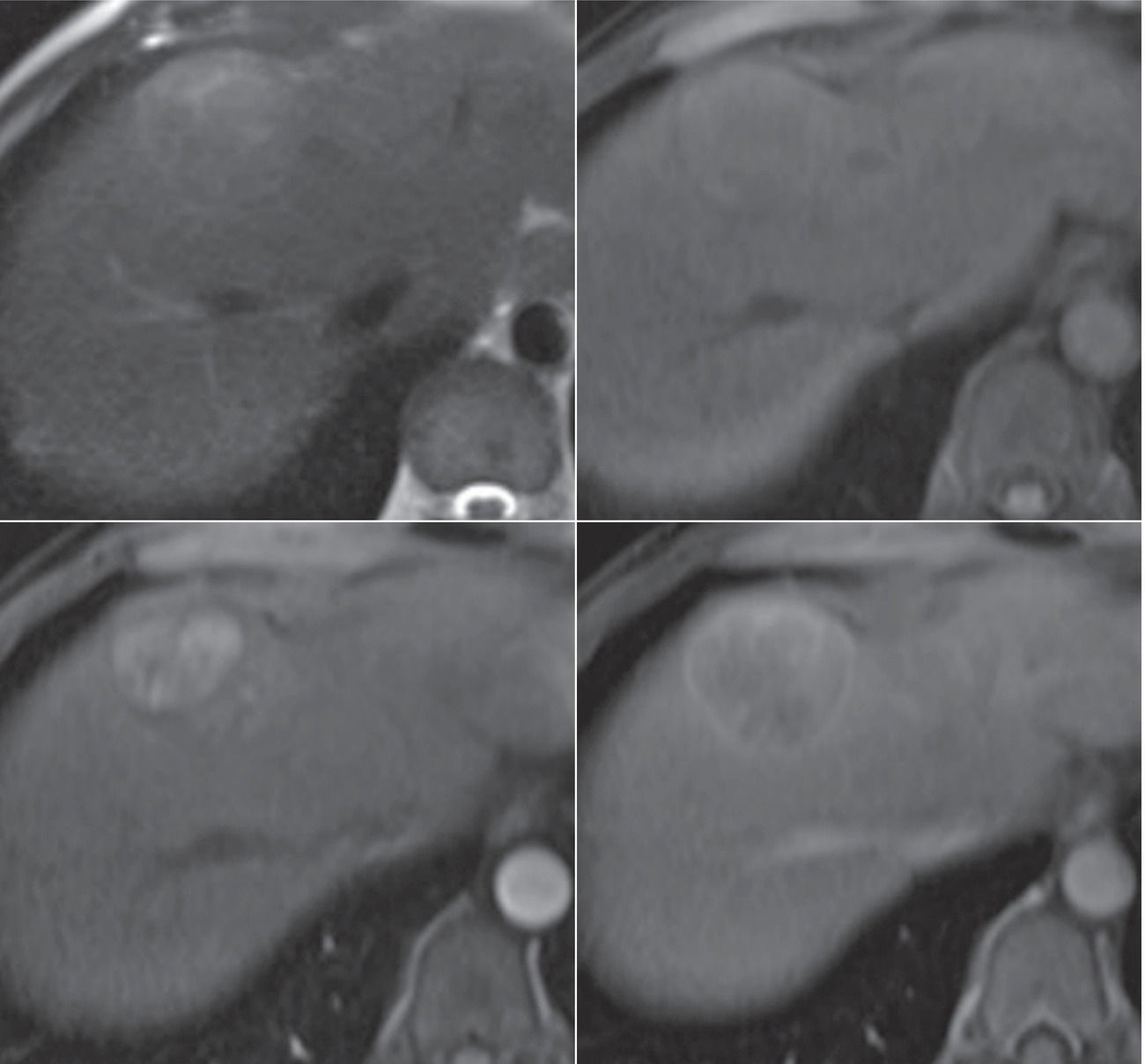
Top row: T2W and FS T1W. Bottom row: Arterial and delayed phase FS T1W+gad.
5 A 46-year-old woman with painless jaundice. Images from an MRI performed with conventional extracellular gadolinium contrast are shown.
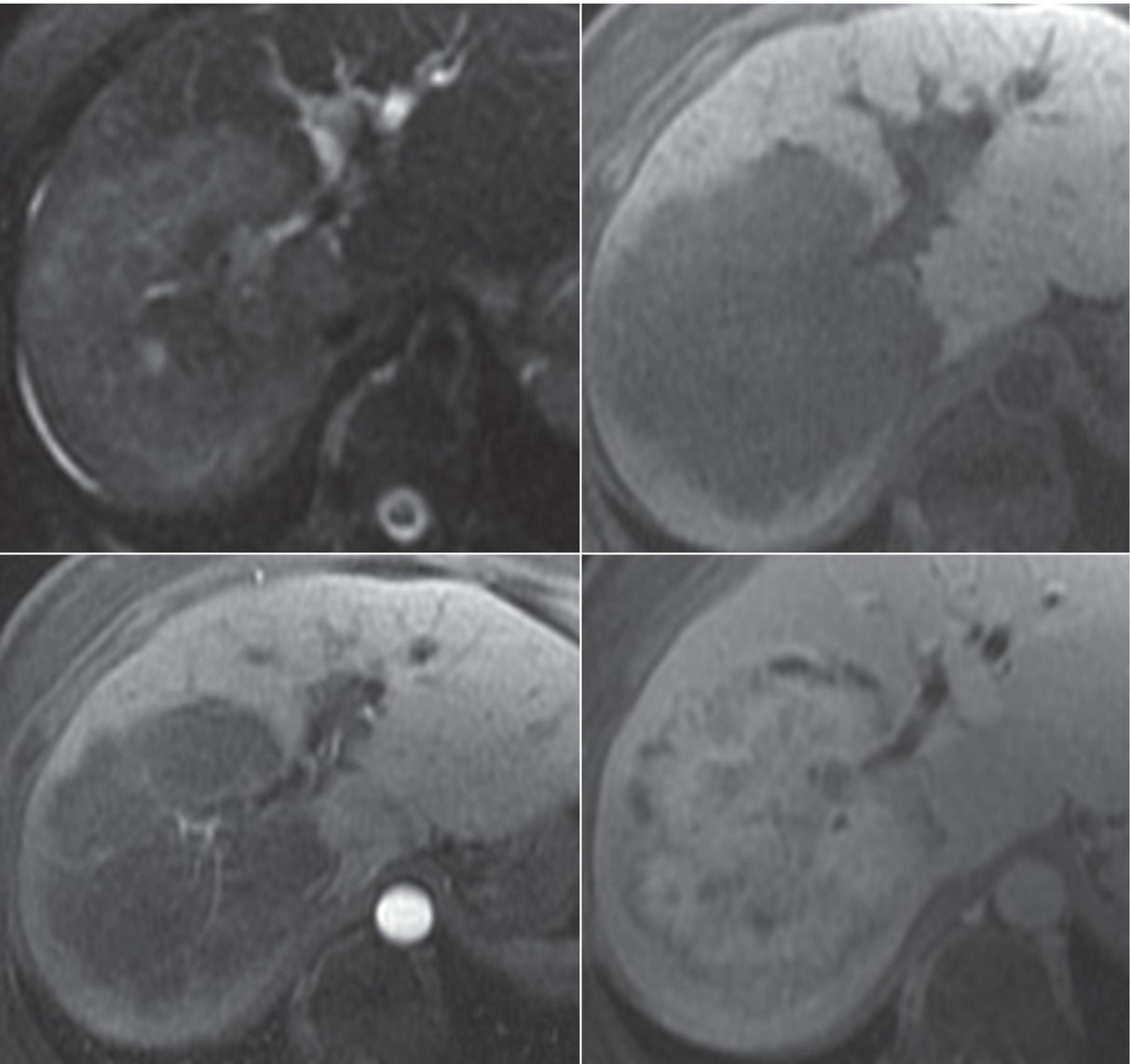
Top row: T2W and FS T1W. Bottom row: Arterial and delayed phase FS T1W+gad.
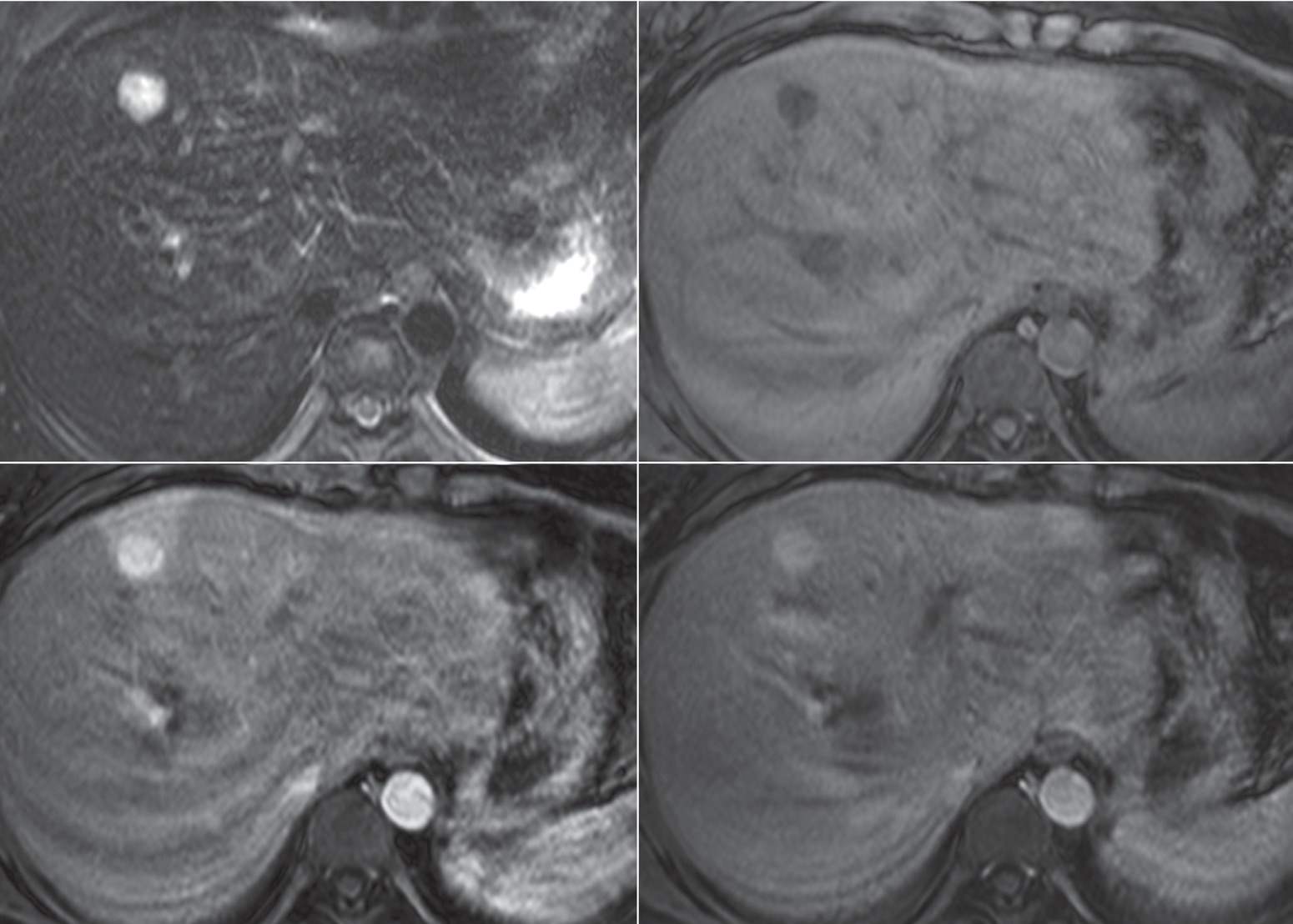
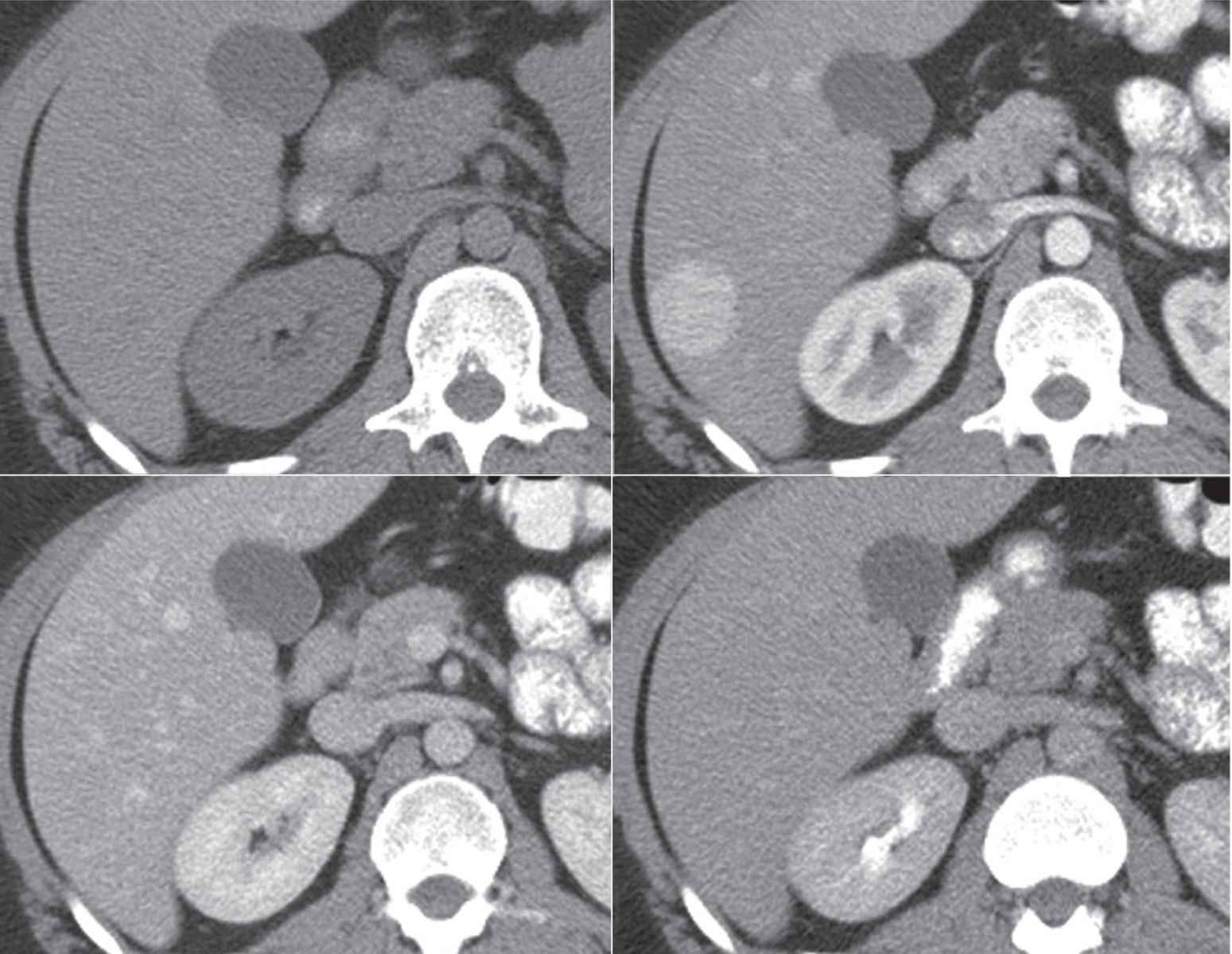
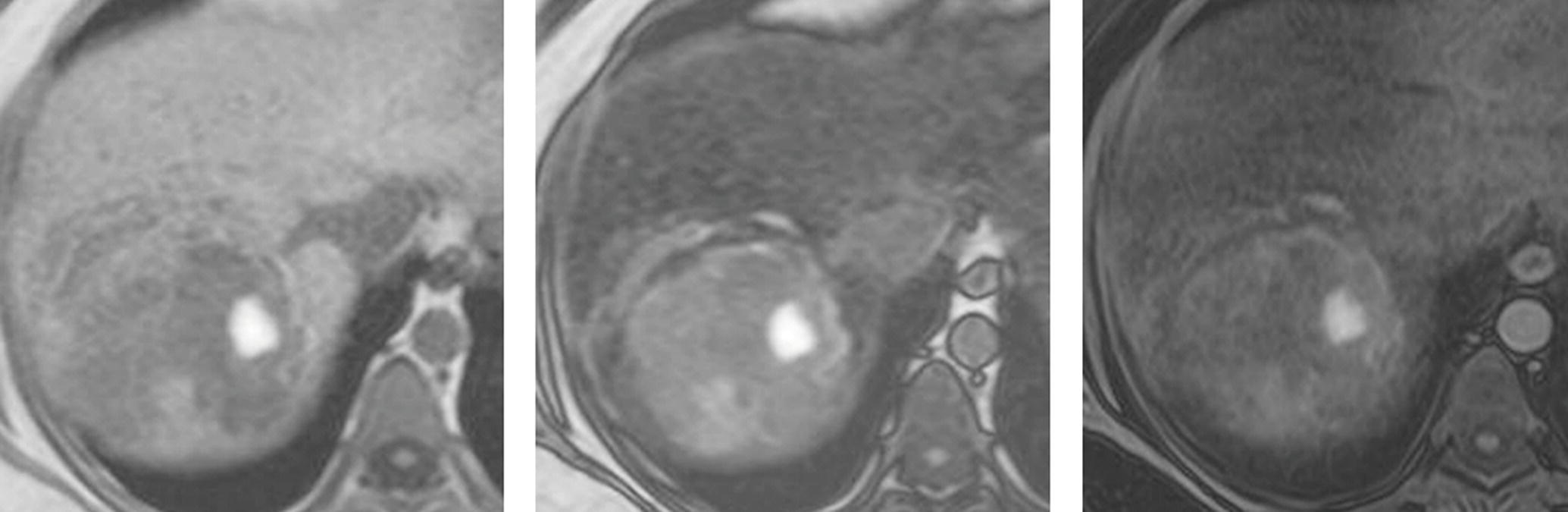
6 A 21-year-old woman found to have a liver lesion on ultrasound. Images from an MRI using hepatobiliary gadolinium contrast agent gadoxetate disodium (Eovist—Bayer HealthCare) are shown.
T2W, arterial phase FS T1W+hepatobiliary gad, and 20-minute FS T1W+hepatobiliary gad.
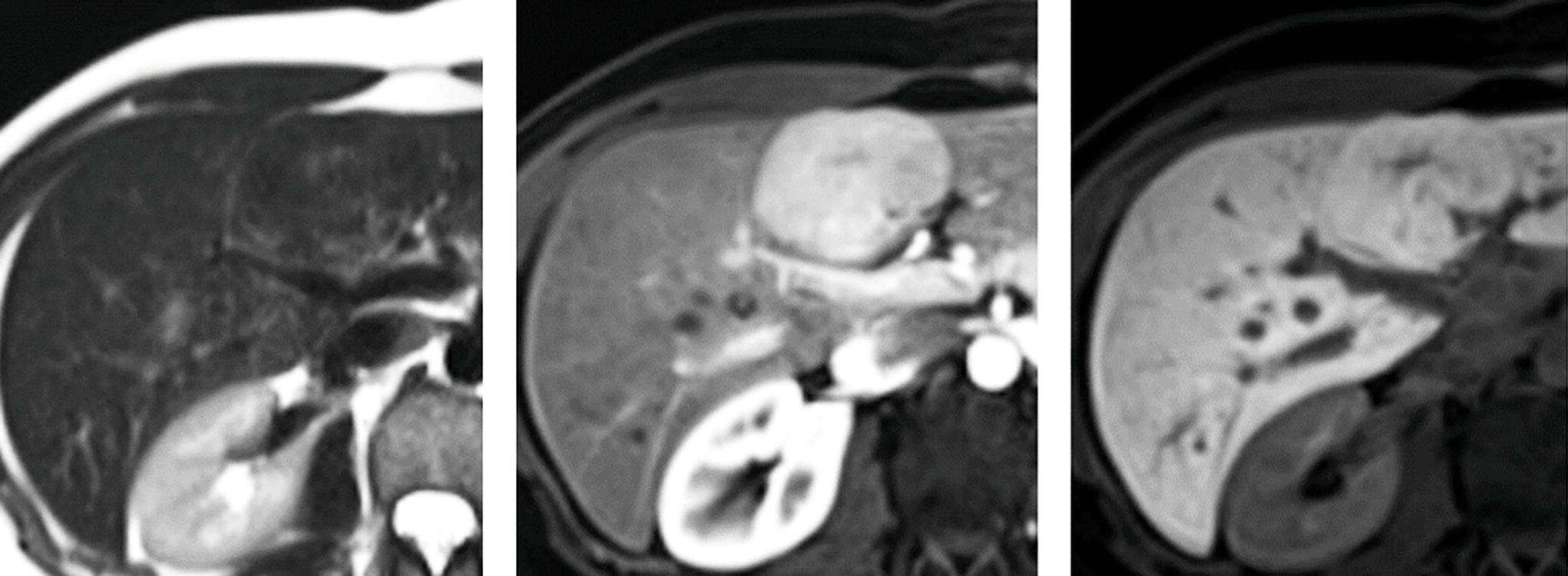
7 A 51-year-old man with hepatitis B and cirrhosis. Images from an MRI performed with hepatobiliary contrast agent are shown.
FS T2W, arterial phase FS T1W+hepatobiliary gad, and a 20-minute FS T1W+hepatobiliary gad.
8 Which of the following would be considered an ancillary feature favoring hepatocellular carcinoma rather than a major feature according to the Liver Imaging Reporting and Data System (LI-RADS)?
A. Washout appearance
B. Capsule appearance
C. Arterial enhancement
D. Hepatobiliary phase hypointensity
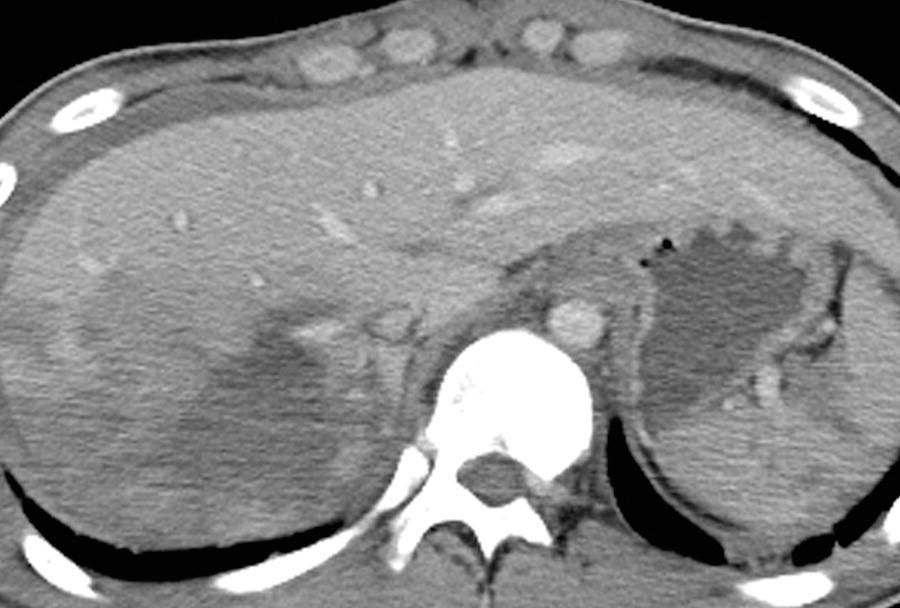
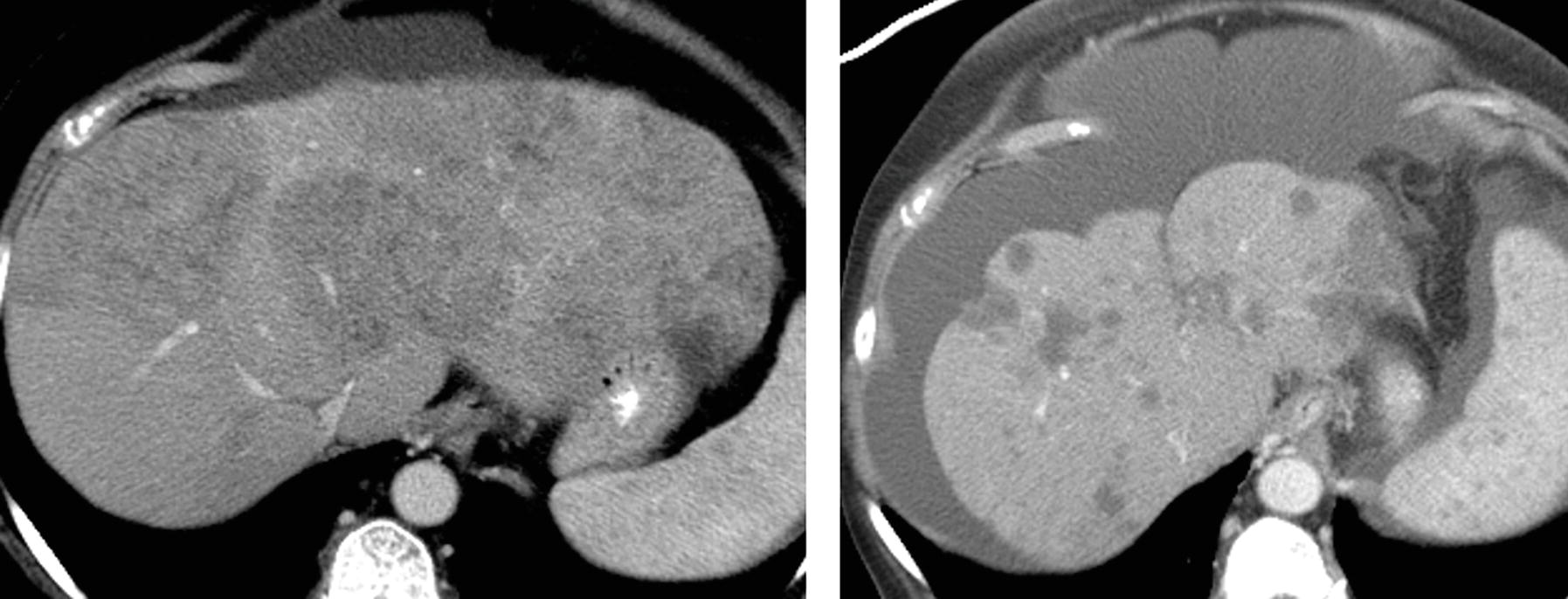
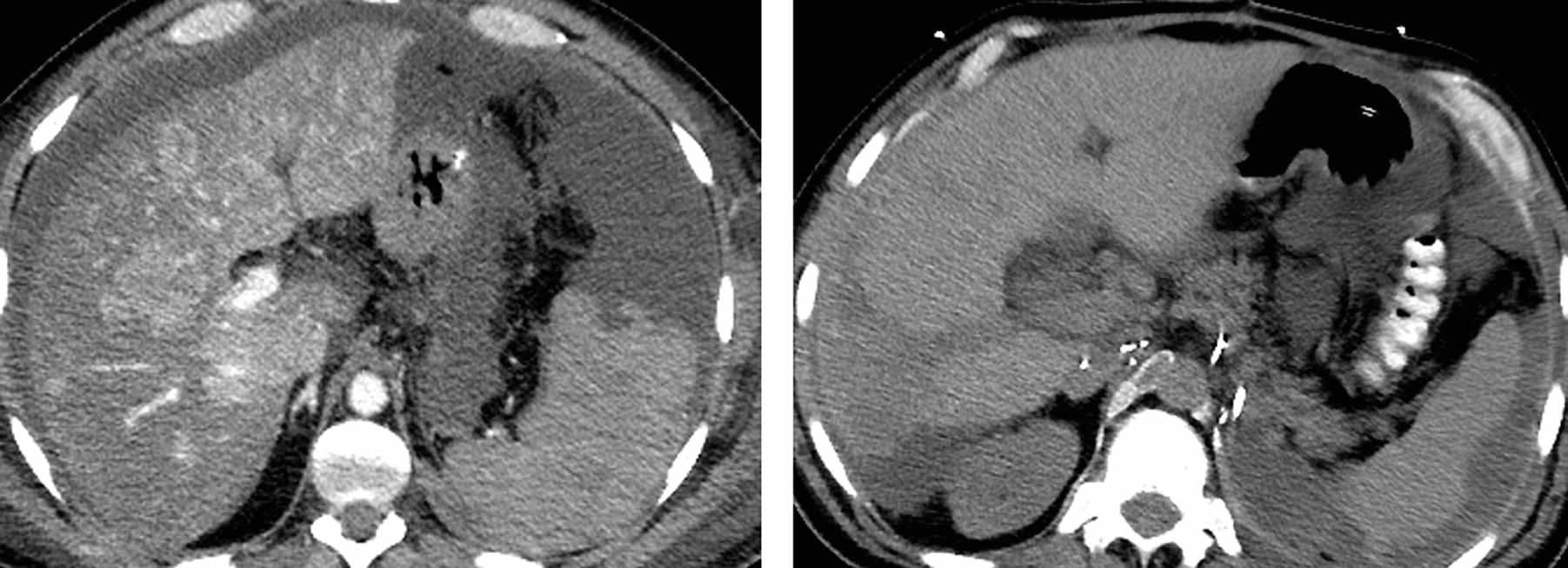
9 Images from a CT on a 55-year-old man with hepatitis C and cirrhosis are shown. Arterial phase images are shown on the left, and delayed images are shown on the right. Which LI-RADS category best fits the findings?
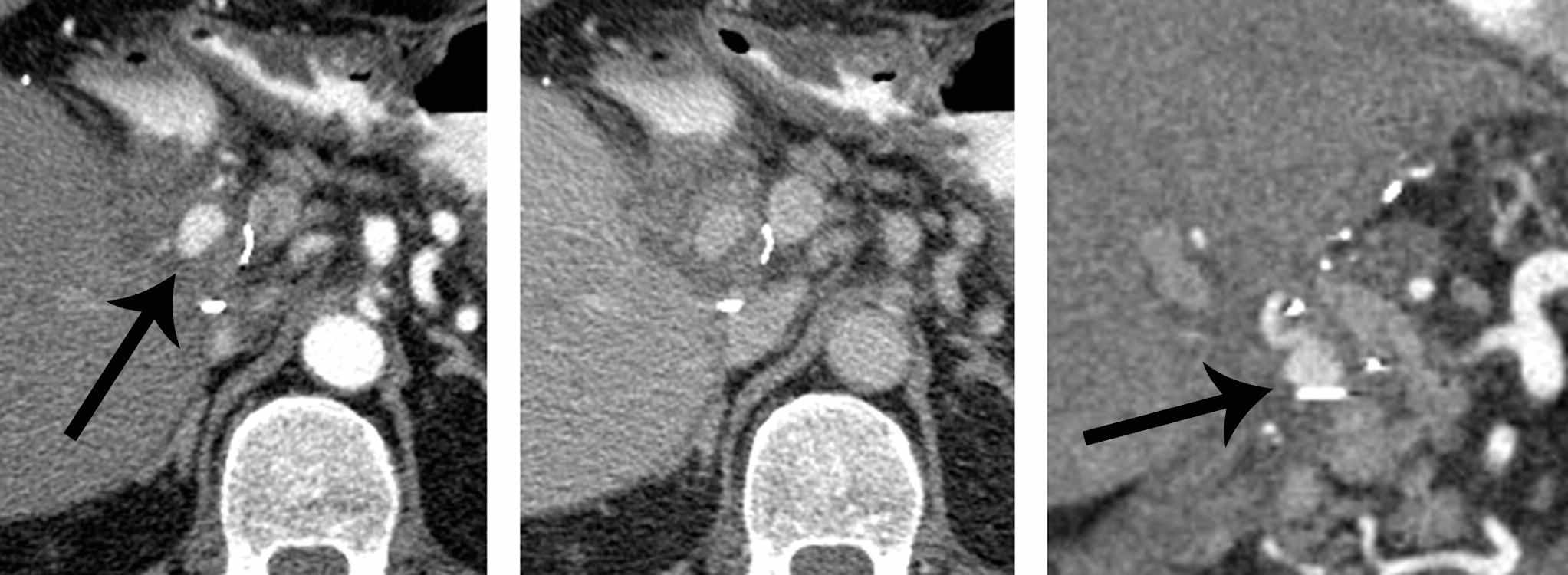
A. LR-2 probably benign
B. LR-3 intermediate probability for hepatocellular carcinoma
C. LR-4 probably hepatocellular carcinoma
D. LR-5 definitely hepatocellular carcinoma
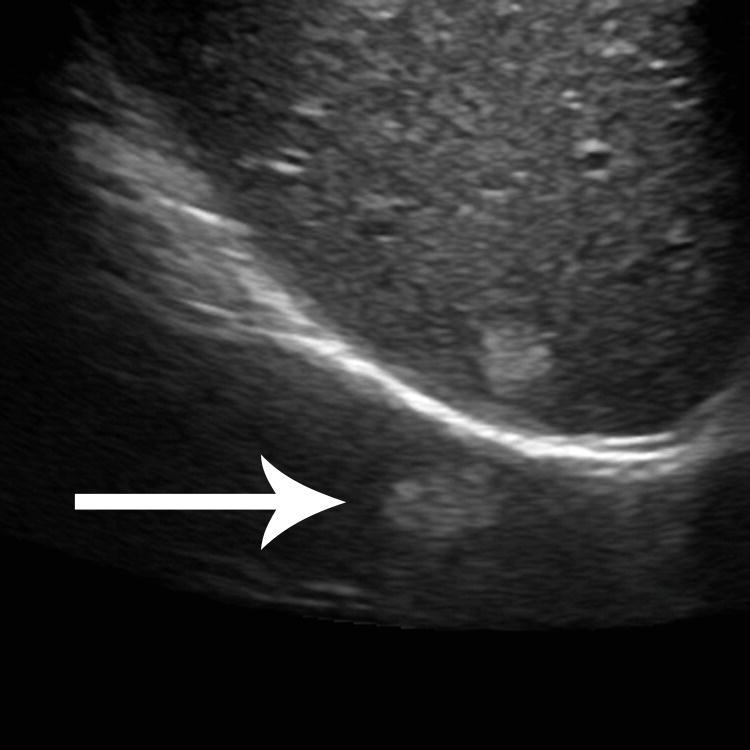
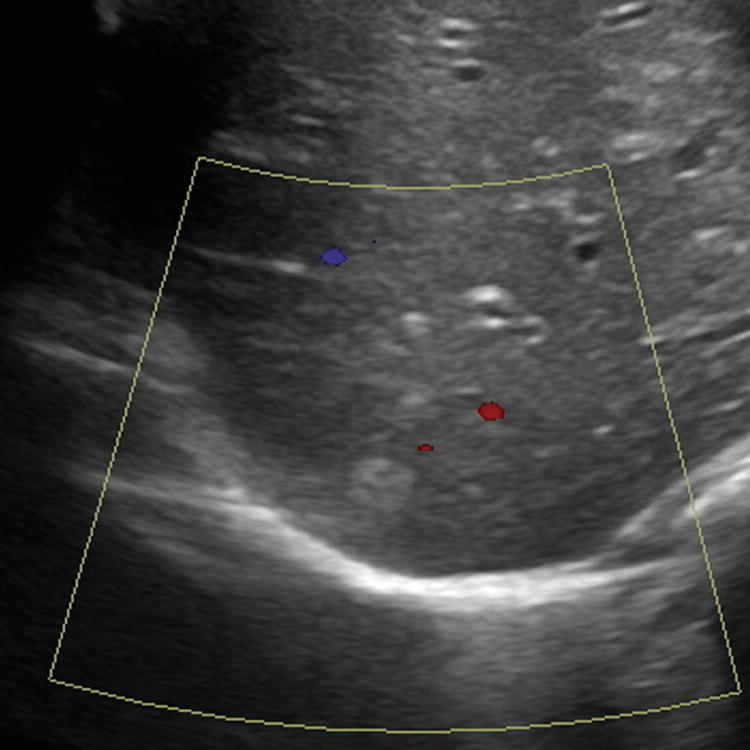
10a A 24-year-old man with no history of liver disease presents with epigastric pain and vomiting. A transverse image from an abdominal ultrasound is shown. What is the most likely diagnosis?
A. Hemangioma
B. Hepatocellular carcinoma
C. Angiomyolipoma
D. Metastasis
A. Lung nodule
B. Mirror artifact
C. Peritoneal nodule
D. Twinkle artifact
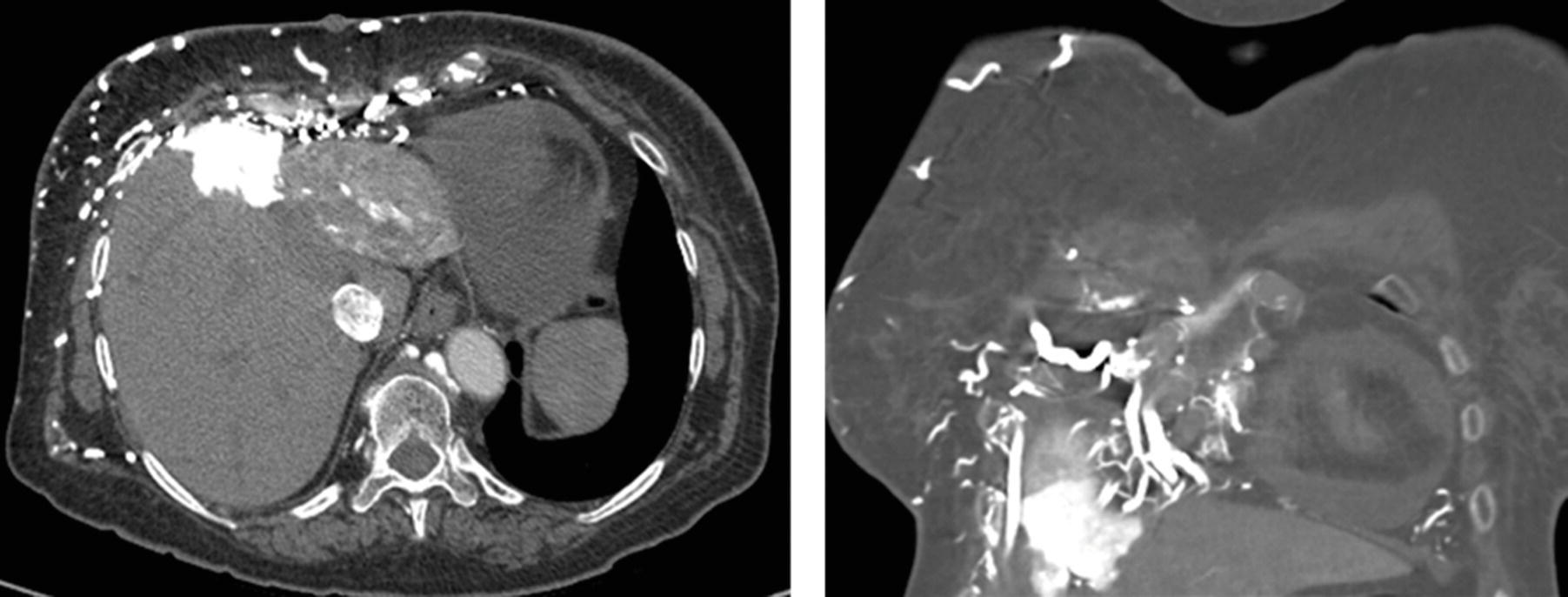
11 A 22-year-old patient presents with abdominal pain. A venous phase CT and hepatic venogram are shown. Which of the following is the most common known etiology of this disease process?
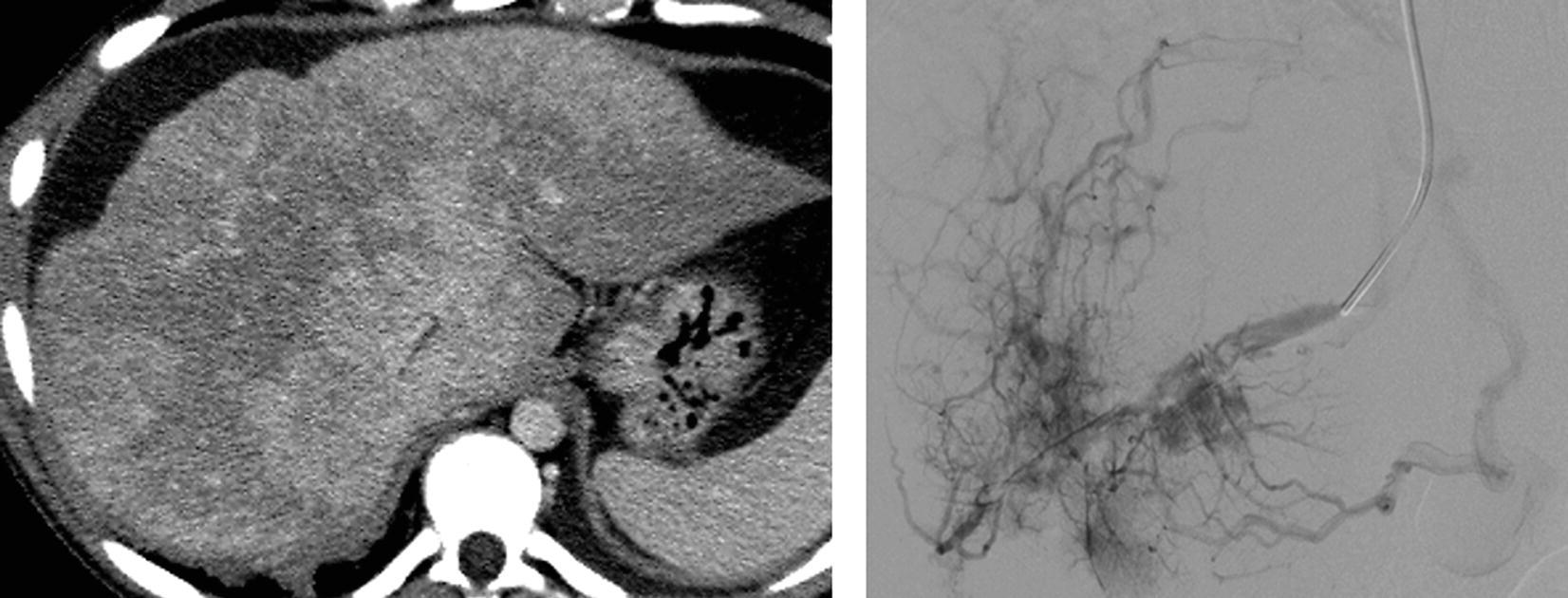
A. Thrombophilia
B. Viral hepatitis
C. Alcohol abuse
D. Congenital defect
For the patients in questions 12 to 15, select the most likely diagnosis (A to F). Each option may be used once or not at all.
A. Von Meyenburg complex
B. Pyogenic abscess
C. Biliary cystadenoma/cystadenocarcinoma
D. Peritoneal carcinomatosis
E. Polycystic liver disease in autosomal-dominant polycystic kidney disease
F. Subcapsular hematoma
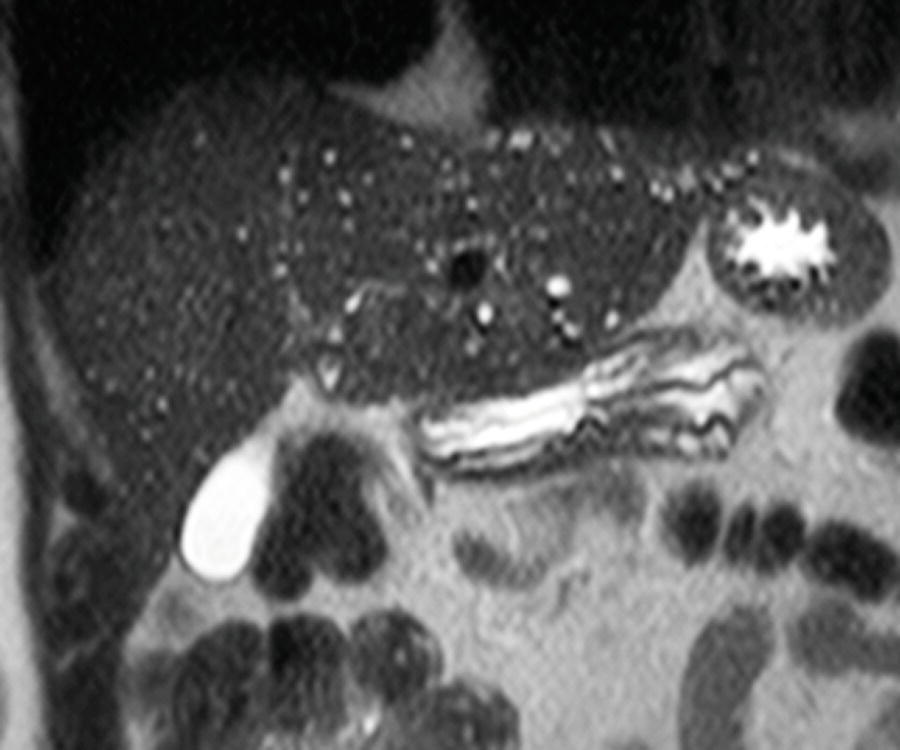
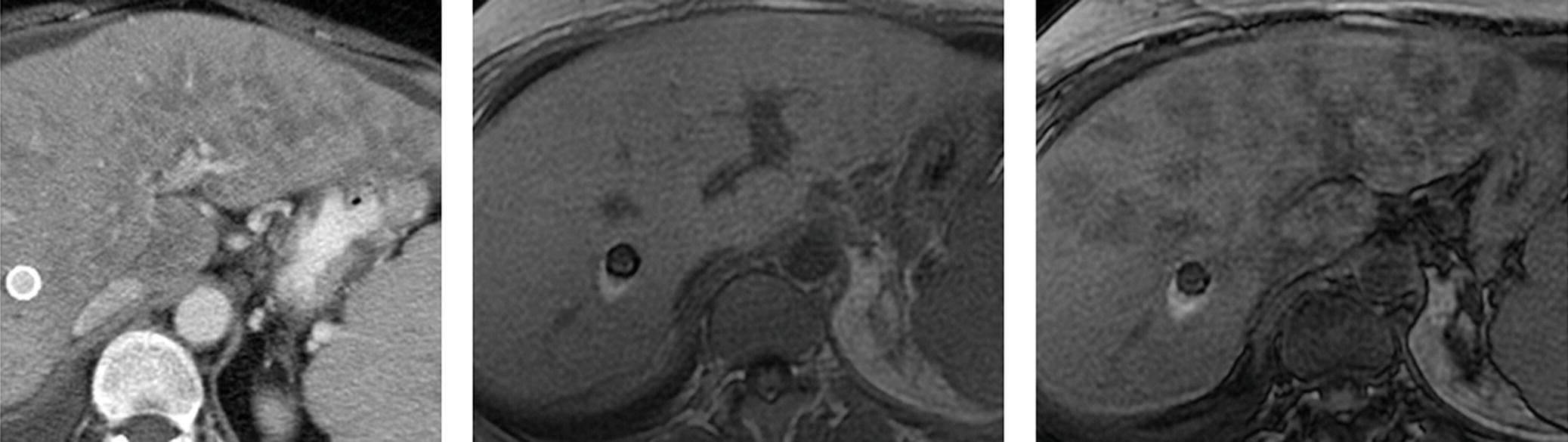
13 A woman with chronic renal failure, fatigue, and decreasing hematocrit.
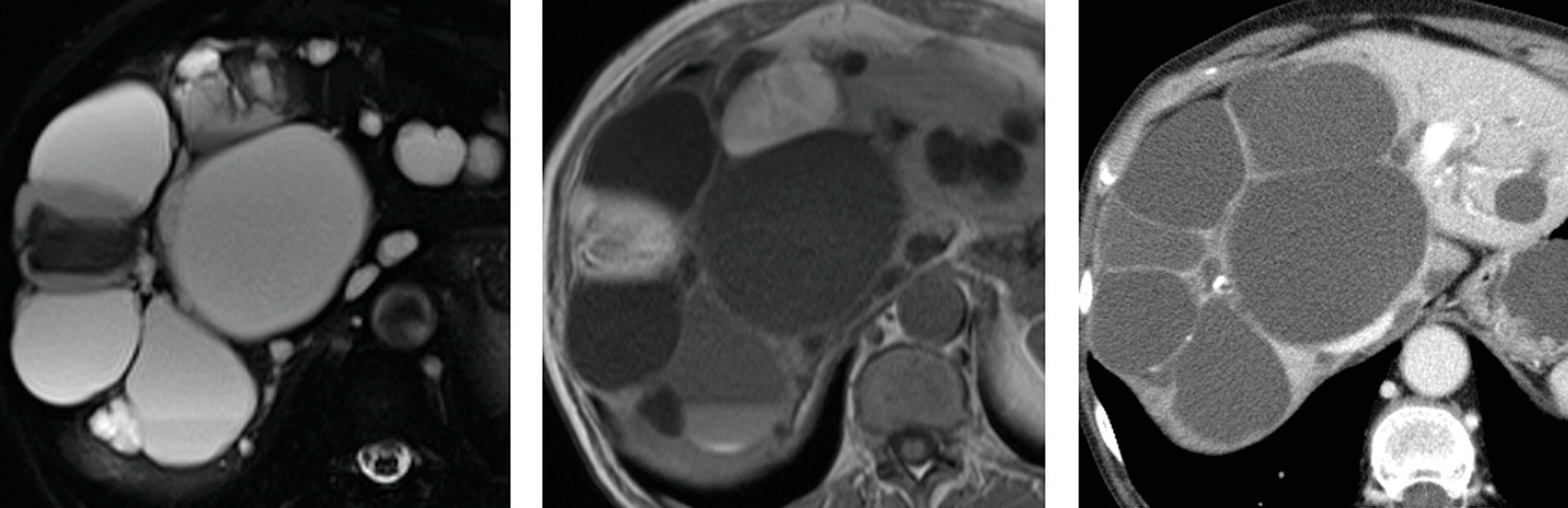
FS T2W, T1W MRI, and venous phase CT.
14 A 63-year-old man with pancreatic cancer status post common bile duct stent placement complains of worsening pain.
A. Right posterior hepatic notch sign
B. Macronodularity
C. Caudate lobe hypertrophy
D. Expanded gallbladder fossa sign
17 Regarding contrast agent selection for liver MRI, which of the following indications has the best consensus for the use of a hepatobiliary contrast agent such as gadoxetate disodium (Eovist—Bayer HealthCare) over a conventional extracellular contrast agent?
A. Assessing for residual or recurrent hepatocellular carcinoma after transarterial chemoembolization
B. Differentiating between focal nodular hyperplasia and hepatocellular adenoma
C. Confirming a hemangioma
D. Screening for hepatocellular carcinoma in a patient with hemochromatosis
18 A 54-year-old man undergoes MR imaging for evaluation of a liver mass. Among the choices listed, which is the most likely diagnosis?
Venous phase FS T1W+gad and T2W MRI.
A. Metastasis
B. Hemangioma
C. Simple cyst
D. Focal nodular hyperplasia
19a A 35-year-old man with end-stage renal disease underwent an abdominal ultrasound as part of preoperative evaluation for renal transplant. An MRI was performed to further evaluate an abnormal liver. The cause of the disease process revealed on these T1W GRE in-phase and out-of-phase images is most likely:
A. Viral hepatitis.
B. Blood transfusions.
C. Alcohol consumption.
D. Hereditary depositional disease.
19b Which of the following parameters would be the most effective for reducing T2* effect and susceptibility artifact?
A. Gradient-echo sequence and shorter TE
B. Gradient-echo sequence and longer TE
C. Fast spin-echo sequence and shorter TE
D. Fast spin-echo sequence and longer TE
20a A 46-year-old woman with breast ductal carcinoma in situ (DCIS) was found to have a liver lesion on breast MRI. Dedicated liver MRI was performed with a conventional extracellular contrast agent for further evaluation. What is the most likely diagnosis?
Top row: FS T2W and FS T1W. Bottom row: Arterial and delayed phase FS T1W+gad.
A. Hemangioma
B. Metastatic breast cancer
C. Abscess
D. Hepatocellular carcinoma
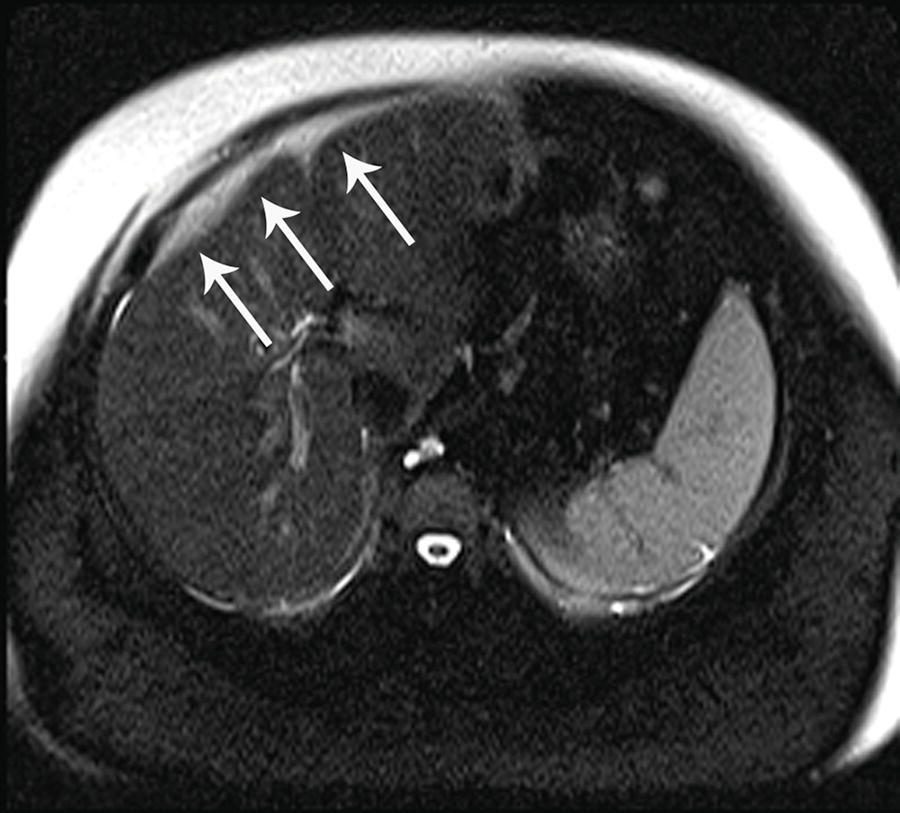
20b This is the arterial phase postcontrast T1W image from the previous case. What finding is indicated by the arrows?
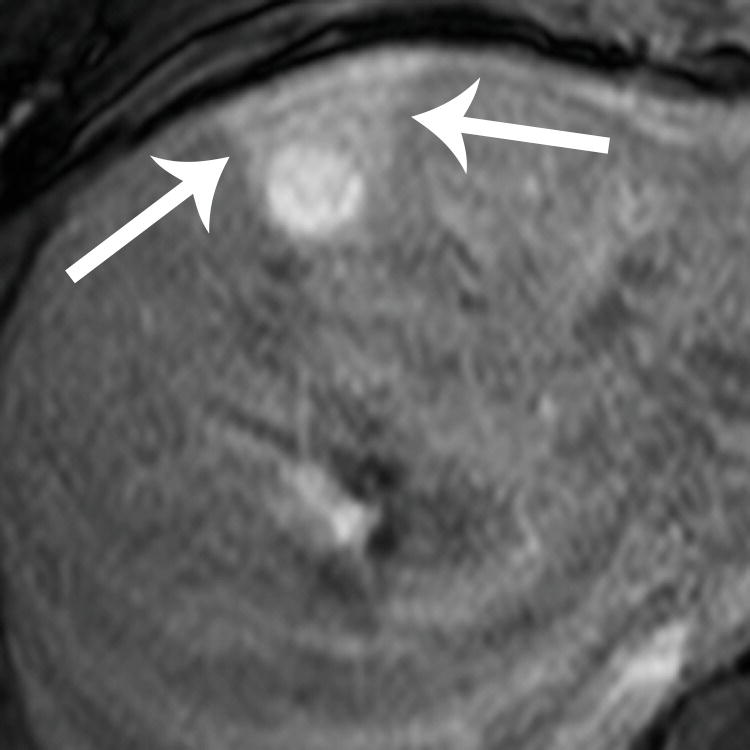
A. Poor fat saturation
B. Focal fatty sparing
C. Transient hepatic intensity difference (THID)
D. Hemorrhage
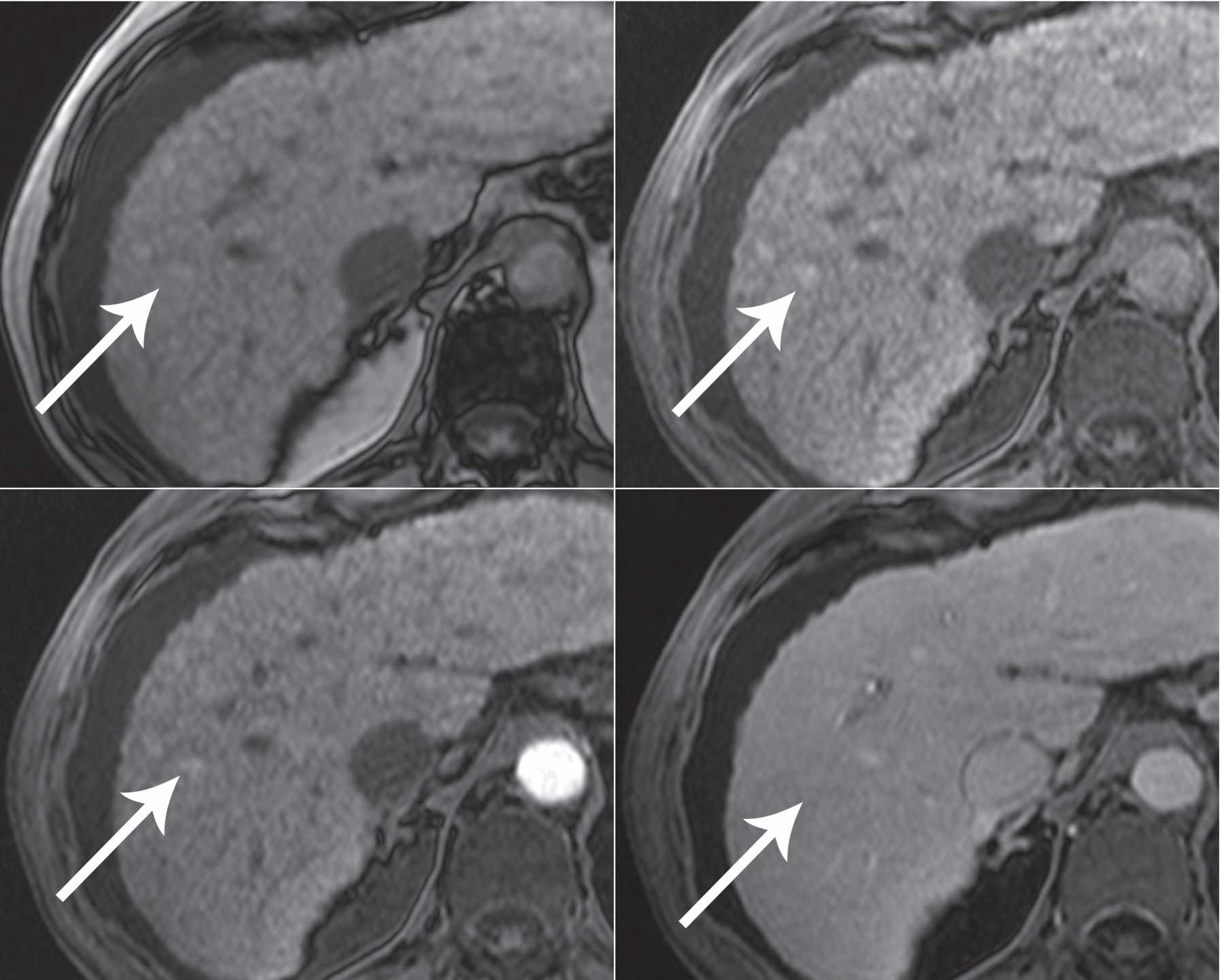
21 A 77-year-old man with chronic hepatitis B undergoes a screening MRI using conventional extracellular contrast agent. What is the most likely diagnosis?
Top row: In-phase and out-of-phase T1W. Bottom row: Arterial and delayed phase FS T1W+gad.
A. Hepatocellular carcinoma
B. Hepatocellular adenoma
C. Angiomyolipoma
D. Nodular steatosis
22a A 19-year-old man was injured in a motor vehicle collision. Which statement is TRUE regarding the management of the liver findings on CT?
A. Partial hepatic resection is indicated for extent of laceration.
B. Angiography is indicated for embolization of a pseuodaneurysm.
C. No intervention is needed if patient is hemodynamically stable.
D. Percutaneous catheter placement is indicated for subcapsular hematoma.
22b The patient was hemodynamically stable and managed conservatively. Within 24 hours, the patient developed jaundice, which prompted a HIDA scan. What is the diagnosis?
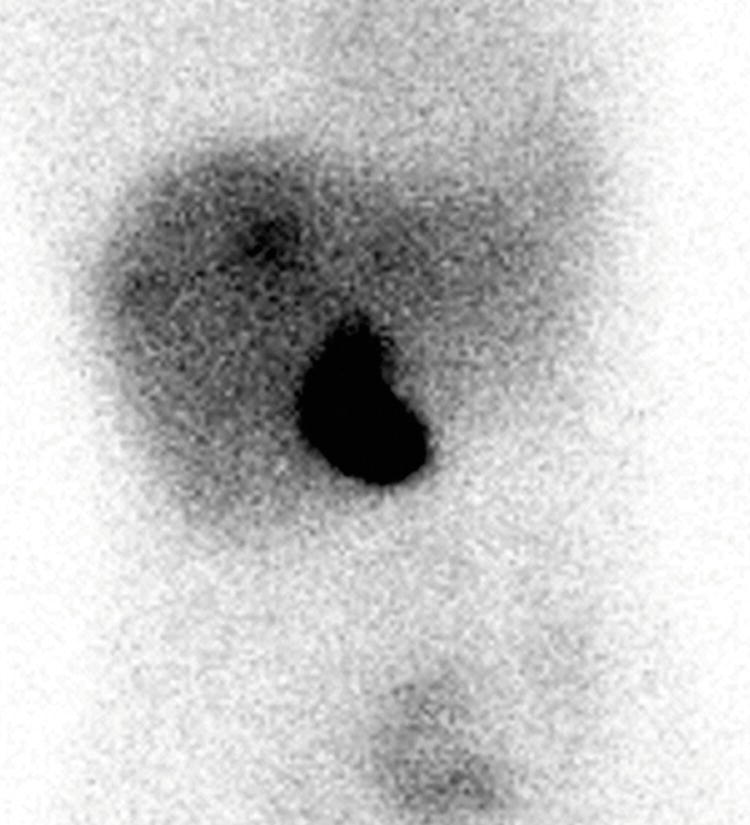
A. Intrahepatic bilomas
B. Intraperitoneal bile leak
C. Common bile duct obstruction
D. Gallbladder laceration
23 A 52-year-old woman undergoes a CT scan with images shown below. Imaging findings are consistent with:
A. Cholangiocarcinoma
B. Hemangioma
C. Lymphadenopathy
D. Portal vein occlusion
24a A 30-year-old woman is evaluated for a liver lesion that was incidentally noted at the time of a pelvic ultrasound. Which of the following statements is TRUE about the finding in the right lobe of the liver?
Top row: Noncontrast and arterial phase CT. Bottom row: Venous and delayed phase CT.
A. The finding demonstrates washout appearance and is most likely a malignancy.
B. The finding is likely a mass of hepatocellular origin.
C. The finding is likely a transient hepatic attenuation difference (THAD).
D. The finding demonstrates a central scar.
24b Hepatocellular adenomas in which of the following groups of patients have the highest risk of malignant transformation to hepatocellular carcinomas?
A. Women using oral contraceptives
B. Men
C. Patients with diabetes
D. Patients with steatosis in the background liver
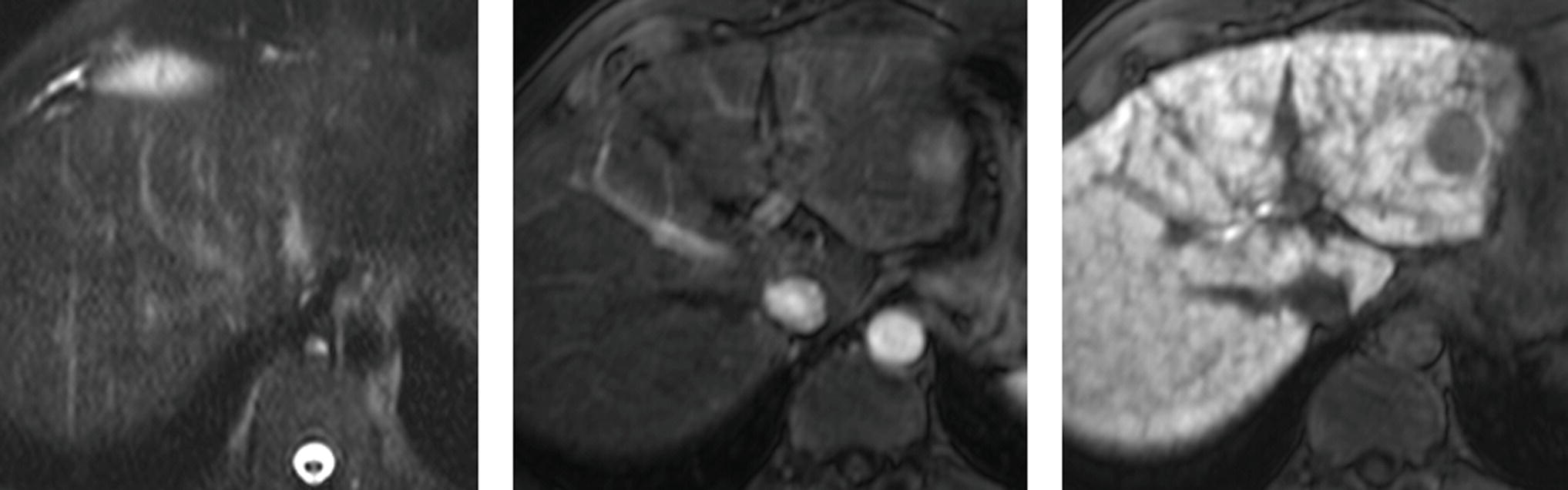
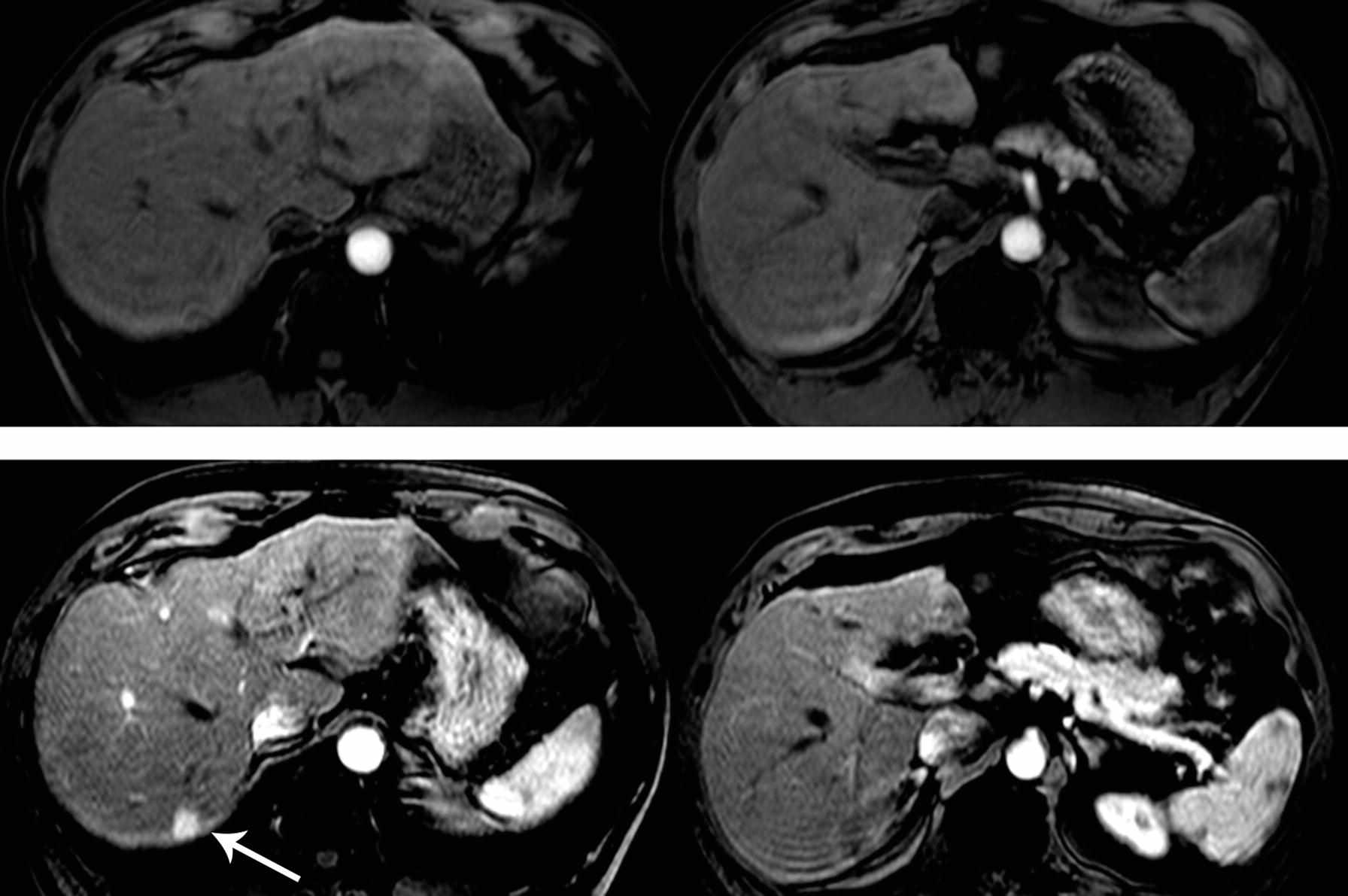
25a A 19-year-old woman was found to have elevated liver function tests. Workup included a liver MRI with hepatobiliary gadolinium contrast agent. Findings are most consistent with:
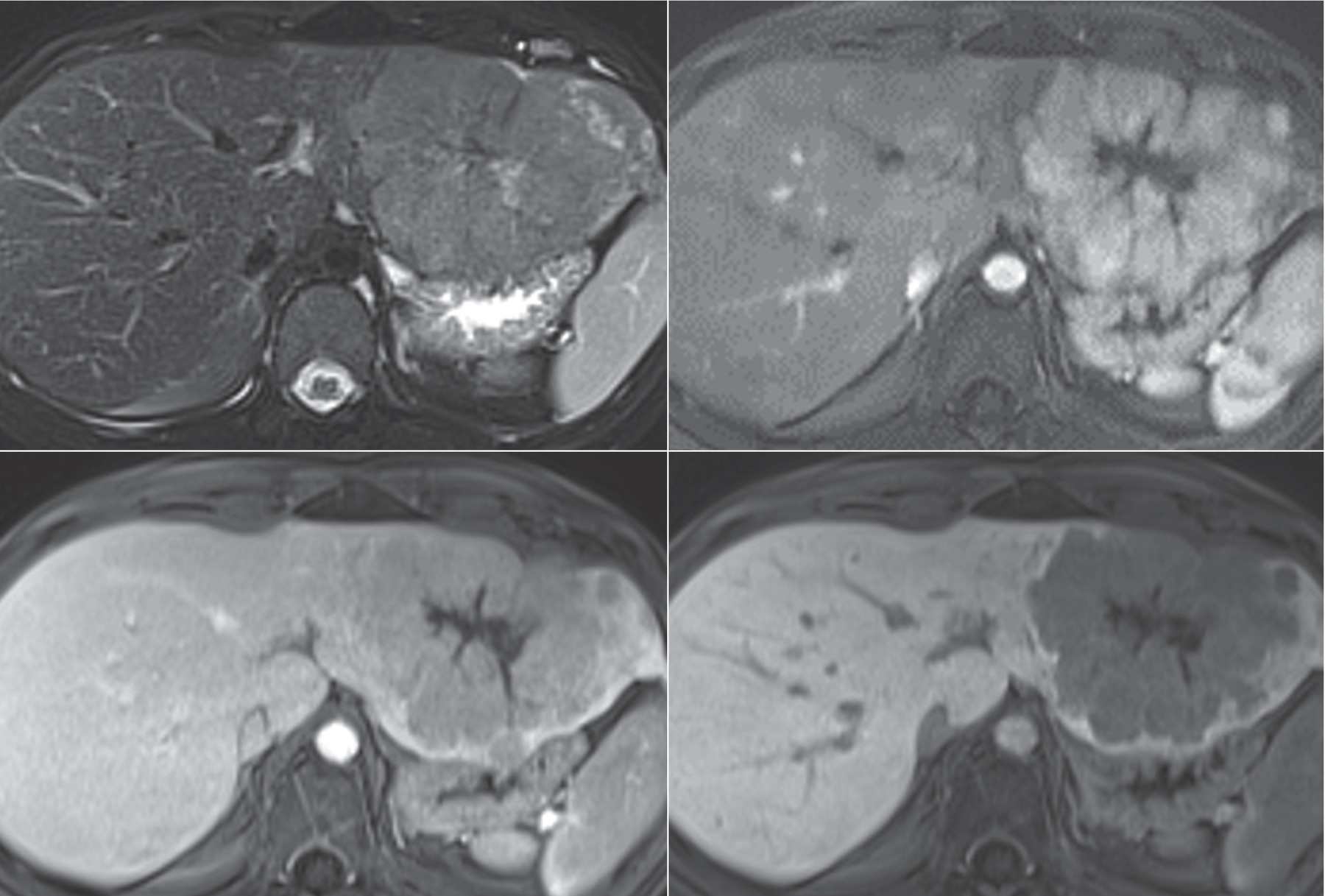
Top row: FS T2W and arterial phase FS T1W+hepatobiliary gad. Bottom row: Venous and hepatobiliary phase FS T1W+hepatobiliary gad.
A. Colon carcinoma metastasis
B. Giant cavernous hemangioma
C. Focal nodular hyperplasia
D. Fibrolamellar hepatocellular carcinoma
25b Which of the following statements is TRUE regarding fibrolamellar hepatocellular carcinoma (FHCC)?
A. Five-year survival is higher compared to conventional hepatocellular carcinoma.
B. Most patients are female.
C. The background liver is cirrhotic in the majority of cases.
D. There is a bimodal distribution affecting patients <40 and >60 years of age.
26 Which of the following is the most common benign liver tumor?
A. Hepatocellular adenoma
B. Focal nodular hyperplasia
C. Peliosis hepatis
D. Hemangioma
A. Congestive heart failure
B. Budd-Chiari syndrome
C. Arteriovenous malformation
D. Hepatic infarction
28 An MRI exam was performed in this 80-year-old woman with fever to further evaluate a liver mass seen on CT. What is the best explanation of findings on the (apparent diffusion coefficient) ADC map?
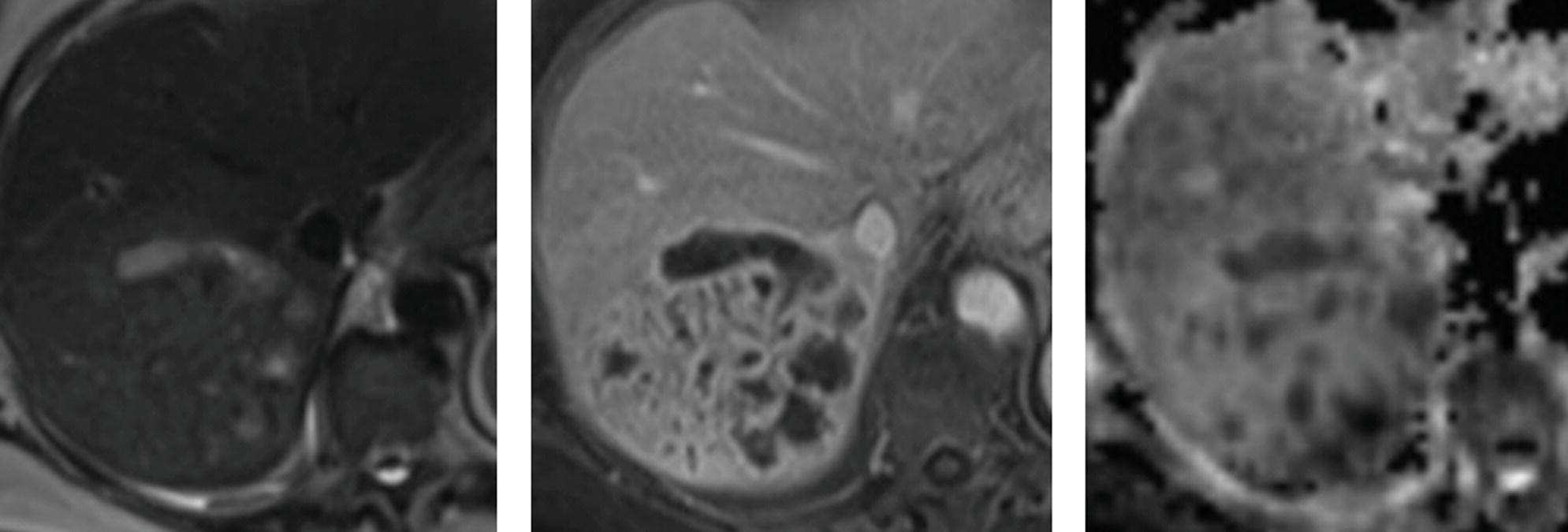
T2W, venous phase FS T1W+gad, and ADC map.
A. There is restricted diffusion in the enhancing soft tissue of this highly cellular neoplasm.
B. The foci of hypointensity on ADC map are due to gas.
C. There is restricted diffusion in the loculated fluid of this pyogenic abscess.
D. The foci of hypointensity on ADC map are due to iron deposition.
29 A 56-year-old woman presents with right upper quadrant pain and elevated liver function tests. Images from an MRI using conventional extracellular gadolinium contrast are shown below. What is the most likely diagnosis?
Top row: FS T2W and FS T1W. Bottom row: Arterial and delayed phase FS T1W+gad.
A. Old infarct
B. Hemangioma
C. Ascending cholangitis
D. Cholangiocarcinoma
A. Portal vein thrombosis
B. Biliary ductal dilatation
C. Segmental fatty sparing
D. Liver laceration
31 A 68-year-old man with a history of primary sclerosing cholangitis is status post left hepatectomy for resection of a cholangiocarcinoma. The abnormality shown on the multiphase CT images below is associated with:
Axial arterial, axial venous, and coronal arterial phase contrast-enhanced CT.
A. Decreased platelet count
B. Decreased hematocrit
C. Elevated CA19-9 level
D. Elevated white blood cell count
32 A 22-year-old woman presented to the emergency department with malaise and elevated liver function tests after recent excessive alcohol consumption. An ultrasound was performed. What is the most likely diagnosis?

A. Ascending cholangitis
B. Acute hepatitis
C. Fungal microabscesses
D. Hemangiomas
33a A 35-year-old woman with no history of chronic liver disease or underlying malignancy presents with abdominal pain. Based on the following MR images, what is the best description of the mass in the liver?
In-phase T1W, out-of-phase T1W, and FS T1W.
A. Fat-containing mass in the background of hepatic steatosis
B. Fat-containing mass in the background of hepatic hemosiderosis
C. Hemorrhagic mass in the background of hepatic steatosis
D. Hemorrhagic mass in the background of hepatic hemosiderosis
33b What is the most likely diagnosis of the mass in the previous question?
A. Focal nodular hyperplasia
B. Hepatocellular adenoma
C. Hepatocellular carcinoma
D. Metastatic disease
34 A 41-year-old woman who underwent a diagnostic procedure to evaluate suspected liver disease presents with acute severe epigastric pain. What finding is demonstrated involving the lateral segment left lobe on the CT?

A. Diffuse periportal edema
B. Focal fatty sparing
C. Subcapsular hematoma
D. Transient hepatic attenuation difference (THAD)
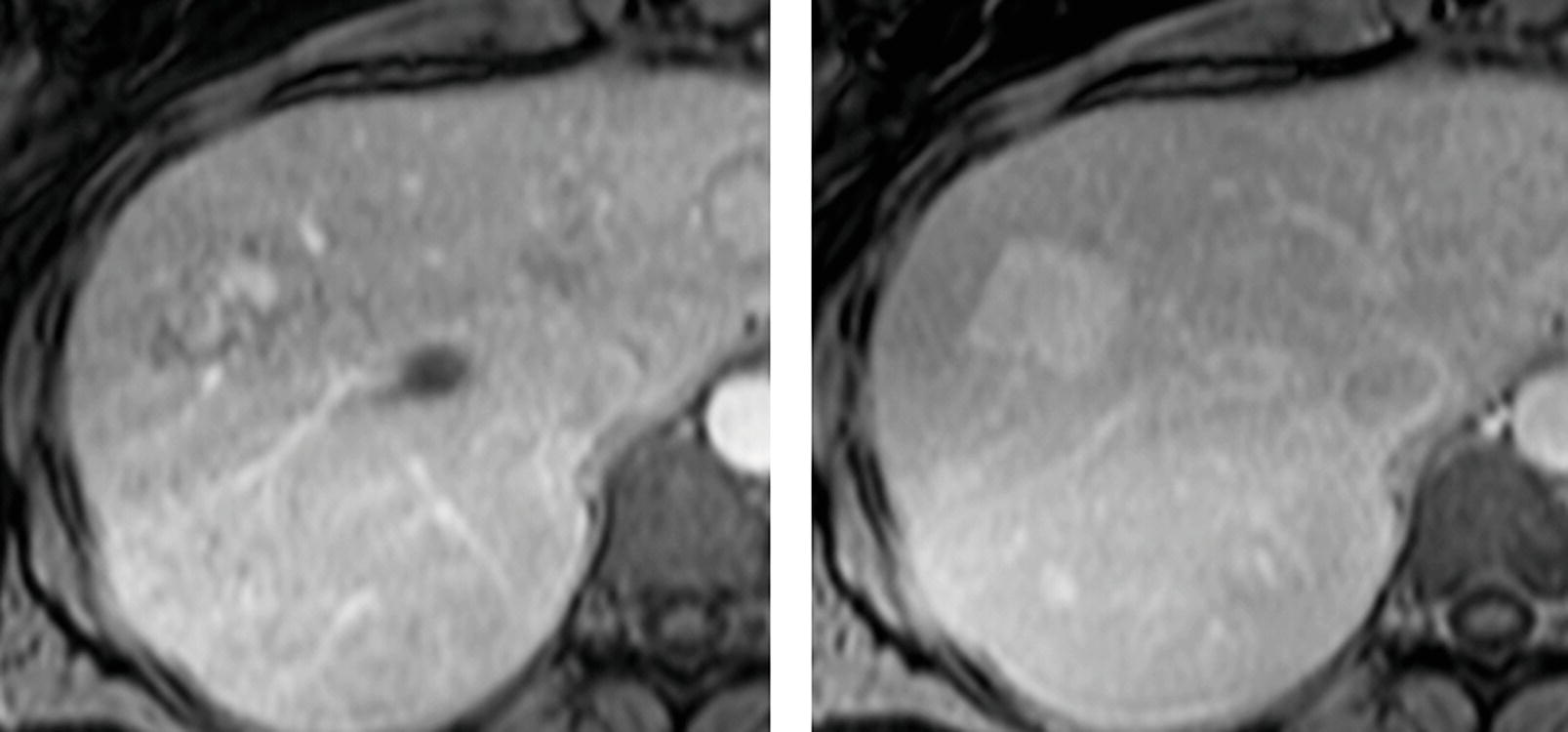
35 A 60-year-old man with cirrhosis underwent MRI exams 5 months apart. Arterial phase images of the current MRI exam are shown in the top row, and arterial phase images of the prior MRI exam are shown in the bottom row with a finding (arrow) in segment VII. The patient did not receive treatment between the exams. What is the most likely explanation for the appearance of the current exam in the top row?
A. The arterial phase on the current exam is not optimally timed for assessment of hypervascular neoplasms.
B. There has been spontaneous resolution of a dysplastic nodule.
C. There was a hepatocellular carcinoma that responded to treatment administered before both exams.
D. The finding the prior study was ghosting artifact from arterial pulsation no longer seen due to swapping of the phase- and frequency-encoding directions.
For the patients in questions 36 to 40, select the most likely underlying primary tumor (A to F) that is associated with the hepatic imaging findings. Each option may be used once or not at all.
A. Pancreatic ductal carcinoma
B. Neuroendocrine tumor
C. Non-small cell lung carcinoma
D. Breast carcinoma
E. Lymphoid tumor
F. Mucinous colorectal carcinoma
37 A 51-year-old man status post Whipple procedure.

Top row: Noncontrast and arterial phase. Bottom row: Venous and delayed phase.
38 A 41-year-old man status post liver transplant several months ago for cirrhosis and hepatocellular carcinoma. Arterial and venous phase CT as well as ultrasound images are shown.

39 A 77-year-old woman. Venous phase images are shown from two CT scans performed 12 months apart.
Initial scan and scan 12 months later after chemotherapy.
41 A patient with cirrhosis and hepatocellular carcinoma is undergoing evaluation for liver transplantation. Which of the following is a contraindication to transplantation according to the Milan criteria?
A. Encephalopathy
B. Refractory variceal hemorrhage
C. Malignant portal vein thrombus
D. Solitary HCC measuring 4 cm
42 The most common etiology of graft failure after liver transplant is
A. Posttransplant lymphoproliferative disorder
B. Vascular thrombosis
C. Biliary stricture
D. Rejection
43 A 63-year-old man with cirrhosis is status post CT-guided microwave ablation of a hepatocellular carcinoma in the right hepatic lobe. Two CT scans are shown. What is the most likely diagnosis?

Arterial phase CT scans 6 months after ablation and 14 months after ablation.
A. Hemangioma
B. Recurrent hepatocellular carcinoma
C. Abscess
D. Dysplastic nodule
A. Hemangioma
B. Simple cyst
C. Pulsatile flow artifact
D. Radiofrequency interference
45 A patient with a liver transplant was evaluated with ultrasound followed by angiography. The arrow indicates the location of spectral Doppler interrogation. What vascular complication is demonstrated?
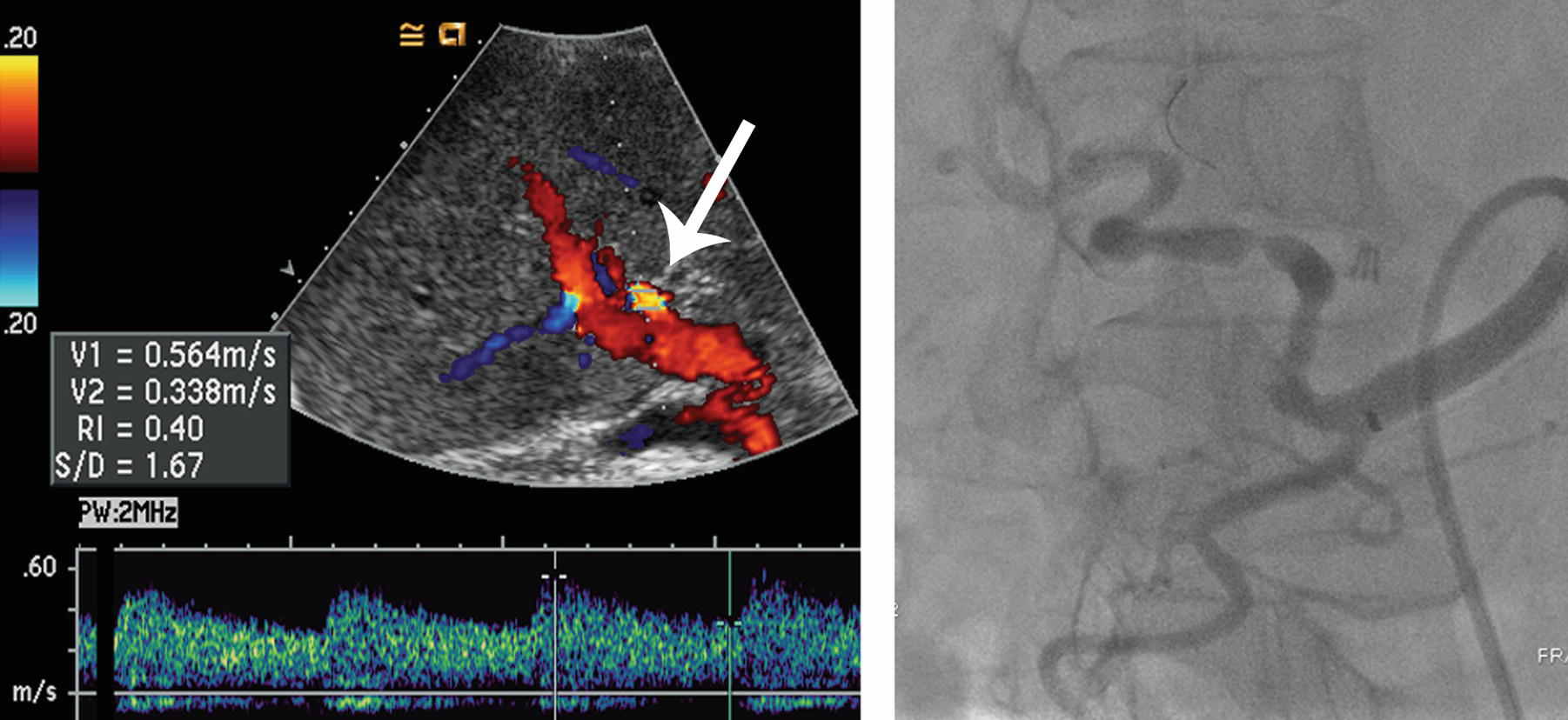
A. Hepatic artery stenosis
B. Portal vein thrombosis
C. Pseudoaneurysm
D. Arterioportal fistula
A. Kasabach-Merritt syndrome
B. Cushing syndrome
C. Carcinoid syndrome
D. Lambert-Eaton syndrome
For the patients in questions 47 to 50, select the most likely diagnosis (A to D) for the hepatic abnormalities. Each option may be used once, more than once, or not at all.
A. Siderotic nodule
B. Regenerative nodule, nonsiderotic
C. Nodular steatosis
D. Infarct
47 A 44-year-old woman with end-stage liver disease now with abdominal pain. Images from a CT scan and MRI are shown. A transjugular intrahepatic portosystemic shunt is partially visualized in the right lobe.
Venous phase CT, in-phase T1W MRI, and out-of-phase T1W MRI.
48 An MRI performed with conventional extracellular contrast agent is shown.
Top row: Out-of-phase T1W and FS T1W. Bottom row: Arterial and delayed phase FS T1W+gad.
49 A 39-year-old man with testicular cancer status post retroperitoneal nodal dissection. Postoperative course was complicated by hemoperitoneum. Images from two CT scans are shown.
Venous phase CT followed by noncontrast CT 1 month later.
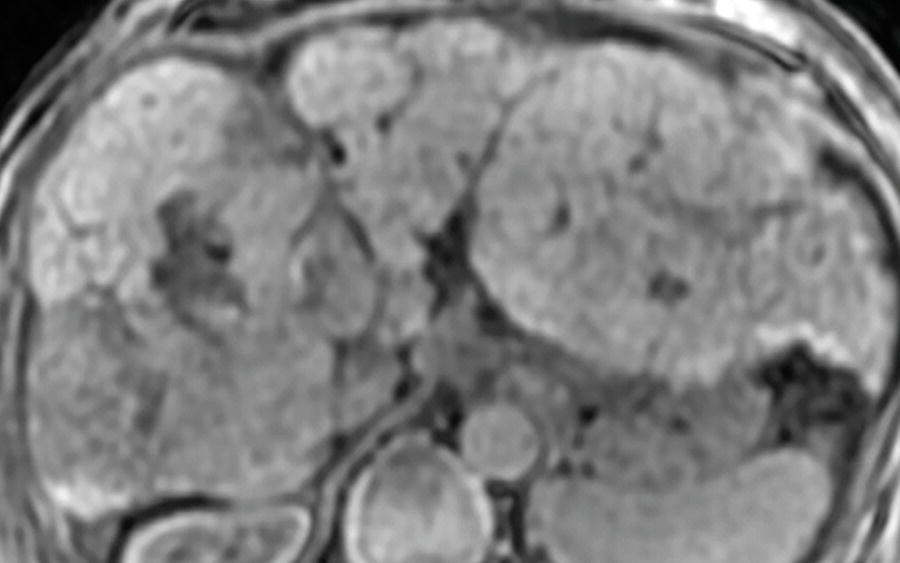
50 A 53-year-old man with chronic hepatitis B infection.
Top row: In-phase and out-of-phase T1W. Bottom row: FS T2W and arterial phase FS T1W+gad.
A. Moiré fringes.
B. Focal fatty infiltration.
C. Ascites.
D. Uneven fat saturation.
52 A patient with cirrhosis underwent abdominal evaluation with ultrasound followed by CT. A spectral Doppler ultrasound image and two arterial phase CT images are shown. What is the finding?
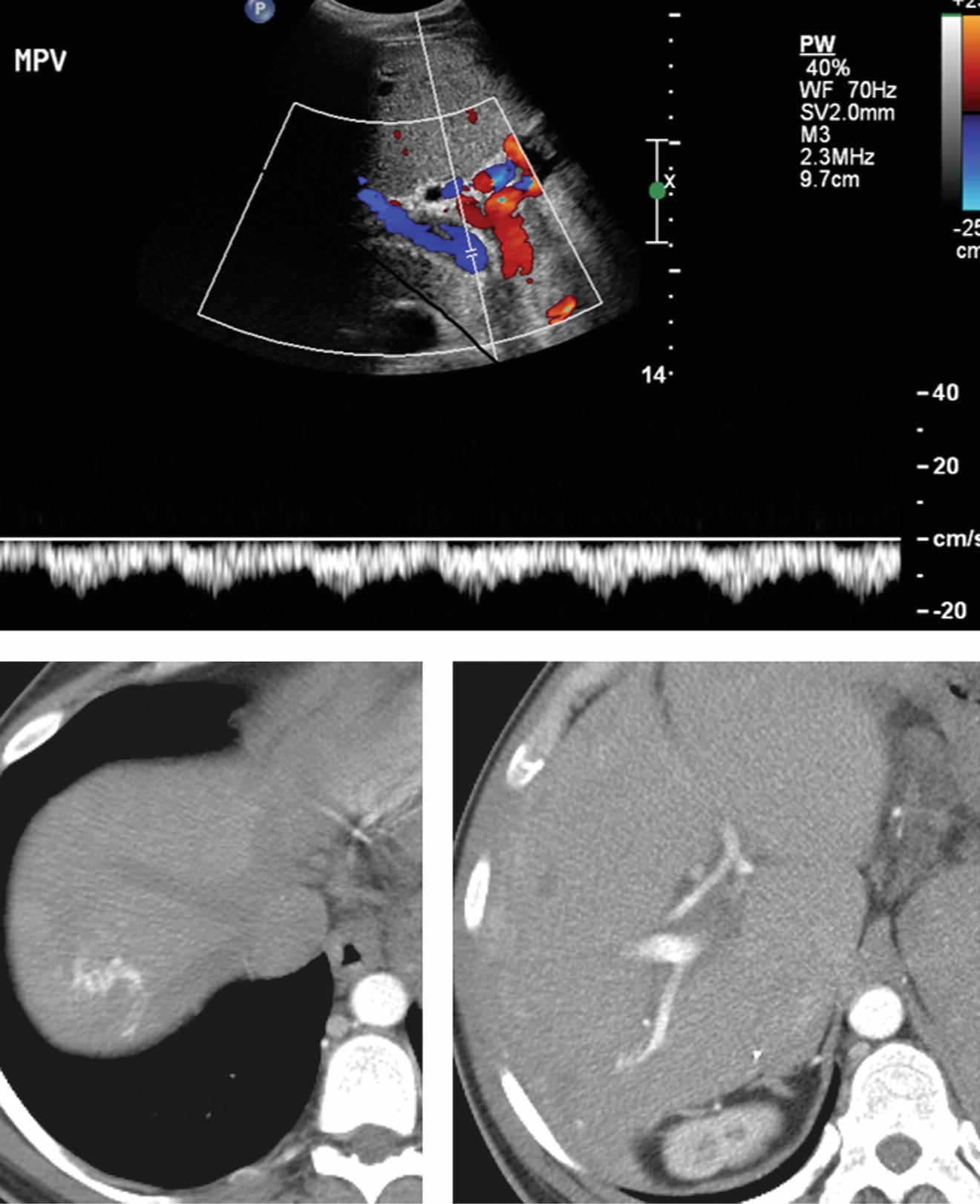
A. Hepatopedal flow in the portal vein
B. Respiratory variation in the portal vein
C. Arterioportal shunting
D. Cavernous transformation of the portal vein
53a A 46-year-old woman underwent MRI for multiple liver lesions found on ultrasound. Arterial and delayed phase FS T1W images from an MRI performed using conventional extracellular contrast agent are shown. This pattern of enhancement is most commonly identified with which of the following lesions?
A. Cavernous hemangioma
B. Peliosis hepatis
C. Lymphoma
D. Pseudoaneurysm
53b The organisms responsible for the most common form of peliosis hepatis seen in AIDS patients are species of:
A. Bartonella
B. Echinococcus
C. Ascaris
D. Cryptococcus
ANSWERS AND EXPLANATIONS
1 Answers: A4; B6; C7; D3; E1; F10; G2; H11; I9; J8; K5; L12.
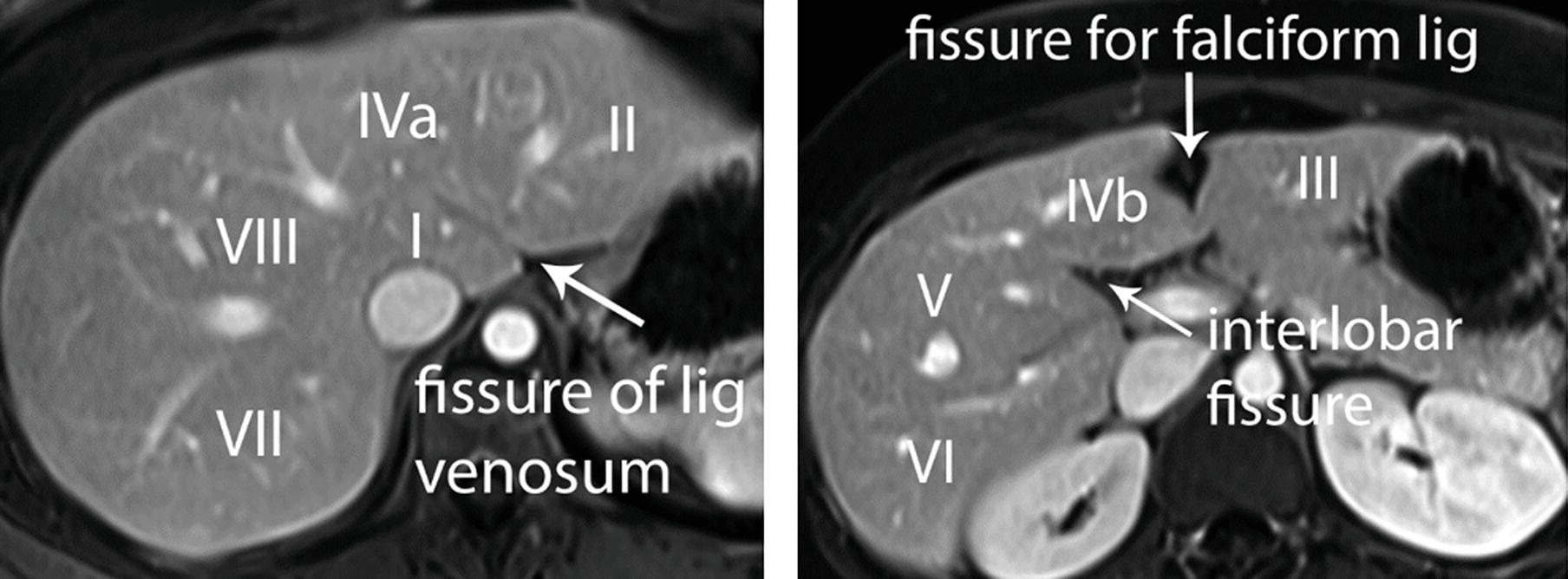
An understanding of hepatic lobar and segmental anatomy is essential in reporting to aid treatment planning. The liver is divided into right, left, and caudate lobes. The right lobe is subdivided into anterior and posterior segments and the left lobe into medial and lateral segments. The main hepatic veins are located in between segments of the liver. The portal triads (composed of the portal veins, hepatic arteries, and bile ducts) are located within segments of the liver. The Bismuth-Couinaud system is commonly used to provide a segmental nomenclature for localizing focal hepatic lesions. Vertically oriented planes along the right, middle, and left hepatic veins are maintained. These vertical planes intersecting a horizontal plane at the level of the right and left portal veins separate the liver into nine segments.
Segment I is the caudate lobe, located posterior to the fissure for the ligamentum venosum. Functionally, it is an autonomous part of the liver and has a separate blood supply, venous drainage, and biliary drainage.
The fissure for the ligamentum venosum is a coronally or obliquely oriented well-defined fissure. A normal variant accessory or replaced left hepatic artery from the left gastric artery can be seen running through this fissure.
The interlobar fissure (fissure of the gallbladder) separates the right and left lobes.
The fissure for the falciform ligament (fissure for the ligamentum teres) is located in the inferior aspect of the left hepatic lobe. The remnant umbilical vein “recanalizes” in the setting of portal hypertension and can be seen running through this fissure.
References: Boll DT, Merkle EM. Liver: normal anatomy, imaging techniques, and diffuse diseases. In: Haaga JR, Lanzieri CF, Gilkeson RC (eds). CT and MRI imaging of the whole body, 5th ed. Philadelphia, PA: Elsevier, 2009:1953–2040.
Ding A, Kulkarni N, Fintelmann FJ, et al. Liver: normal anatomy and examination techniques. In: Gore RM, Levine MS (eds). Textbook of gastrointestinal radiology, 4th ed. Philadelphia, PA: Elsevier Saunders, 2015:1471–1497.
2 Answer D.The liver is diffusely hyperdense in this patient with cardiac disease. Normal density is 45 to 65 HU on a noncontrast CT scan obtained with conventional kVp of 120. At visual inspection, it should appear similar to the spleen, which is about 35 to 55 HU. Diffuse hepatic hyperdensity can be caused by iodine deposition in patients treated with the cardiac antiarrhythmic drug amiodarone, which is 37% iodine by weight. This hyperdensity does not always indicate toxicity, and patients may be asymptomatic. However, if injury is severe, the patient may develop steatosis and cirrhosis. If there is pulmonary involvement, interstitial fibrosis and high-density pulmonary opacities may be seen.
Other causes of diffuse hepatic hyperdensity include hemochromatosis (iron deposition), Wilson disease (copper deposition), gold therapy, and glycogen storage disease. Thorotrast was associated with deposition of high density in a characteristic reticular pattern within the liver and spleen. The use of Thorotrast, a radioactive contrast agent, was discontinued in the 1950s when it was discovered to be carcinogenic. Total parenteral nutrition and radiation therapy are more commonly causes of steatosis and decreased liver density. Hepatorenal syndrome is unrelated to liver hyperdensity. It refers to renal failure caused by cirrhosis or fulminant hepatitis, leading to portal hypertension and ascites.
References: Coy, DL, Kolokythas O. Chapter 9: Liver and biliary. In: Lin E, Coy DL, Kanne JP (eds). Body CT: the essentials. New York, NY: McGraw-Hill, 2015.
Morgan T, Qayyum A, Gore RM. Chapter 89: Diffuse liver disease. In: Gore RM, Levine MS (eds). Textbook of gastrointestinal radiology, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2015:1629–1675.
3 Answer A.MRI is the imaging modality of choice to evaluate focal hepatic lesions, as reflected in the ACR Appropriateness Criteria. This series of questions reviews the classic appearances of some primary hepatic tumors on MRI. There is a well-circumscribed lesion in hepatic segment VII, which is very bright on the T2W image approaching signal intensity of cerebrospinal fluid, consistent with the “light bulb” sign. The mass demonstrates peripheral, nodular, discontinuous enhancement, followed by centripetal fill-in on delayed phase. These features are diagnostic for cavernous hemangioma. Fill-in may be partial or complete in hemangiomas. Hemangiomas are dilated venous channels with hepatic arterial supply. The great majority are asymptomatic and require no follow-up or treatment.
References: Boland GWL, Halpert RD. Chapter 6: Liver. In: Boland GWL, Halpert RD (eds). Gastrointestinal imaging: the requisites, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2014:218–290.
Cogley JR, Miller FH. MR imaging of benign focal liver lesions. Radiol Clin North Am 2014;52:657–682.
4 Answer D.This mass is a hepatocellular carcinoma (HCC). Signal intensity of the mass in segment VIII is similar to surrounding liver on both noncontrast T1W and T2W images, a clue that the tumor may be of hepatocellular origin (i.e., an HCC, focal nodular hyperplasia, or hepatocellular adenoma). The mass enhances on the arterial phase and demonstrates washout appearance as well as capsule appearance on delayed phase. These features are classic for HCC in this patient with cirrhosis. Additional imaging features that may be also present in HCC are intralesional fat, restricted diffusion, and portal vein tumor thrombus.
MRI is the most sensitive and specific imaging modality for the diagnosis of HCC. Awareness of patient demographics and clinical history is critical in the evaluation of hepatic lesions. In the presence of cirrhosis, a high index of suspicion for HCC should be maintained for any enhancing liver lesion. Washout appearance is an important imaging feature in the identification of classic HCC. A mass demonstrates washout appearance if it initially appears iso- to hyperintense to surrounding liver and then appears hypointense to surrounding liver on a later phase. “Washout” is often a misnomer because this appearance is predominantly due to increase in enhancement of the surrounding liver rather than loss of signal intensity by the mass itself.
References: ACR Appropriateness Criteria: Liver lesion— initial characterization. American College of Radiology website. https://acsearch.acr.org/docs/69472/Narrative. Published 1998. Updated 2014. Accessed April 4, 2015.
Choi JY, Lee JM, Sirlin CB. CT and MR imaging diagnosis and staging of hepatocellular carcinoma: Part II. Extracellular agents, hepatobiliary agents, and ancillary imaging features. Radiology 2014;273(1):30–50.
5 Answer E.This neoplasm is a mass-forming cholangiocarcinoma. The MRI demonstrates a large mass that shows sparse early enhancement and then heterogeneous progressive enhancement on later phases. Delayed enhancement is a feature suggesting a desmoplastic tumor such as a cholangiocarcinoma. Its hypointensity is very distinct from the surrounding liver parenchyma on T1W imaging, a clue that the tumor may not be of hepatocellular origin.
Cholangiocarcinoma is a malignant tumor arising from the biliary tree and represents the second most common primary malignancy of the liver. It can be categorized into three types based on morphology: mass-forming, periductal infiltrating, and intraductal growth types. Mass-forming cholangiocarcinoma may be seen with or without biliary ductal dilation. There may be associated hepatic capsular retraction, satellite nodules, and vascular encasement. It can be mistaken for a hemangioma due to its progressive delayed enhancement but lacks the well-defined puddles of peripheral discontinuous nodular enhancement seen with cavernous hemangiomas. In addition, the mass lacks the characteristic “light bulb” T2 hyperintensity of a hemangioma.
References: Chung YE, Kim MJ, Park YN, et al. Varying appearances of cholangiocarcinoma: radiologic-pathologic correlation. Radiographics 2009;29(3):683–700.
Sainani NI, Catalano OA, Holalkere NS, et al. Cholangiocarcinoma: current and novel imaging techniques. Radiographics 2008;28(5):1263–1287.
6 Answer C.This patient has a focal nodular hyperplasia (FNH). There is an arterial-enhancing mass which retains contrast agent at 20 minutes on this MRI performed with Eovist hepatobiliary contrast agent. The mass is isointense on precontrast T2W image with exception of the small central scar, which is classically T2 hyperintense. All of the other answer choices are typically hypointense to the liver on the hepatobiliary phase.
If a conventional extracellular contrast agent (not shown here) is used, homogeneous arterial enhancement is seen, classically followed by venous and delayed phase isointensity. A prominent feeding vessel extending toward the central scar is sometimes identified on arterial phase. The central scar may enhance on the delayed phase when conventional extracellular contrast is used. Focal nodular hyperplasia is a benign mass representing a heptaocellular hyperplastic response to a pre-existing arterial malformation. It is most common in women of reproductive age. In 20% of cases, there are multiple lesions.
Differentiation from hepatocellular adenoma (HCA), another benign hypervascular hepatocellular tumor found in young women, is important as no other treatment is required for FNH, while HCA may require follow-up or intervention for hemorrhage, or rarely, malignant transformation. MRI with hepatobiliary contrast agent has been found to be highly sensitive and specific for differentiating FNH and HCA in this patient population. Because FNH contains normal functioning hepatocytes, it accumulates hepatobiliary contrast agent and remains iso- to hyperintense to the liver on 20-minute hepatobiliary phase images. In contradistinction, HCAs are hypointense on hepatobiliary phase.
References: Khosa F, Khan AN, Eisenberg RL. Hypervascular liver lesions on MRI. AJR Am J Roentgenol 2011;197(2):W204–W220.
Silva AC, Evans JM, McCullough AE, et al. MR imaging of hypervascular liver masses: a review of current techniques. Radiographics 2009;29(2):385–402.
7 Answer D.This is the expected appearance of a hepatocellular carcinoma (HCC) on an MRI performed with hepatobiliary contrast agent. The mass in the left lobe of the liver shows arterial enhancement. It is dark compared to surrounding liver on the hepatobiliary phase. There is evidence of cirrhosis with bands of fibrosis which are also hypointense on hepatobiliary phase. Other hypervascular masses such as hemangioma, hepatocellular adenoma (HCA), focal nodular hyperplasia (FNH), and metastasis are significantly less common in the cirrhotic liver compared to the general population. The lesion is isointense to the liver on T2 images, with no evidence of “light bulb” T2 hyperintensity to suggest a hemangioma. This 51-year-old man is not in the right demographic for HCA or FNH, lesions which most commonly occur in premenopausal women.
The role of hepatobiliary contrast agents in the patients at risk for HCC continues to evolve. In general, isointensity or hyperintensity on hepatobiliary phase is reassuring, suggestive of a benign finding such as regenerative nodule, dysplastic nodule, or arterioportal shunt with transient hepatic intensity difference (THID). Borders of an HCC may appear more sharply marginated on hepatobiliary phase than on other sequences, helping in the delineation and measurement of heterogeneous, infiltrative lesions.
References: Choi JY, Lee JM, Sirlin CB. CT and MR imaging diagnosis and staging of hepatocellular carcinoma: Part II. Extracellular agents, hepatobiliary agents, and ancillary imaging features. Radiology 2014;273(1):30–50.
Jhaveri K, Cleary S, Audet P, et al. Consensus statements from a multidisciplinary expert panel on the utilization and application of a liver-specific MRI contrast agent (gadoxetic Acid). AJR Am J Roentgenol 2015;204(3):498–509.
8 Answer D.If a hepatobiliary agent such as gadoxetate disodium (Eovist—Bayer HealthCare) is used, hypointensity on the 20-minute hepatobiliary phase is considered an ancillary feature that favors HCC according to LI-RADS (Liver Imaging Reporting and Data System). Ancillary features may upgrade suspicion for hepatocellular carcinoma no higher than category LI-RADS category 4 (probably HCC). Some other ancillary features that would favor HCC include diffusion restriction, nodule-in-nodule architecture, intralesional fat, and growth less than threshold.
LI-RADS was developed by a multidisciplinary committee supported by the American College of Radiology (ACR) to standardize interpretation and reporting of multiphase CT and MRI exams of the liver. LI-RADS is applicable to the patient population with cirrhosis or chronic hepatitis B and/or C, who are at risk for hepatocellular carcinoma (HCC). The algorithm for LI-RADS version 2014 is an interactive graphic on the ACR Web site with definitions, descriptions, and examples. LI-RADS categories range from LR-1 (100% certainty that observation is benign) to LR-5 (100% certainty that observation is HCC). When an observation does not meet criteria for other categories, it is designated LR-3 indicating intermediate probability for HCC.
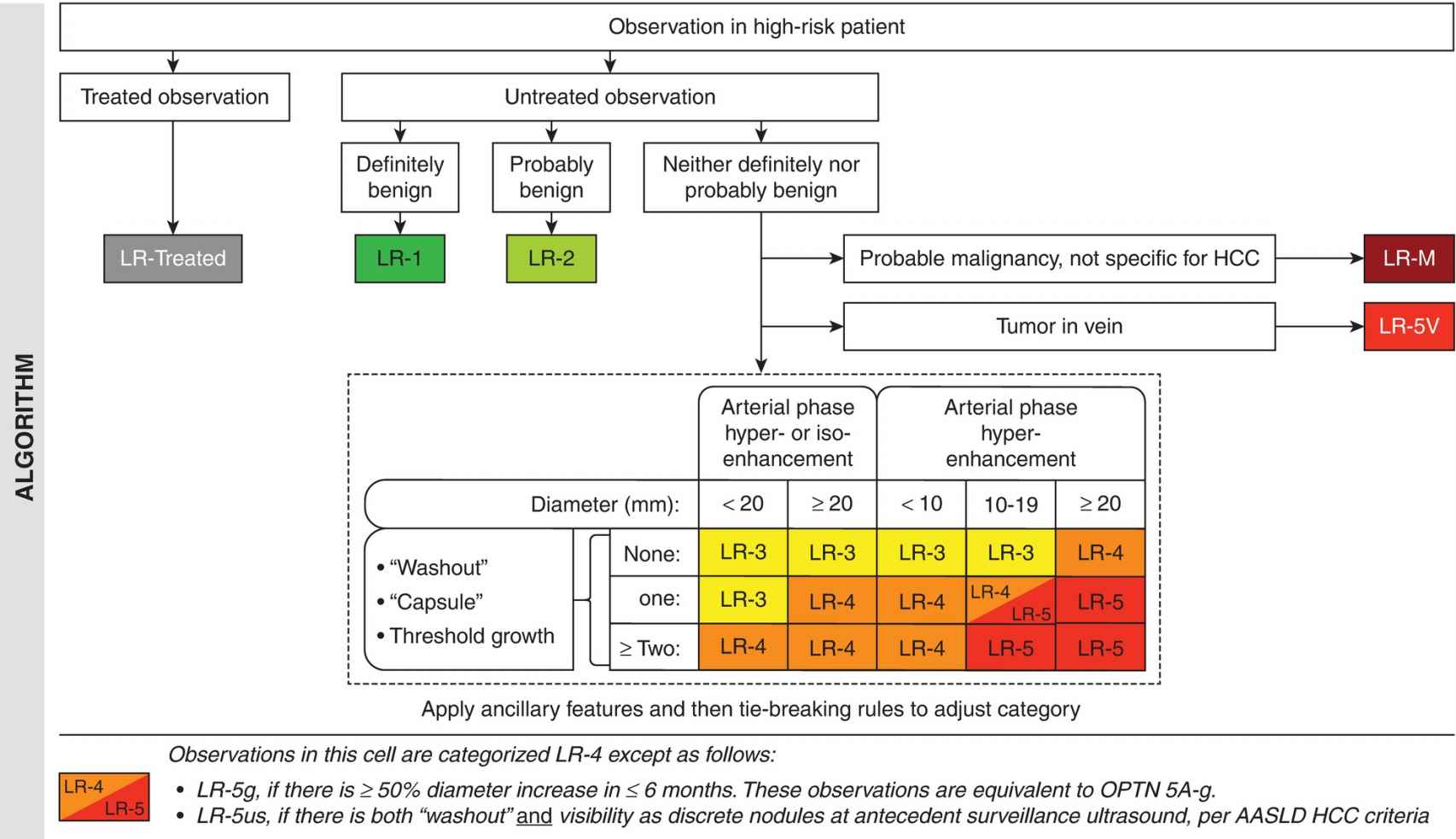
Reproduced with permission from the American College of Radiology. Liver Imaging Reporting and Data System version 2014. Accessed April 2015, from http://www.acr.org/Quality-Safety/Resources/LIRADS.
Major features for HCC in LI-RADS include “washout,” “capsule,” and threshold growth. Arterial enhancement and size thresholds are also included in major criteria, with masses ≥2 cm most worrisome. “Washout” and “capsule” specified in quotation marks (or washout appearance and capsule appearance) are the terms preferred by LI-RADS. This serves as a reminder that these terms are visual cues, which do not necessarily represent true loss of contrast enhancement on imaging or a true capsule at pathology.
Hepatobiliary phase hypointensity is not considered “washout.” On an MRI performed with a hepatobiliary contrast agent, it may only be appropriate to refer to washout appearance on the earliest venous phases in the dynamic portion of the exam (before 3 minutes) before the hepatobiliary phase dominates.
References: American College of Radiology. Liver Imaging Reporting and Data System version 2014. Accessed July 2015, from http://www.acr.org/Quality-Safety/Resources/LIRADS
Liu YI, Shin LK, Jeffrey RB, et al. Quantitatively defining washout in hepatocellular carcinoma. AJR Am J Roentgenol 2013;200(1):84–89.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree