Type 1: segmental or diffuse fusiform dilatation of the common bile duct
Type 2: diverticulum of the common bile duct
Type 3: choledochocele
Type 4: multiple cystic dilatations of the intrahepatic and extrahepatic bile ducts
Type 5: multiple cystic dilatations of the intrahepatic bile ducts (Caroli disease)
The most important aspect of the surgical treatment of choledochal cysts is determining the presence of intrahepatic bile duct anomalies and the relationship between the distal end of the choledochal cyst and the pancreatic duct and common channel (Takeshi et al. 2006). Therefore, the role of preoperative MRCP is to confirm the type of choledochal cyst and determine the presence of APBDU and biliary tract anomalies. Although hepatobiliary scintigraphy and CT can be used for the diagnosis, they have limitations in the demonstration of APBDU. On operative cholangiography, precise anatomy of the biliary tract and APBDU can be confirmed (Fig. 22.8).
22.1.4.2.4 Caroli Disease
Caroli disease is a congenital non-obstructive dilatation of intrahepatic bile ducts. It can present with only bile duct ectasia or be associated with hepatic fibrosis (Caroli syndrome). Diffuse, lobar, or segmental distribution of intrahepatic bile duct dilatations is seen in the liver (Fig. 22.9). A well-known diagnostic clue is the intraluminal portal vein sign (US) or central dot sign (contrast-enhanced CT) (Pariente 2005; Siegel 2011). Classic cholangiographic appearance obtained by conventional ERCP or PTC is bulbous or saccular dilatations of intrahepatic bile ducts. However, these findings can be noninvasively demonstrated by MRCP even in children. On US, CT, and MRI, sludge or calculi can be detected within the dilated bile ducts.
22.1.4.2.5 Bile-Plug Syndrome
Bile-plug syndrome is one of the causes of extrahepatic biliary obstruction in neonates and infants and associated with many etiological factors. The clinical and laboratory findings are similar to other conditions with neonatal cholestasis. Imaging studies are important for making a correct diagnosis and guiding the treatment plan. US shows the dilated gallbladder with or without echogenic bile sludge and concentric dilatation of the common bile duct filled with echogenic bile sludge. Inspissated bile is more echogenic than bile sludge within the gallbladder. The affected common bile duct may blend with the surrounding pancreas parenchyma, causing difficulty in determining the dilated common bile duct (Gubernick et al. 2000). During conservative treatment, the bile plug may be expelled spontaneously, but if it is not, surgical irrigation should be considered.
On MRCP, the extrahepatic bile duct is diffusely dilated. A bile plug filled in the bile duct can be detected as variable-shaped, low signal-filling defects on MRCP. So MRCP is useful in evaluating the presence and extent of the bile plug. On T1-weighted image, the bile plug also has low-signal intensity, and static bile filled in the dilated common bile duct and gallbladder may have high signal intensity (Fig. 22.10).
22.1.4.2.6 Spontaneous Perforation of the Bile Duct
In neonates or infants with spontaneous perforation of the bile duct, the classic presentation is that of a previously healthy infant who develops progressive abdominal distension, irritability, and fluctuating mild jaundice (Xanthakos et al. 2003). The pathogenesis of spontaneous perforation of the bile duct is unknown, although numerous etiologies have been proposed, such as congenital weakness of the CBD, ischemia, stones, infection, distal bile duct stenosis, inspissated bile, and pancreatic reflux from anomalous pancreaticobiliary ductal union. To avoid the delayed diagnosis, this condition should be considered in the differential diagnosis of jaundice in infancy. US plays a limited role in the diagnosis of this entity. If the extrahepatic bile duct is not dilated, it is difficult to suspect this condition. The ascites and loculated fluid collection around the porta hepatis may be helpful in the diagnosis. Hepatobiliary scintigraphy confirms the diagnosis when the radioisotope is leaked from the region of the porta hepatis into the peritoneal cavity. It is the most useful imaging modality and should be used on patients suspected of having bile duct perforation (Fig. 22.11), but because of limited spatial resolution, combined anomalies of the bile duct cannot be evaluated on hepatobiliary scintigraphy. MRCP can depict the bile duct and pancreatic duct anomalies such as choledochal cyst, anomalous pancreaticobiliary ductal union, distal bile duct stenosis, and loculated fluid collection or pseudocyst formation at the porta hepatis (Lee et al. 2010).
22.1.4.2.7 Cholelithiasis and Cholecystitis
In children, development of cholelithiasis may be idiopathic or associated with obstructive biliary anomaly, total parenteral nutrition, furosemide, hemolytic anemia, etc.. The best diagnostic tool for cholelithiasis is US. The typical US appearance is echogenic stone with posterior acoustic shadowing and its positional change (Pariente 2005; Siegel 2011). The differentiation between small, non-shadowing stones and bile sludge is sometimes difficult on US. Besides typical US findings, the sonographic Murphy sign and gallbladder wall thickening and gallbladder hydrops are suggestive of acute cholecystitis (Fig. 22.12) (Siegel 2011).
22.1.4.3 Hepatic Tumors
22.1.4.3.1 Hepatoblastoma
Hepatoblastoma is the most common primary liver tumors in young children with a peak presentation at 1–2 years of age. There is an increased risk of hepatoblastoma in Beckwith-Wiedemann syndrome, hemihypertrophy, familial adenomatosis polyposis coli, and premature or low-birth-weight infants. It is a large, well-defined, and heterogeneous liver mass in an infant. Serum AFP is typically raised in 90 % of the patients.
On US, it is a well-defined solid mass with a spoke-wheel appearance due to fibrous septa, heterogeneous echogenicity due to hemorrhage or necrosis, and typically hypervascular on Doppler US (Jha et al. 2009). CT demonstrates a large, heterogeneous, and hypoattenuating mass with heterogeneous enhancement. Calcification can be seen in 55 % of patients. On MRI, the mass shows variable signal intensity on T2-weighted images due to hemorrhage (Figs. 22.13 and 22.14).
22.1.4.3.2 Hepatic Hemangioendothelioma
Hepatic hemangioendothelioma is the most common vascular hepatic tumor seen during the first year of life. It is a heterogeneous and hypervascular mass and can be associated with cutaneous hemangioma, congestive heart failure, and consumptive coagulopathy (Kasabach-Merritt syndrome). It is usually associated with mild elevations in AFP levels (around 10,000 units), and it tends to involute spontaneously without therapy over a course of months to years.
On US, it is a complex hypoechoic or hyperechoic mass. It has a high flow on Doppler US. CT demonstrates heterogeneously hypoattenuating mass with prominent vessels. It can be solitary or multiple. An abrupt decrease in aortic caliber distal to celiac axis can be seen on CT. MRI also shows a very high-signal intensity mass on T2-weighted images with flow voids. On contrast-enhanced CT or MRI, there is a characteristic intense, nodular peripheral rim enhancement with central progression (Figs. 22.15 and 22.16) (Jha et al. 2009). During follow-up, the tumor decreases in size with increased internal calcification.
22.1.4.3.3 Mesenchymal Hamartoma
Mesenchymal hamartoma is the second most common benign hepatic tumor in children who are usually less than 2 years of age. Imaging findings depend on the predominance of cysts or stroma (mesenchymal elements). Multiple variable-sized cysts with various amounts of stroma are seen on US or CT (Fig. 22.17) (Jha et al. 2009). Calcification or hemorrhage is not generally seen. On MRI, this tumor shows variable signal intensity on T1-weighted images depending on variable protein content.
22.1.4.3.4 Focal Nodular Hyperplasia
Focal nodular hyperplasia (FNH) is uncommon in children (5 % of benign liver tumors) and more common in girls. It may develop based on a congenital vascular malformation or due to iatrogenic hepatic vascular abnormalities.
On US, it is a non-encapsulated, solitary mass with variable echogenicity. The central scar is seen in about one-third of the cases. It is typically very similar to surrounding liver parenchyma on CT and MRI. After contrast enhancement, it shows an early and rapid enhancement in the arterial phase with a rapid washout. Retained contrast can be seen in the central scar on delayed phase which is characteristic for FNH (Fig. 22.18) (Jha et al. 2009).
22.2 Pancreatic Disease
22.2.1 Anatomy and Development
The pancreas forms from the embryonic foregut and is therefore of endodermal origin. Pancreatic development begins with the formation of ventral and dorsal buds. Each structure communicates with the foregut through a duct. The ventral pancreatic bud becomes the head and uncinate process and comes from the hepatic diverticulum. Also, differential rotation and fusion of the ventral and dorsal pancreatic buds result in the formation of the definitive pancreas.
US appearance of the normal pancreas varies widely in children (Nijs et al. 2005). It is typically isoechoic or slightly hyperechoic than the liver. It is homogeneous with variable soft-tissue attenuation on CT. Pancreatic tumors, whether benign or malignant, are rare in children.
22.2.2 Spectrum of Pancreatic Disease
22.2.2.1 Annular Pancreas
The exact etiology is unknown. Annular pancreas can cause duodenal obstruction in the neonatal period in about 50 % of patients. It is associated with other congenital anomalies in up to 70 % of infants; these include duodenal stenosis or atresia, Down syndrome, tracheoesophageal fistula, and congenital heart disease (Nijs et al. 2005).
On US, fluid-distended descending duodenum can be seen encircled by pancreatic tissue. A circumferential narrowing of the duodenum can be identified in upper gastrointestinal series (Fig. 22.19). MRCP can demonstrate associated ductal anatomy.
22.2.2.2 Acute Pancreatitis
Acute pancreatitis is a significant cause of morbidity in children. There can be severe complications in 25 % of patients, with a 9 % recurrence and 10 % mortality rate. There are varied causes of acute pancreatitis, including idiopathic, trauma, structural anomalies, multisystem diseases, drugs and toxins, and viral infections (Darge and Anupindi 2009). Imaging features are nonspecific. US or CT may show diffuse or focal enlargement of pancreas or change in attenuation or echotexture. There may be surrounding fluid, pseudocyst formation, hemorrhage, or pancreatic duct dilatation (Fig. 22.20).
22.2.2.3 Pancreatoblastoma
Pancreatoblastoma is the most common pediatric exocrine tumor of the pancreas and occurs in young children with the mean age of 4 years. This tumor is associated with Beckwith-Wiedemann syndrome. It is usually an asymptomatic, large abdominal mass, and AFP is elevated in 25–55 % of the patients. Imaging studies typically reveal large heterogeneous masses with solid and cystic components, hyperechoic and enhancing septa, and hemorrhagic necrosis (Fig. 22.21) (Chung et al. 2006).
22.2.2.4 Solid and Papillary Epithelial Neoplasm
Solid and papillary epithelial neoplasm (SPEN) usually occurs in adolescent girls. The classic features of SPEN are a large well-encapsulated mass with varying solid and cystic components caused by hemorrhagic degeneration (Chung et al. 2006). Calcifications and enhancing solid areas may be present at the periphery of the mass (Fig. 22.22).
22.3 Splenic Disease
22.3.1 Anatomy and Development
The spleen arises from mesenchymal cells between the layers of the dorsal mesogastrium during the 5th week of gestation. The spleen’s function is hematopoiesis in the fetus, with a peak at approximately 20 weeks’ gestation. Accessory splenules are seen in 15 % of patients.
On US, the spleen is homogeneous, slightly more hyperechoic than the normal kidney, and isoechoic or more slightly hyperechoic than the liver. On MRI, splenic signal intensity varies with age. With contrast, splenic enhancement is initially heterogeneous due to a variable flow rate through red pulp (Fig. 22.23).
22.3.2 Spectrum of Splenic Disease
22.3.2.1 Splenomegaly
The size of the normal spleen depends on the age of the child. Its size is often measured in the longest coronal axis, averaging 6 cm at 3 months of age, 9 cm at 4 years of age, and 13 cm by 15 years of age. There are many causes of splenomegaly in children, including hemolytic anemia (Fig. 22.25), leukemia, lymphoma, portal hypertension, right heart failure, sepsis, and viral disease (Hilmes and Strouse 2007). Portal hypertension is a common cause of splenomegaly in children and is often due to extrahepatic portal vein obstruction from portal vein thrombosis (Fig. 22.24).
The role of imaging depends on the clinical presentation and the suspected diagnoses. Imaging clues to the presence of portal hypertension include heterogeneous liver, relative increase in size of the left lobe and caudate, lobular hepatic margins, and an abnormal Doppler evaluation of the portal vein including demonstration of thrombosis, reversed flow direction, or cavernous transformation (Hilmes and Strouse 2007).
22.3.2.2 Splenic Hamartoma
Hamartoma is rare, but it is the most common primary neoplasm of the spleen in children. It is a benign, well-circumscribed solid or predominantly solid tumor. On US, lesions are hypoechoic and relatively avascular, as opposed to hemangiomas. Lesions are isointense to the normal spleen on T1-weighted images and heterogeneously hypointense on T2-weighted images (Hilmes and Strouse 2007). They are usually enhanced less than normal parenchyma on CT and MRI (Fig. 22.26).
22.3.2.3 Splenic Injury
Abdominal trauma is a leading cause of death in children older than 1 year of age, and spleen is the most commonly injured intra-abdominal organ, accounting for up to 45 % of all visceral injuries (Lynn et al. 2009).
Diagnostic imaging is often critical to the early and accurate detection of splenic injury. Intravenous contrast-enhanced CT is the gold standard for evaluating blunt abdominal trauma (Fig. 22.27). Relative to CT, US is less sensitive in the diagnosis of splenic injuries. Recently, contrast-enhanced US using intravascular microbubble administration has been investigated (Oldenburg et al. 2004; Valentino et al. 2008). For homogeneous parenchymal enhancement of the spleen, the portal venous phase is optimal for detecting organ injury. Parenchymal ruptures can be associated with intraparenchymal and subcapsular hematomas, and splenic rupture is the most common injury and is easily identified by the presence of hemoperitoneum.
22.4 Illustrations: Liver, Biliary Tract, Pancreas, and Spleen
22.4.1 Neonatal Hepatitis
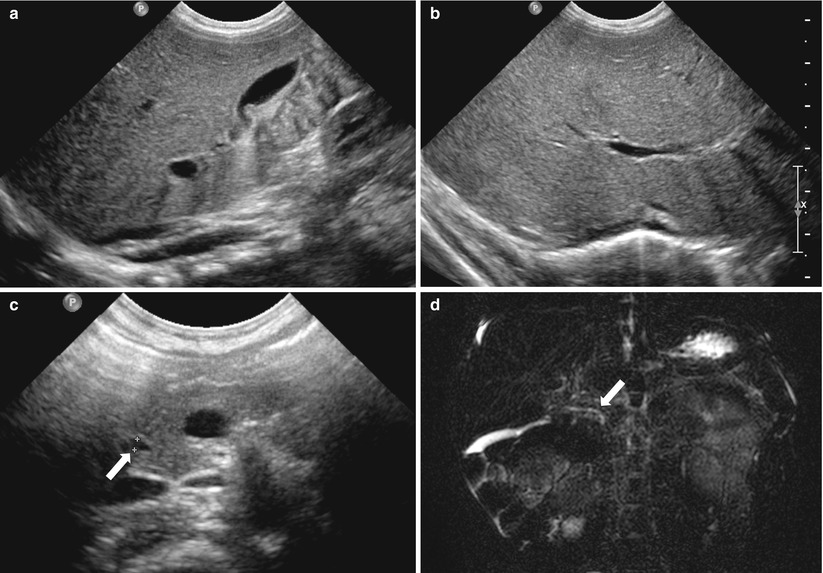
Fig. 22.1




Herpes simplex virus hepatitis in a male neonate. (a) Abdominal US shows grossly normal gallbladder. (b) Liver also shows homogenous parenchymal echogenicity without increased periportal echogenicity. (c) Common bile duct (arrow) is visualized on pancreas head portion. (d) Two-dimensional T2-weighted MR cholangiopancreatography (MRCP) well demonstrates normal extrahepatic biliary duct (arrow)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree