Liver: Portal Venous System and Hepatic Veins

Bile Ducts and Gallbladder
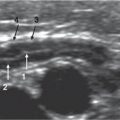
Ultrasound (US) is the imaging modality of choice for screening the gallbladder and biliary tract in children. The study should consist of a systematic examination of the liver, bile ducts, gallbladder, pancreas, and spleen. A complete duplex and color Doppler examination of the hepatic vessels should be performed. US guidance is very useful to guide invasive diagnostic or therapeutic procedures.
Magnetic resonance cholangiopancreatography (MRCP) is also a noninvasive, nonradiating technique; in young children, MRCP needs to be performed under sedation. MRCP uses the signal from the bile within the ducts to allow visualization of the biliary system. Fasting is necessary. The basic principle is to use a heavily T2-weighted sequence with fat suppression to show the high signal intensity of the static fluids. MRCP has the potential to replace diagnostic endoscopic retrograde pancreatography (ERCP) and percutaneous transhepatic cholangiography. A normal study obviates the need for more invasive studies.
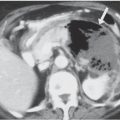
Computed tomography (CT) has very few indications because of the use of radiation and, frequently, intravenous contrast. CT is useful in differentiating aerobilia from calculus. Multidetector equipment allows fast scans and three-dimensional (3D) reconstruction of very good quality even in non–breath-holding children.
ERCP is invasive and technically diffcult. It requires general anesthesia in children and has the potential for significant associated morbidity. However, it is a useful diagnostic and therapeutic tool in selected cases.
Hepatobiliary scintigraphy is an isotopic study that uses technetium (99mTc)-labeled iminodiacetic acid that is extracted and secreted by the liver. Scintigraphic visualization of tracer in the gastrointestinal (GI) tract indicates patency of the extra hepatic biliary ducts. It is useful to demonstrate bile leakage after surgery and for diagnosing of biliary atresia.
Bile Ducts




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree