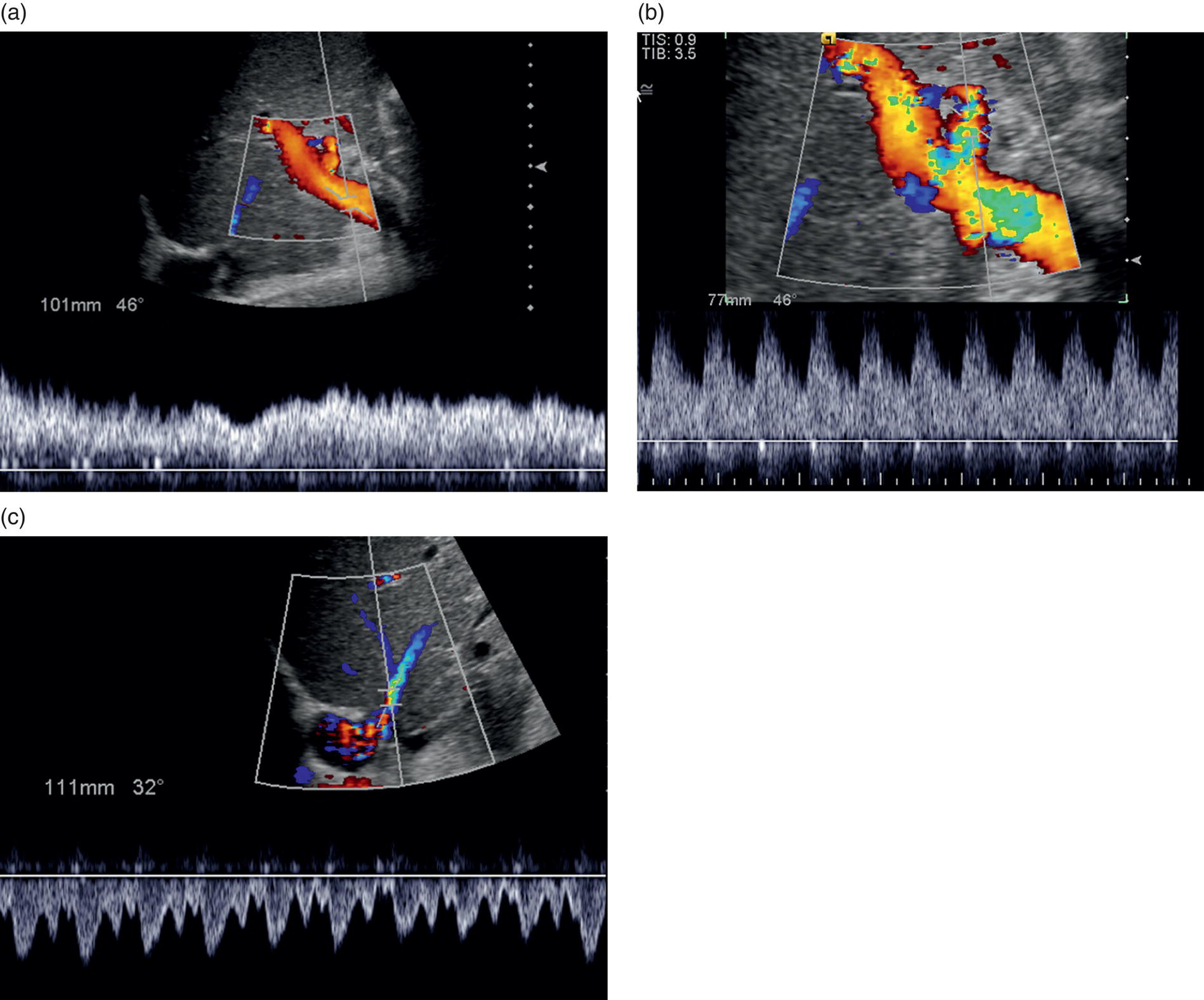
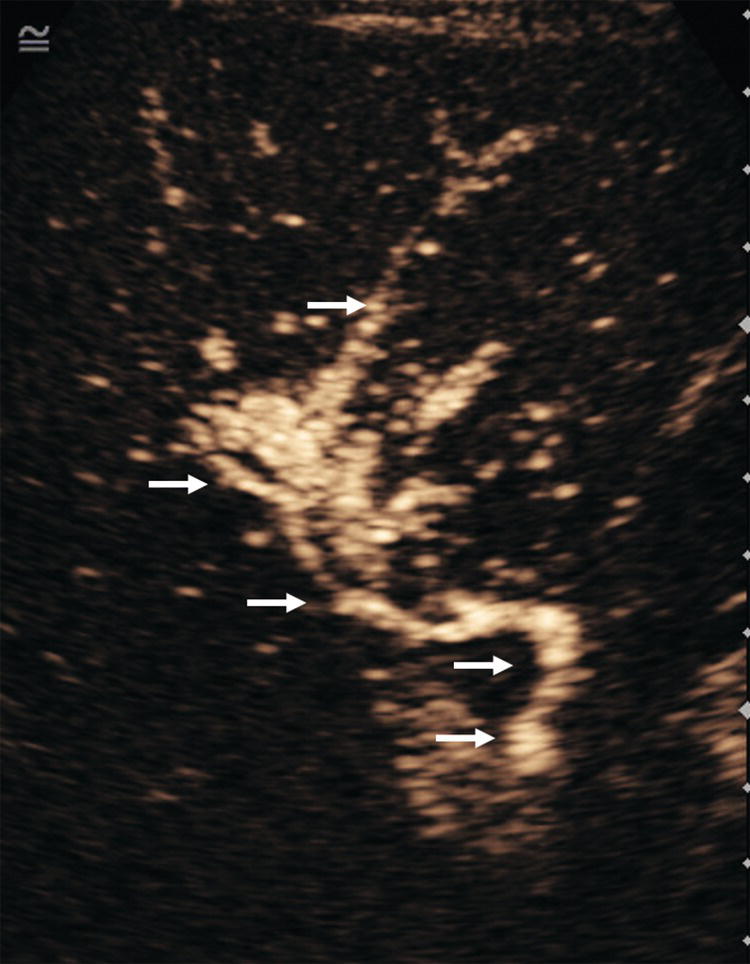
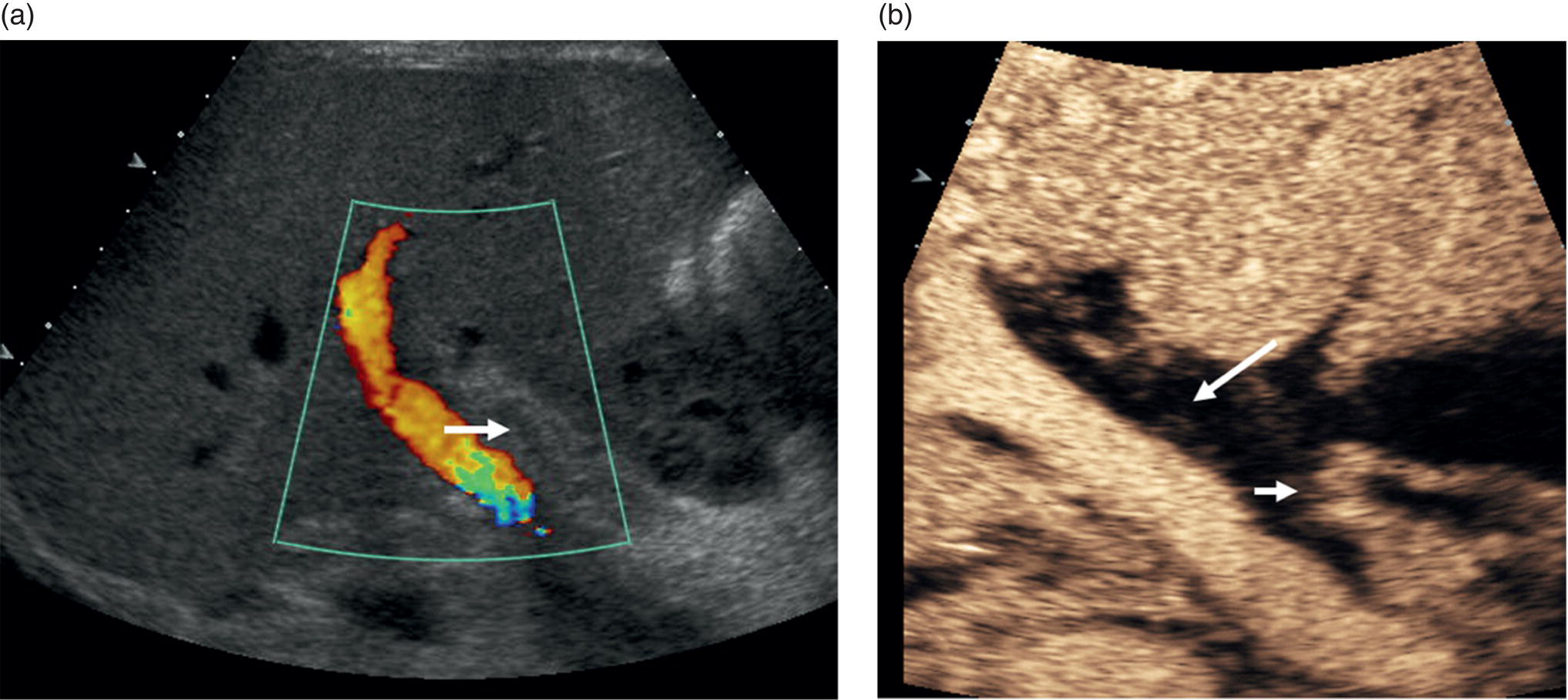
Thomas Puttick and Paul S. Sidhu Department of Radiology, King’s College Hospital, London, UK Orthotopic liver transplantation was introduced in 1963 and has been continually modified to improve patient outcome [1]. Liver transplantation is performed when there is end‐stage liver damage that has failed conservative medical and surgical treatments. The ultrasound assessment of the pre‐transplant patient is limited, with important areas of surveillance including underlying hepatocellular carcinoma (HCC) detection and the status of portal vein blood flow. The traditional orthotopic liver transplantation is the preferred technique, but with the shortage of cadaveric livers, both split‐liver transplantation and living donor liver transplantation are becoming more common [2]. Following transplantation, ultrasound plays a vital role. The introduction of bedside ultrasound, with colour and spectral Doppler techniques, was a milestone in the post‐operative care of these patients [3]. It is important that ultrasound practitioners understand common surgical techniques, particularly the anastomotic techniques, expected post‐operative imaging findings and that they are able to identify complications. Any post‐surgical complication, such as a fluid collection, abscess, small bowel ileus or a pleural effusion, will be a possibility following liver transplantation. The unique complications associated with a liver transplant are important too appreciate. The most common complications in the immediate post‐operative period are related to the vascular anastomoses and the hepatic artery is crucial; the patent artery is clearly depicted by Doppler ultrasound techniques. This chapter will present an overview of the position of ultrasound in the assessment of the liver transplant patient [4, 5]. Common indications for liver transplantation in the adult population include cirrhosis secondary to chronic hepatitis, acute hepatitis, metabolic disorders, sclerosing cholangitis, and Budd–Chiari syndrome. Widely accepted guidelines for patients with HCC requiring liver transplant are the Milan criteria, which state that no HCC lesion should be larger than 5 cm or up to three lesions equal to or less than 3 cm in diameter [6]. Contraindications for liver transplantation include sepsis, extrahepatic malignancy, severe cardiopulmonary disease, active alcohol or substance misuse, or abnormal anatomy that excludes liver transplantation. Portal vein thrombosis is a relative contraindication that makes surgery challenging with increased morbidity and mortality [7]. The pre‐operative ultrasound aspects in the liver transplant candidate are primarily associated with parenchymal change, presence of focal liver lesions, presence of portal hypertension, varices and the state of the portal vein [4]. Surgery for transplantation in the recipient involves hepatectomy, vascularisation of the new liver and biliary reconstruction. The surgical technique can be varied, but whole‐liver transplantation involves one biliary and four vascular anastomoses. The biliary anastomosis is an end‐to‐end anastomosis from the donor common bile duct (CBD) to the recipient common hepatic duct (CHD): a choledocholedochostomy. If the recipient CHD is diseased or absent, then a choledojejunostomy is formed. In orthotopic liver transplantation, the donor coeliac artery is anastomosed to the recipient hepatic artery via the bifurcation of the hepatic artery or the gastroduodenal artery. If there is a small or diseased hepatic artery or coeliac artery, then a donor iliac artery graft or aorto‐hepatic graft can be anastomosed to the recipient aorta. Portal vein connection is via an end‐to‐end anastomosis. The supra‐ and infrahepatic vena cava anastomoses are often end‐to‐end anastomoses [8]. Other surgical techniques include ‘piggy‐back’ transplant with an anastomosis between the donor vena cava at the junction with the hepatic veins directly onto the recipient vena cava, with a remnant blind donor inferior vena cava (IVC); right or left transplants; segmental transplant (in small children); and living donor transplants. Understanding ultrasound segmental liver anatomy using the Couinaud nomenclature is common practice and is essential in segmental transplants [9, 10]. The appearances of the normal vascular anatomy in the post‐transplant patient is readily identified on colour and spectral Doppler ultrasound (Figure 13.1) [11]. Figure 13.1 (a) The normal post‐liver transplantation colour and spectral ultrasound Doppler examination of the portal vein. (b) The normal post‐liver transplantation colour and spectral Doppler ultrasound examination of the hepatic artery. (c) The normal post‐liver transplantation colour and spectral Doppler ultrasound examination of a hepatic vein. Imaging is used to identify post‐transplantation complications, which are broadly divided into vascular, biliary and other complications associated with the surgical procedure. Identification of normal post‐operative appearances is vital to identify complications. Normal post‐operative ultrasound assessment would entail an examination on days 1, 3, and 5 following liver transplantation, primarily for the integrity of the vascular component of the transplant and to document any early post‐operative collections (haematoma, biloma, or less often infective). Any more frequent imaging with ultrasound or computed tomography (CT) is based on clinical requirements, and when ultrasound is inconclusive. A routine ultrasound examination involves assessment of the liver parenchyma and colour, spectral Doppler ultrasound interrogation of the vessels and assessment of the biliary tree and perihepatic spaces. There are common expected findings in the post‐operative liver transplantation that should resolve within a short time period, which include a small perihepatic haematoma, small right‐sided pleural effusion, small‐volume ascites and periportal oedema. Complications following liver transplantation identified with ultrasound include vasculature abnormality, biliary duct changes, liver parenchyma abnormalities and changes in perihepatic spaces. It is important not to take the imaging findings in isolation but to correlate the imaging findings with the liver graft function, biochemical and haematological findings, and most importantly the clinical assessment of the patient. Rejection is a common cause of hepatic dysfunction following transplantation, which is confirmed on liver biopsy, usually performed under ultrasound guidance. The role of ultrasound is to identify other causes of post‐transplantation hepatic dysfunction that can mimic rejection [12]. Vascular complications can involve occlusion (arterial or venous thrombosis), stricture (arterial or venous stenosis) and leaking (arterial pseudoaneurysm formation). Vascular thrombosis or stenosis can occur within the hepatic artery, portal vein or less commonly the intrahepatic veins and the IVC. Vascular complications may occur in the immediate post‐operative period, prompting initial identification with a bedside ultrasound, which is vital for graft preservation. Once the abnormality is suspected on ultrasound examination and if there is ongoing clinical concern or a suboptimal ultrasound, then contrast‐enhanced CT is often performed to confirm a vascular abnormality. The application of contrast‐enhanced ultrasound (CEUS) at this stage has also been reported successful [13]. The normal hepatic artery waveform demonstrates a rapid systolic upstroke (<80 m/s, time from end diastole to the first systolic peak) and continuous diastolic flow. The resistive index (RI, peak systolic velocity – peak diastolic velocity/peak systolic velocity) should be between 0.5 and 0.7. The post‐transplant hepatic artery should be readily identified on colour and spectral Doppler ultrasound, with the addition of CEUS to help delineate difficult vessels (Figure 13.2). In the immediate post‐transplant period, the hepatic artery may exhibit a high RI with little or no flow seen in diastole which is often due to reperfusion oedema. For this reason, scanning on day 0 post transplant is usually avoided and the initial ultrasound is scheduled for after >24 hours post surgery. Figure 13.2 A contrast‐enhanced ultrasound examination of a ‘difficult’ hepatic artery not seen clearly on the colour Doppler ultrasound examination. The hepatic artery is clearly patent (arrows), with a short window of opportunity to assess the artery after the ultrasound contrast agent injection, before enhancement of the portal vein and liver parenchyma. Hepatic artery thrombosis occurs in 3–10% of liver transplantations and accounts for 60% of all post‐transplantation complications [14]. Hepatic artery thrombus results in liver parenchyma ischaemia, then infarction, followed by biliary duct stricture and necrosis. If the hepatic artery thrombosis occurs early (within approximately 15 days of transplantation) and prior to the development of arterial collaterals, it can be life threatening (with a 20–60% mortality rate) and requires urgent surgical intervention. Risk factors for early hepatic artery thrombosis include acute rejection, prolonged cold ischaemic time of the donor liver, ABO blood incompatibility, paediatric transplantation and small donor or recipient vessels [15]. The colour Doppler and spectral ultrasound will identify over 90% of patent hepatic arteries, with a spectral Doppler ultrasound trace mandatory to demonstrate the arterial waveform [16]. If there is uncertainty as to the patency of the hepatic artery, a CEUS examination is useful prior to further imaging with CT (Figure 13.3) [17].
13
Liver Transplantation
Indications for Transplant
Surgical Techniques in Liver Transplantation
Post–Liver Transplant Imaging
Vascular Complications
Hepatic Artery
Hepatic Artery Thrombosis

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








