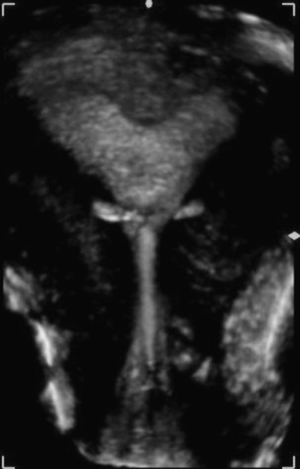
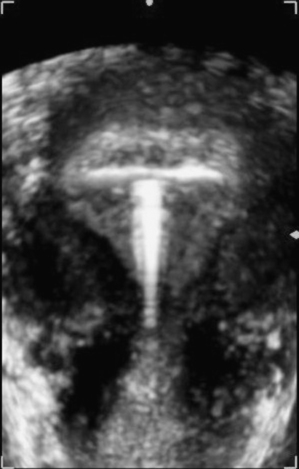
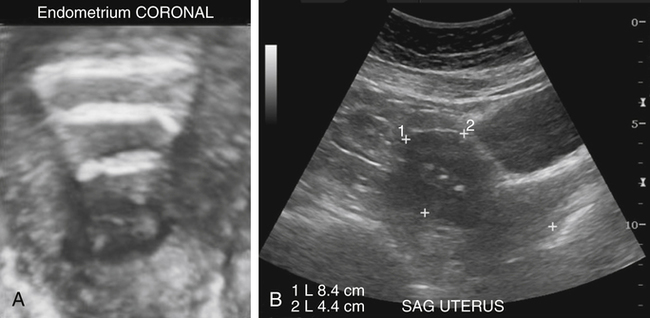
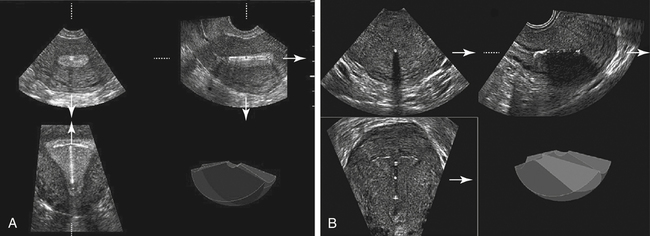
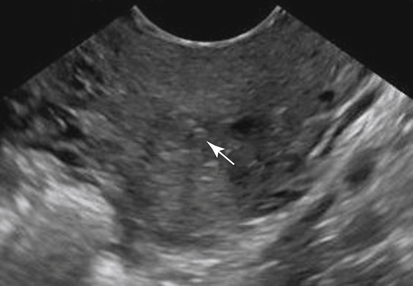
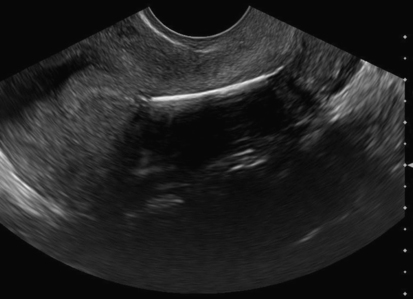
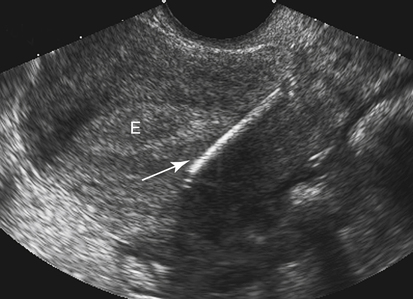
• Describe the sonographic appearance of properly positioned intrauterine devices (IUDs). • Describe the sonographic appearance of abnormally positioned IUDs. • Differentiate the sonographic characteristics of IUDs in association with complicating factors, including infection, perforation, and intrauterine and ectopic pregnancy. • Identify gynecologic symptoms associated with IUD use. An intrauterine device (IUD) is a flexible contraceptive device inserted through the vaginal canal into the endometrium. It is typically T-shaped, made of plastic, wrapped in copper, and may or may not contain hormones. Plastic strings tied to the end of the IUD generally suspend through the cervix into the superior portion of the vaginal canal. When the IUD has been properly inserted, the device expands from its temporarily constricted state (used for insertion through the endocervical canal) and lies in the midline of the endometrial cavity. The top bars of the “T” unfold after insertion to lie across the fundal portion of the endometrial cavity, and the stem lies vertically (Fig. 14-2). The IUD strings (usually two) are attached to the bottom of the stem and pass through the endocervical canal into the upper portion of the vagina, where they typically coil causing no symptoms. When the patient or clinician cannot locate the strings, a sonogram is ordered to localize the IUD. Missing strings might indicate the IUD has been expelled, the strings have fallen off, the strings have retracted into the uterus, malposition of the IUD, or perforation of the IUD into the myometrium or peritoneal cavity. Other indications for sonographic evaluation of an IUD include pelvic pain following insertion, abnormal bleeding, and a positive pregnancy test with a known IUD.1 The most common IUDs currently used in the United States include ParaGard and Mirena. These are small, safe, and highly effective contraceptive devices. ParaGard is a nonhormonal T-shaped plastic device wrapped in copper. Copper has a stimulating effect on the uterus, thickening the cervical mucus and producing a fluid that is toxic to sperm. This type of IUD is preferred but may cause menometrorrhagia and pelvic cramping. Copper-wrapped IUDs are approved for 10 years of continuous use before removal is necessary. Mirena is a T-shaped plastic device that releases low amounts of progestin. This type of IUD stimulates the endometrial glands to shrink and atrophy, reduces sperm survival, and inhibits embryo implantation. The hormones may prevent or decrease menstrual bleeding and cramping.2 This type of levonorgestrel-releasing device requires removal every 5 years. Discontinued IUDs include the serpentine-shaped Lippes Loop (Fig. 14-3), Copper 7 (shaped like a 7), Saf-T Coil (coil-shaped), and Dalkon Shield.3 Sonographic appearance varies depending on the type of IUD. All types of IUDs should be located in the midline portion of the endometrial cavity. The ParaGard IUD demonstrates two parallel hyperechoic linear echoes with intense posterior acoustic shadowing. The two echogenic parallel structures (entrance-exit reflections) represent the anterior and posterior surfaces of the IUD. The intense attenuation of the sound beam is caused by the copper wire (Fig. 14-4, A). The Mirena IUD demonstrates a hypoechoic or mildly echogenic stem with thin echogenic “T-arms” (Fig. 14-4, B). 3D imaging in the coronal plane displays the IUD in its entirety, which is advantageous when evaluating location. The strings are the consistency of fine fishing line and are occasionally visualized sonographically (Fig. 14-5). Expulsion of the IUD generally occurs within the first year, most commonly during the first few months after insertion. Expulsion is more likely to occur when inserted soon after childbirth or in women with a history of previous expulsion, nulliparity, or severe menorrhagia.4 Clinically, women can be asymptomatic or complain of cramping, vaginal discharge, intermenstrual or postcoital bleeding or spotting, and dyspareunia.5 An IUD is abnormally located if it is inferiorly located within the endometrial cavity or if any part extends past the confines of the cavity into the uterus or cervix. An inferior location of the IUD may be a result of migration or improper insertion of the device, and patients may experience pain or be asymptomatic. An IUD in this location decreases the contraceptive effectiveness and is at risk for being expelled.6 If the IUD is embedded in the myometrium, operative hysteroscopy may be required for removal. Extension or penetration of the IUD through the basal layer of the endometrium into the uterine myometrium may occur. Generally, the “T” portion of the IUD extends partially or completely through the lateral and fundal portions of the endometrial layers embedding into the myometrium of the uterus.7 Women may be asymptomatic or experience pelvic pain or irregular bleeding. According to one study, patients presenting for 3D sonography with pain or irregular bleeding are at higher risk of having an abnormally located IUD compared with patients with a normally positioned IUD.1 Myometrial penetration of an IUD results in an eccentric position of the IUD within the endometrial cavity or myometrium (Fig. 14-7). The linear hyperechoic “arms” of the IUD breach the basal layer of endometrium and extend into the myometrium. 3D imaging in the coronal plane has greatly improved sonographic detail of IUDs by enhancing visualization of the shape and location of the device within the endometrial cavity.3 Perforation is rare occurring in approximately 1 per 1000 insertions.8 Perforation almost always occurs during insertion and is associated with an inexperienced clinician, retroverted uterus, and congenital uterine anomalies. Pelvic pain is the principal clinical finding. Complications include damage and scarring of the surrounding organs and pelvic infection.9 If an IUD has perforated to the extent that it is no longer within the endometrial cavity, the endometrial cavity is clearly delineated separately from the location of the IUD. The IUD may be visible in the myometrium, the cervix, or the pelvic or abdominal cavity. It is possible that no IUD is seen at all, suggesting expulsion or perforation into the peritoneum. A radiograph should be obtained whenever the IUD cannot be visualized sonographically because IUDs are radiopaque and show up on radiographic images (Fig. 14-8).
Localize Intrauterine Device
Normal Sonographic Appearance of an Intrauterine Device
Intrauterine Device Complications
Expulsion of Intrauterine Device
Migration
Myometrial Penetration
Sonographic Findings
Perforation
Sonographic Findings

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Localize Intrauterine Device