Fig. 10.1
(a–c) Distinguishing true AS from pseudo AS. In patients with LF-LG AS, as the continuity equation is less accurate and is known to underestimate the valve area, distinguishing the patient with severe AS causing LV dysfunction secondary to afterload mismatch (true AS) from the one who has LV dysfunction and coexisting mild to moderate AS (pseudo AS) is clinically essential. DSE can help to discriminate the two distinct pathologies; at peak stress valve area can slightly increase while gradients are dramatically increased in true AS, whereas in pseudo AS, valve area increases > 0.3 cm2 and gradients slightly increase due to moderate AS
Box 10.1 Distinguising True from Psuedo AS During Dobutamine Infusion
True | AVA does not change but transvalvular gradients increase |
Pseudo | Increased flow results in increased AVA (i.e., increase >0.3 cm2) |
Surgical Aortic Valve Replacement: Predictors of Outcome
In 1980, Carabello et al. demonstrated that outcomes of patients with LG and low EF AS were poor and risk of surgery was high [8]. Subsequently, in a study of 52 patients with impaired LVEF (≤35 %) and LG (<30 mmHg) AS, Connoly et al. confirmed high operative risk. Perioperative mortality was 21 %, and overall survival at 3 and 5 years was 62 and 39 %, respectively [9]. Significant improvement in symptomatic status following AVR was reported in particular younger patient age group and larger prosthesis size. However, it is still incompletely understood whether AVR in these patients improves long-term survival compared to medical therapy. Pereira et al. compared LG (<30 mmHg) severe AS patients with LV dysfunction (LVEF ≤35 %) who did and did not receive surgical valve replacement and demonstrated that there is not only symptomatic benefit but also a mortality benefit following AVR in the LG AS group. In patients who underwent AVR, 4-year survival rate was found markedly improved (79 %), as compared to medically treated patients. Together with age and serum creatinine level, AVR was found to be a main predictor of improved survival [10]. In order to better understand which patients would have more benefits from AVR, further studies tested clinical utility and prognostic importance of LV contractile reserve with dobutamine stress echocardiography (DSE).
Impact of LV Contractile Reserve (CR)
In patients with true AS, determination of LV CR with a DSE test is an essential step in clinical decision making and furthermore provides important prognostic data regarding perioperative mortality and postoperative survival. LV contractile reserve is defined as an increase in stroke volume >20 % during DSE [11] (Fig. 10.2).
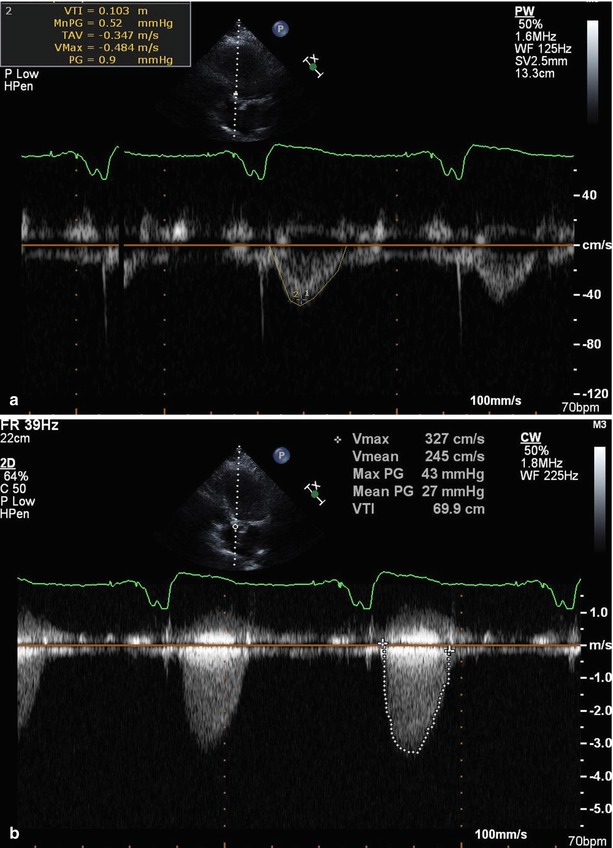
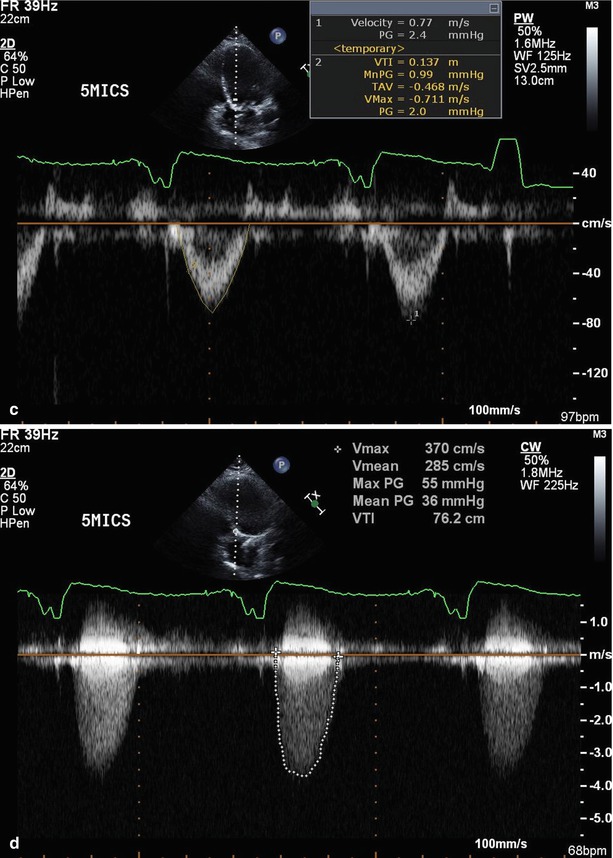
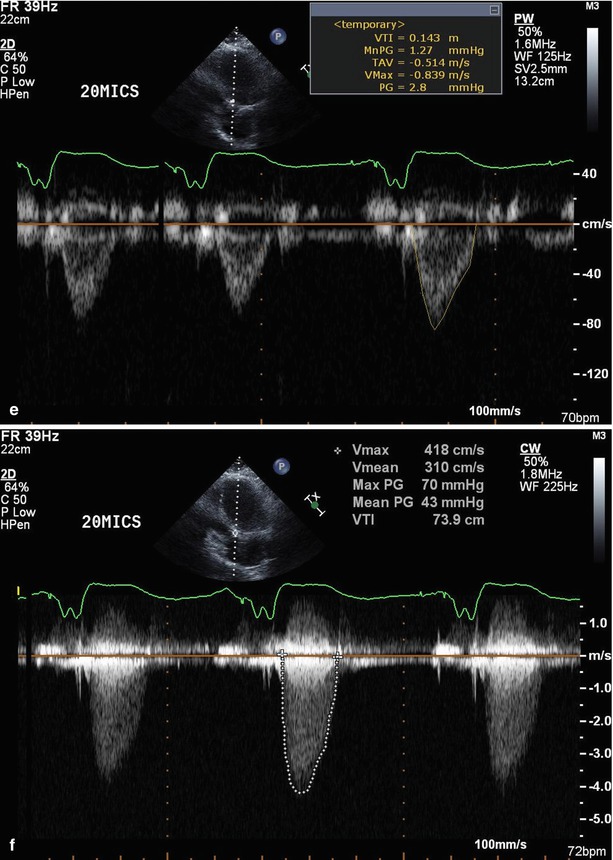
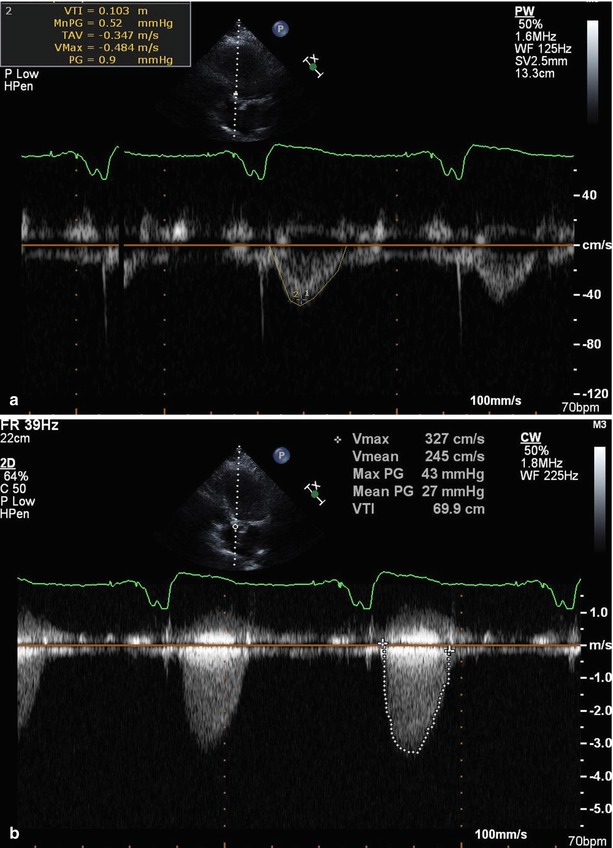
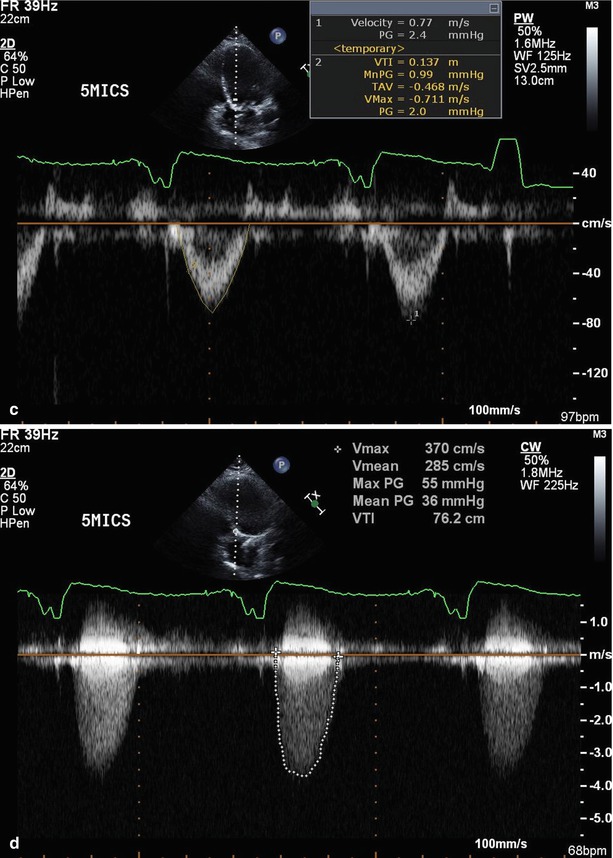
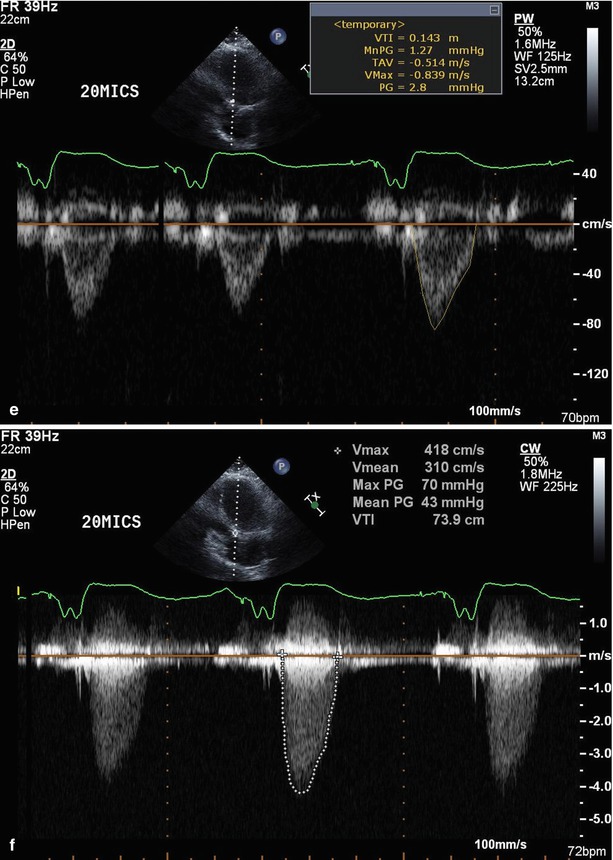
Fig. 10.2
Assessment of low-gradient AS by dobutamine stress echocardiography and LV contractile reserve. A 71-year-old man presented with shortness of breath (NYHA class III). Baseline LVEF was 20 %, calculated AVA was 0.45 cm2, and max/mean gradients were 43/27 mmHg. DSE was performed (1) to distinguish true AS from pseudo AS and (2) to assess whether he had LV CR. (a) Baseline stroke volume was calculated 32 cc; (b) after low-dose dobutamine stroke volume and gradients were increased to 43 cc and 55/36 mmHg, respectively. (c) At peak DSE, stroke volume was calculated 46 cc and gradients were increased to 70/43 mmHg. LVCR was calculated as 43 %. DSE results in this patient with LF-LG AS are consistent with true AS with LV CR. This case was considered high risk for conventional SAVR due to his comorbidities, and 26 mm Edwards Sapien valve was inserted via transfemoral route
Assessment of LV CR is important, because presence of LV CR indicates better survival in patients with LF-LG severe AS and reduced LVEF. In a study of 136 patients with LG (<40 mmHg) symptomatic severe AS, who underwent DSE, perioperative mortality was found 5 % in patients with LV CR versus 33 % in those without CR [12]. However, lack of LV CR should not be considered an absolute contraindication for valve replacement. In a subsequent report of 66 patients from the above study, symptomatic recovery and improvement of functional capacity after AVR were similar in those with and without LV CR [13]. Based on these data, risk stratification in patients with LF-LG AS is difficult, because symptomatic recovery and improvement of LVEF after surgery are not associated with higher operative mortality rate and decreased survival (Fig. 10.3a–f) [14].
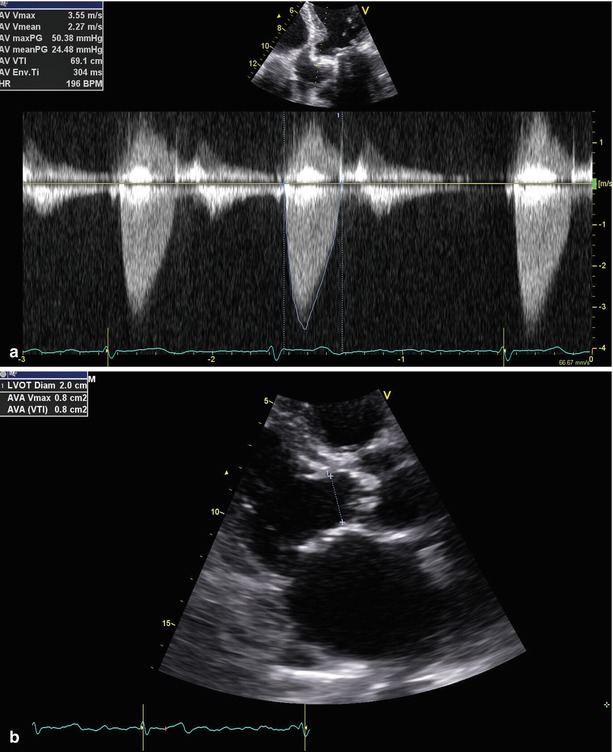
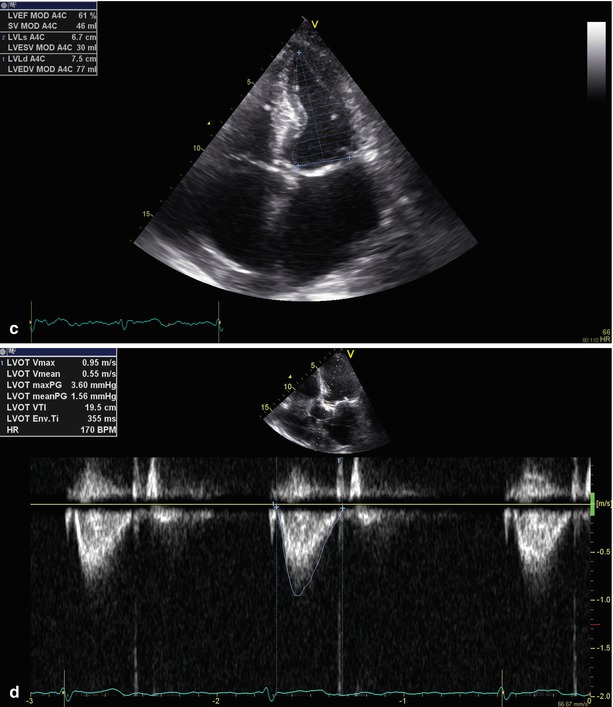
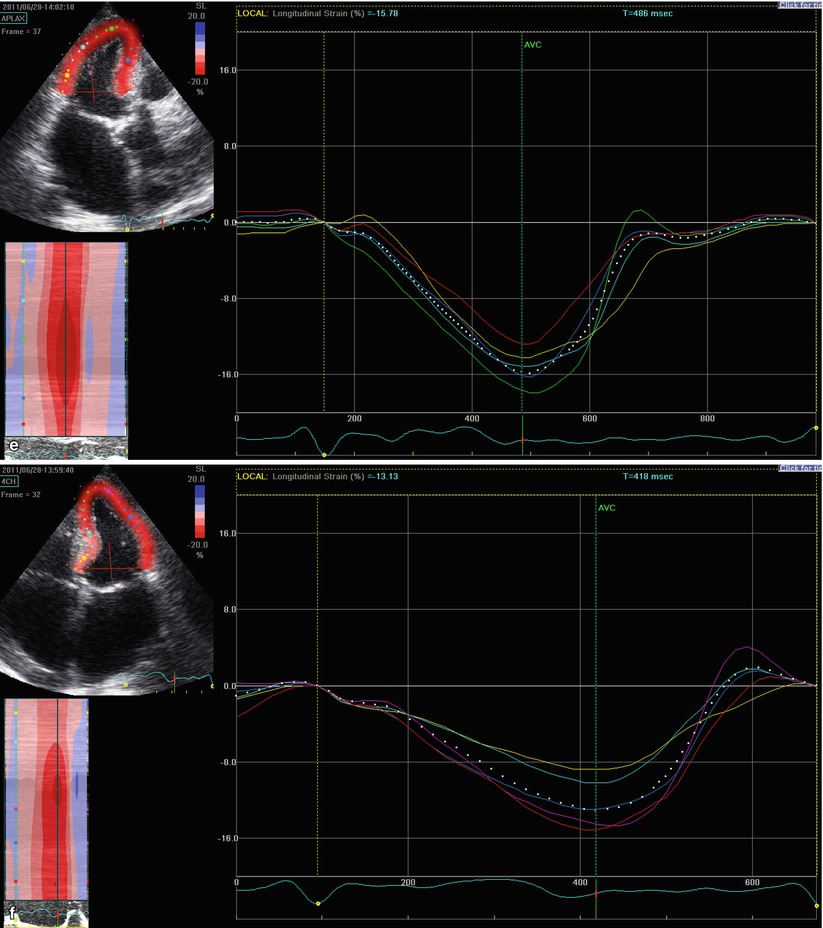
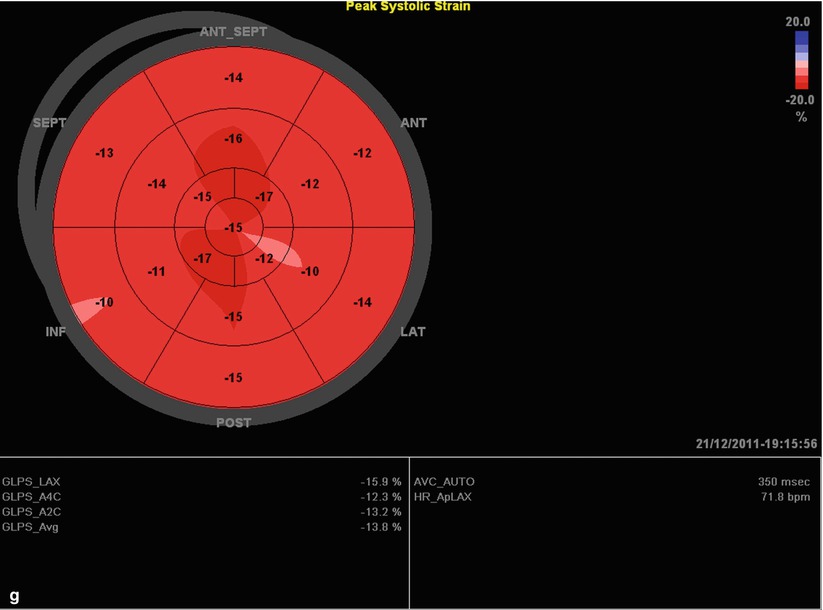
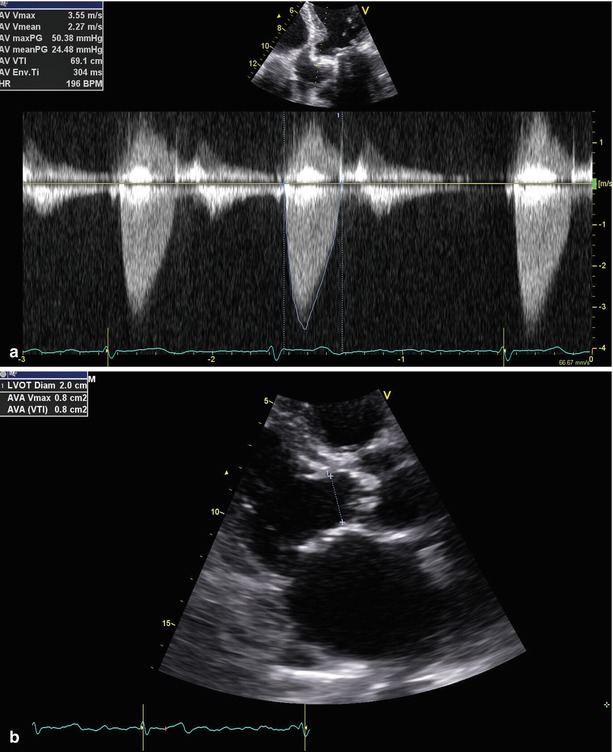
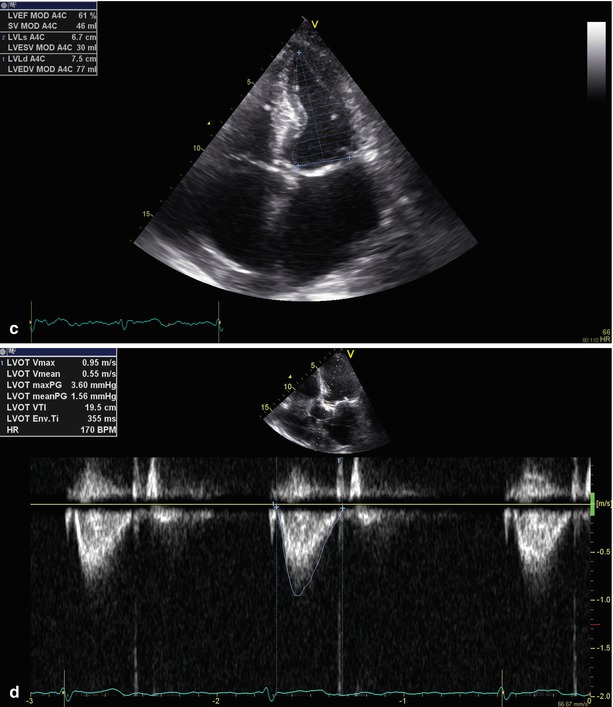
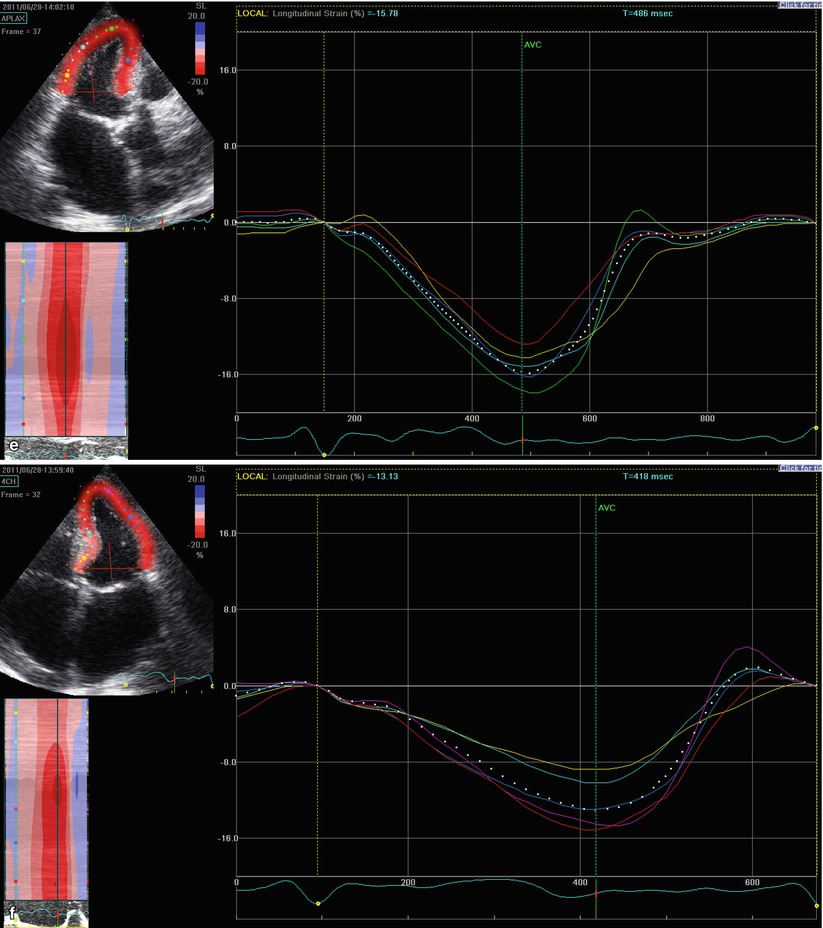
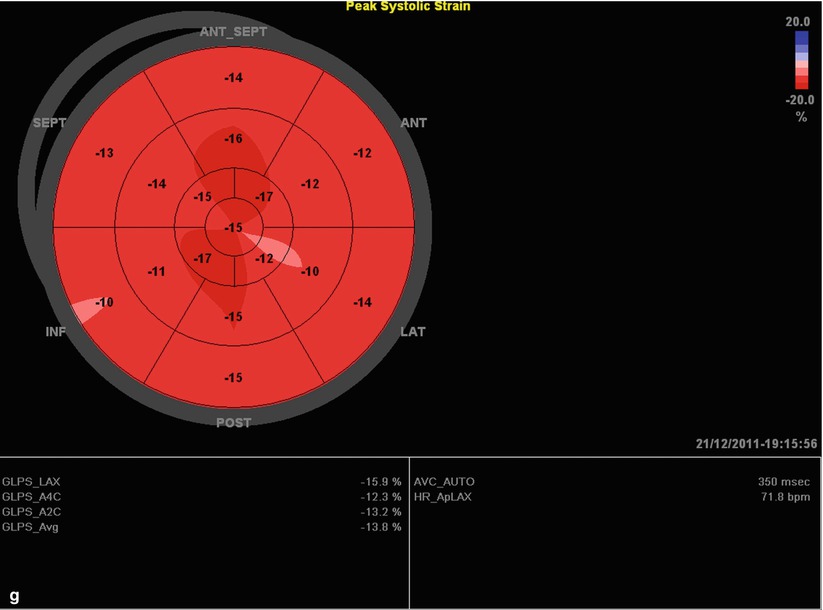
Fig. 10.3
(a–d) Paradoxically low-flow and low-gradient severe AS. A 78-year-old man who was diagnosed with severe AS presented with dyspnea on exertion. Calculated AVA was 0.88 cm2 (iAVA was 0.44 cm2/m2 with a BSA of 2 m2) but gradients were measured as 50/24 mmHg despite LVEF of 61 %. SVi was calculated 30.6 mL/m2. The patient was considered as low-flow and low-gradient severe AS despite preserved LV EF. (e–g) Assessment of segmental and global strain by 2D STE. Global longitudinal strain was found to be 13.3 % indicating mildly decreased LV function. Decreased global strain indicates possible subtle impaired LV dysfunction. Since the patient was not a good candidate for surgical AVR due to multiple comorbidities, transcatheter aortic valve replacement (TAVi) was performed via transfemoral approach (From Ozkan [37]; with permission from AME publishing)
Impact of Plasma BNP Levels
Increased plasma BNP levels have been correlated with onset of symptoms and prognosis in asymptomatic AS patients [15, 16]. In one study, 69 patients with LG (<40 mmHg) and low LVEF (40 %) were investigated with DSE to distinguish true from pseudo AS. Simultaneously, plasma BNP was analyzed in order to understand its diagnostic and prognostic value in LF-LG AS. Patients with true AS had significantly higher BNP levels than patients with pseudo AS. However, large overlaps of BNP levels were observed between patient with pseudo and true AS. Furthermore, high plasma BNP was associated with poor outcome in the entire study cohort with a cutoff value of 550 pg/mL independent of LV CR [17]. These data suggest that increased BNP levels cannot reliably distinguish true from pseudo AS.
Low-Gradient AS in the Era of TAVR
TAVR is a promising alternative therapeutic approach for patients, who are at high risk for conventional SAVR. The Placement of Aortic Transcatheter Valves (PARTNER) trial demonstrated that in high-risk patients, TAVR is associated with significantly better outcome in comparison to standard medical therapy in non-operable patients [18] and equivalent outcomes compared to SAVR [19]. However, reflecting the fact that a gradient >40 is a specific inclusion criteria, a dedicated subgroup analysis of outcome in patient with LF-LG AS is not available. There is currently no randomized data investigating outcomes of LF-LG AS patients after TAVR. In non-randomized studies, Clavel et al. compared outcome of patients with low LVEF who received SAVR versus TAVR using propensity-matched analysis. The authors found that TAVR is associated with better LVEF recovery compared to SAVR. Recovery of LVEF was not significantly different in patients with low versus high gradients. In this study, among the 283 patients, only 71 patients underwent DSE. In this subset, the presence of LV CR was not found to be a predictor of LVEF recovery [20].
In another recent study, 38 patient with low gradients (<40 mmHg) and low LVEF (<40 %), who underwent TAVR, were compared to a group of surgically treated patient (n = 33). Both groups had significant improvement in LVEF with presence of high preoperative gradient being a predictor for an improvement of LVEF [21]. Gotzmann et al. studied 167 consecutive patients who underwent TAVR, of whom 15 (8 %) had LF-LG (<40 mmHg) and decreased LVEF (<40 %) [22]. While all patients showed symptomatic benefit, significant improvement of LVEF, and exercise capacity, all cause mortality at 6 months following TAVR was found considerably higher in the LF-LG group.
A recent study analyzed 126 patients after TAVR—35 patients with low-gradient AS and 91 patients with high-gradient (≥40 mmHg) AS—and confirmed that low-gradient patients are at increased risk. Although procedural success was reported as 98 %, major adverse cardiovascular events (MACE) and cardiovascular death were reported 29 and 10 %, respectively. In multivariate analysis, presence of low preoperative transvalvular gradient was found to be associated with two- to fourfold increase in hazards for MACE and cardiovascular death [23].
Mitral regurgitation has been found more common in patients undergoing TAVR. Mitral regurgitation can be responsible for both the LF-LG itself and increased surgical operative mortality in this cohort [24]. Significant regression of MR has been shown in AS patients following TAVR, a finding which may contribute to maintained forward stroke volume and associated symptomatic improvement and better outcome [25].
Low-Gradient Aortic Stenosis Despite Preserved LVEF
As described above, low-gradient severe AS is most commonly seen in patients with LV systolic dysfunction, where low cardiac output is secondary to systolic dysfunction. However, recent studies demonstrated that severe LG AS can be encountered in patients with normal LVEF. This clinical entity of “paradoxical low flow and low gradient” is consistent with more advanced stages of disease with poor prognosis [4]. However, other studies demonstrate that assessing the true frequency of this entity is confounded by inconsistent grading of aortic valve stenosis, with both echocardiography and invasive measurements [26]. The discrepancy between aortic valve area (AVA) and mean gradient (MG) can potentially cause an underestimation of stenosis and thus lead inappropriate delay of AVR [27]. In fact, previous studies show that compared to high-gradient patients, patients with LG severe AS were less frequently referred to AVR. Since AVR has been found to be associated with significant improvement in long-term survival despite low-gradient, clarification of disease severity is critical in the subgroup of LF-LG AS [28, 29].
Prevalence and Significance of Paradoxically Low-Flow and Low-Gradient AS
In a study of 512 patients with severe aortic stenosis, indexed AVA ≤0.6 cm2/m2, and preserved LVEF >50 %, 181 (35 %) patients had paradoxically low flow (stroke volume index ≤35 mL/m2) [4]. When compared with normal flow patients, low-flow patients were more frequently female, had a higher prevalence of lower transvalvular gradient (32 ± 17 versus 40 ± 15 mmHg; p < 0.001), a lower LV diastolic volume index (52 ± 12 versus 59 ± 13 mL/m2; p < 0.001), lower LVEF (62 ± 8 % versus 68 ± 7 %; p < 0.001), and a higher level of LV global afterload reflected by a higher valvuloarterial impedance (5.3 ± 1.3 versus 4.1 ± 0.7 mmHg · mL−1 · m−2; p < 0.001). Importantly, compared with normal flow patients, low-flow patients had a lower overall 3-year survival (76 % versus 86 %; p < 0.006). These data suggest that this pattern of the disease represents more advanced stage of the disease, which are in turn associated with poorer outcomes.
Other studies suggest that the current focus on transvalvular gradients, when grading AS clinically, is associated with underestimation of AS severity and misdiagnosis of LG severe AS. This delay to diagnosis is also associated with a significant, and inappropriate, delay to AVR. An almost 50 % lower referral rate for AVR and twofold increase in mortality exists for patients with low-gradient AS as compared to high-gradient patients [28].
Pathophysiology
Current data suggest that LG severe AS (i.e., paradoxically low-flow and low-gradient AS) can be explained by decreased cardiac output. Postulated mechanisms include severe concentric LV hypertrophy with small LV cavity, restrictive filling pattern, and increased global afterload with decreased arterial compliance. Subtle LV myocardial dysfunction has been demonstrated by 2D Speckle Tracking Echocardiography (2D-STE) [30, 31], with increased myocardial fibrosis and decreased longitudinal mechanics also shown in previous MRI studies [32]. Increased fibrosis and subendocardial ischemia result in subtle LV systolic dysfunction with apparently normal LVEF.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








