Imaging evaluation of cranial neuropathies requires thorough knowledge of the anatomic, physiologic, and pathologic features of the cranial nerves, as well as detailed clinical information, which is necessary for tailoring the examinations, locating the abnormalities, and interpreting the imaging findings. This article provides clinical, anatomic, and radiological information on lower (7th to 12th) cranial nerves, along with high-resolution magnetic resonance images as a guide for optimal imaging technique, so as to improve the diagnosis of cranial neuropathy.
Key points
- •
Enhancement of the intracanalicular and/or the labyrinthine portion of the facial nerve is always abnormal.
- •
Vestibulocochlear nerve schwannomas typically develop as intracanalicular–cisternal masses, whereas meningiomas develop as cisternal masses.
- •
Simultaneous glossopharyngeal, vagal, and spinal accessory neuropathy indicates a jugular foramen lesion. In the latter setting, paraganglioma constitutes the most common etiology.
- •
In isolated vagal neuropathy, detailed knowledge of the clinical findings is mandatory to tailor the examination and interpret the imaging findings.
- •
In hypoglossal neuropathy, the most important magnetic resonance imaging (MRI) feature is unilateral signal intensity denervation changes of the tongue musculature.
- •
Neurosarcoidosis, subarachnoid hemorrhage, basal meningitis, and viral neuritis may involve multiple lower cranial nerves and be demonstrated on MRI as nerve thickening and contrast enhancement.
Introduction
Imaging evaluation of cranial neuropathies (CNs) is a challenging task for radiologists, requiring thorough knowledge of the anatomic, physiologic, and pathologic features of the cranial nerves, as well as detailed clinical information, which is necessary for tailoring the examinations, locating the abnormalities, and interpreting the imaging findings. Although computed tomography (CT) provides excellent depiction of the skull base foramina, the nerves themselves can only be visualized in detail on magnetic resonance imaging (MRI). This review provides clinical, anatomic, and radiological information on lower CNs (VII to XII), along with high-resolution magnetic resonance images as a guide for optimal imaging technique, so as to improve the diagnosis of cranial neuropathy.
Introduction
Imaging evaluation of cranial neuropathies (CNs) is a challenging task for radiologists, requiring thorough knowledge of the anatomic, physiologic, and pathologic features of the cranial nerves, as well as detailed clinical information, which is necessary for tailoring the examinations, locating the abnormalities, and interpreting the imaging findings. Although computed tomography (CT) provides excellent depiction of the skull base foramina, the nerves themselves can only be visualized in detail on magnetic resonance imaging (MRI). This review provides clinical, anatomic, and radiological information on lower CNs (VII to XII), along with high-resolution magnetic resonance images as a guide for optimal imaging technique, so as to improve the diagnosis of cranial neuropathy.
Anatomy
CN VII: Facial Nerve
The facial nerve is a complex mixed nerve, consisting of the facial nerve proper (the larger motor component) and the nervus intermedius (the smaller sensory component). The preganglionic fibers originate from the main motor nucleus, which is situated in the midpons. These join fibers from the superior salivatory nucleus, the nucleus solitarius, and the spinal tract of CN V. The facial nerve emerges at the ventrolateral aspect of the caudal pons, crosses the cerebellopontine angle (CPA) cistern, together with the vestibulocochlear nerve, and enters the temporal bone. The intratemporal course and central connections of the facial nerve can be roughly divided into the following segments:
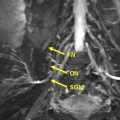
The meatal segment runs within the internal acoustic canal (IAC), occupying the anterosuperior portion of the latter ( Fig. 1 ).
Superior to the cochlea, the labyrinthine segment connects with the geniculate ganglion and provides the greater superficial petrosal nerve, which participates in the innervation of the lacrimal gland and mucous membranes of the nasal cavity and palate.
The tympanic (horizontal) segment extends from the geniculate ganglion to the horizontal semicircular canal.
At the latter location, a second genu is formed, marking the beginning of the mastoid portion, which runs inferiorly within the mastoid bone and provides a) the nerve to the stapedius muscle b) the chorda tympani nerve, which provides secretomotor innervation to the submaxillary and sublingual glands, as well as sensory innervation to the anterior two thirds of the tongue c) the auricular branch of the vagus nerve, which participates in the sensory innervation of the posterior auditory canal.
The motor component of CN VII exits the skull through the stylomastoid foramen, and provides the posterior auricular nerve, which innervates the postauricular muscles, and two small branches, which innervate the posterior belly of the digastric muscle and the stylohyoid. Subsequently, the facial nerve penetrates the parotid gland, passes lateral to the retromandibular vein, and courses superficially into the muscles of facial expression.
CN VIII: Vestibulocochlear Nerve
The vestibulocochlear nerve is a sensory nerve, consisting of a superior vestibular, an inferior vestibular, and a cochlear component. The fibers originate from vestibular nuclei located in the pons and medulla, and cochlear nuclei situated in the inferior cerebellar peduncles. The nerve emerges in the groove between the pons and the medulla oblongata, just posterior to the facial nerve, and courses together and parallel to the latter within the CPA cistern and the internal acoustic canal. The cochlear component runs in the anteroinferior aspect of the canal, whereas the superior and inferior vestibular components run in the posterosuperior and posteroinferior aspects, respectively (see Fig. 1 ). The peripheral branches of the vestibular components are distributed in the utricle, saccule and semicircular ducts, whereas the respective branches of the cochlear component end at the organ of Corti.
CN IX: Glossopharyngeal Nerve
Among the six lower CNs, the glossopharyngeal is the smallest in terms of diameter, importance, and clinical significance. The ninth nerve is a mixed nerve, which contains motor, somatosensory, visceral sensory, and parasympathetic fibers. The preganglionic fibers originate from the nucleus ambiguous, inferior salivatory nucleus, nucleus of tractus solitarius, and spinal trigeminal nucleus. The nerve exits the brain stem from the lateral aspect of the upper medulla along with cranial nerves X and XI, crosses the pontine cistern, and enters the pars nervosa of the jugular foramen ( Fig. 2 ). In passing through the latter, the nerve enters the superior and the petrous ganglia, from which final peripheral branches emanate. These include:
The tympanic nerve (which forms the tympanic plexus that gives off the lesser superficial petrosal nerve, a branch to join the superficial petrosal nerve and branches to the tympanic cavity)
Carotid branches (which connect with the vagus nerve and sympathetic branches)
Pharyngeal branches (which supply the muscles and mucous membrane of the pharynx)
Tonsilar branches (which supply the palatine tonsils)
Lingual branches (which supply the posterior third of the tongue and communicate with the lingual nerve)
A muscular branch (which is distributed to the stylopharyngeus)
CN X: Vagus Nerve
The vagus nerve contains motor, sensory, and parasympathetic nerve fibers, and features the most extensive course and distribution among all CNs, coursing through the neck and traversing in the thorax and abdomen. The preganglionic fibers emanate from the nucleus ambiguous, dorsal motor nucleus, nucleus of tractus solitarius, and spinal trigeminal nucleus. The nerve emerges from the medulla oblongata, between the olive and the inferior cerebellar peduncle, just posterior to the glossopharyngeal nerve (see Fig. 2 ), entering the pars vascularis of the jugular foramen, where it forms the jugular and the nodose ganglia. Between the 2 latter ganglia, the vagus nerve gives off an auricular ramus, which innervates the skin of the concha of the external ear; a meningeal ramus, which runs to the dura matter of the posterior fossa; as well as a pharyngeal ramus, which forms the pharyngeal plexus with the glossopharyngeal nerve that supplies the muscles of the pharynx and soft palate (except the stylopharyngeus and tensor veli palatine muscles). Just distal to the nodose ganglion, the vagus nerve gives off the superior laryngeal nerve, which provides motor innervation to the cricothyroid muscle and sensory innervation to the larynx. Subsequently, CN X descends in the neck within the carotid sheath, between the common carotid artery and the internal jugular vein. At the base of the neck, it provides the superior cardiac branches and the recurrent laryngeal nerves. The right recurrent laryngeal nerve bends upward and medially behind the subclavian artery, and ascends in the ipsilateral tracheoesophageal sulcus, whereas the left branch arises to the left of the aortic arch, loops beneath the ligamentum arteriosum, and ascends in the left tracheoesophageal sulcus. The recurrent laryngeal nerve innervates all the laryngeal muscles, except the cricothyroid, which is innervated by the superior laryngeal nerve. Subsequently, the vagus nerve enters the thorax, coursing over the subclavian artery on the right side, and between the common carotid and subclavian artery on the left side, and gives off branches to the pulmonary and esophageal plexuses. After crossing through the esophageal hiatus, the nerve terminates in multiple abdominal viscera.
CN XI: (SPINAL) Accessory Nerve
The accessory nerve (often termed the spinal accessory nerve) is a motor nerve, composed of a small cranial part, which originates from the nucleus ambiguous and emerges from the side of the medulla oblongata, and a large spinal portion, which originates from the ventral horn of the spinal cord, between the C1 and C5 levels ( Fig. 3 ). The 2 parts unite and enter the pars vascularis of the jugular foramen. The cranial part reaches the inferior vagal ganglion portion and is distributed to the striated muscles of the soft palate and larynx, whereas the spinal portion crosses the transverse process of C1 and provides innervation to the sternocleidomastoid and trapezius.
CN XII: Hypoglossal Nerve
The nucleus of the hypoglossal nerve is situated along the paramedian area of the anterior wall of the fourth ventricle in the medulla. The nerve emerges from the preolivary sulcus, runs through the hypoglossal canal, passes behind the inferior ganglion of the vagus nerve, and between the internal carotid artery and internal jugular vein ( Fig. 4 ). After reaching the submandibular region, the hypoglossal nerve is distributed to the intrinsic muscles of the tongue (except the palatoglossus), as well as the genioglossus, styloglossus, hyoglossus, and anterior strap muscles.
Imaging protocol
High-field imaging (3 T or newer 1.5 T scanners) is preferred to make use of the highest available signal-to-noise ratio and contrast-to-noise ratio, while keeping the imaging time in an acceptable range. A protocol that is commonly employed in most institutions and provides adequate high-resolution diagnostic evaluation is presented in Table 1 . Thin-section imaging (1 mm) and low voxel size (0.6–1 mm for isotropic constructive interference in steady state [CISS] imaging) are essential to obtain the high-resolution evaluation of the posterior fossa CNs.
| Plane | Sequence | Technique | Comment |
|---|---|---|---|
| 3-plane | Scout | GRE | |
| Sagittal | T1 W | TSE or 3D GRE | Thin (1 mm) slices |
| Axial | T2 W | TSE | Fat suppression |
| Axial | IR | FLAIR | |
| Axial | DWI | ||
| Axial | T1 W | TSE | Thin (1 mm) slices |
| Axial | CISS | 3D | Thin (0.6 mm) slices |
| Axial and coronal (+GD) | T1 W | TSE | Thin (1 mm) slices |
| Axial (+GD) | T1 W | TSE | Brain |
Pathologic conditions
CN VII: Facial Nerve
Facial palsy presents clinically with ipsilateral facial drop and difficulty in facial expression, pain around the jaw or behind the ear, increased sensitivity to sound, decreased ability to taste, headache, and changes in the amount of tears and saliva produced. It is crucial for clinicians to determine whether the forehead muscles are spared, which reflects pathology in the cerebral hemispheres (central facial palsy); or are affected, which implicates pathology in the facial nerve itself (peripheral facial palsy).
After gadolinium administration, a thorough evaluation of all portions of the facial nerve is essential to detect areas of abnormal enhancement. Enhancement of the intracanalicular portion (which extends from the opening to the fundus of the IAC) and/or the labyrinthine portion (which extends from the fundus of the IAC to the facial hiatus) is always abnormal. The remaining portions of the nerve, as well as the geniculate ganglion, may normally enhance. In the case of abnormal facial nerve enhancement, the differential diagnosis includes Bell palsy, schwannoma, hemangioma, acute otitis media, lymphoma, sarcoidosis, viral neuritis, perineural tumor spread, Lyme disease, and Guillain-Barré and Ramsay-Hunt syndromes.
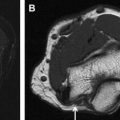
In Bell palsy, there is enhancement of the intracanalicular and/or the labyrinthine portion of the ipsilateral facial nerve ( Fig. 5 ), whereas some authors have also reported higher signal intensity ratio of the geniculate ganglion and tympanic segment on the affected side than on the normal side. The affected segment maintains linear morphology without any nodularity, and may be normal in size or slightly enlarged. Although the diagnosis of Bell palsy is typically clinical, MRI is reserved for patients in whom nerve decompression is planned, when there is suspected mass lesion in nonresolving neuropathy, or when there are indeterminate results of electromyography. Imaging can be used to confirm potential swelling of the nerve proximal to the meatal foramen and to detect any associated mass lesion.
Schwannoma may develop in any portion of the facial nerve, although it has a predilection for the region of the geniculate ganglion. Typically, it presents as a well-demarcated space-occupying lesion, which is isointense to hypointense relative to gray matter on T1 weighted images and moderately hyperintense of T2 weighted images, and enhances homogeneously after gadolinium administration. Larger lesions undergo internal bleeding, presenting as hyperintense zones on T1 weighted images, or cystic degeneration or necrosis appearing as hyperintense areas on T2 weighted images. CT demonstrates bony scalloping and remodeling rather than destruction.
Facial nerve venous vascular malformation (previously described as facial nerve hemangioma) also shows predilection for the geniculate ganglion. In the latter location, the lesion may be isointense to adjacent brain and only detectable on contrast-enhanced T1 weighted images, where it is expected to enhance intensely. Hemangiomas have similar signal characteristics compared with schwannomas, although in the former, the bony margins are indistinct, enabling differentiation from the latter, which feature well-defined remodeled margins. In addition, hemangiomas containing bone may feature foci of low signal intensity on MRI, and bone spicules or honeycomb morphology on CT. Associated widening of the facial nerve canal is sometimes present. Meningiomas infrequently arise in the geniculate ganglion, are not readily differentiated from hemangiomas on imaging studies, and are included in the differential diagnosis solely based on the aforementioned location.
In acute otitis media, there is obvious T2 hyperintensity and contrast enhancement of the tympanic segment of the facial nerve, although findings are difficult to assess because of the inflammation of the adjacent tissues. MRI is helpful in determining the degree of facial nerve involvement, as well as potential extension of the inflammation within the otic capsule and epidural and intradural spaces.
Perineural spread of parotid malignancies and squamous cell carcinoma of the parotid or face may occur along the facial nerve. MRI demonstrates enlargement and enhancement of the involved nerve portion and commonly secondary enlargement of the stylomastoid foramen. The facial nerve may be involved by neurosarcoidosis and Lyme disease, and demonstrates nerve enhancement as well as diffuse or multifocal nodular enlargement, which tends to regress after therapy. In Guillain-Barré syndrome, facial nerve involvement is acute, typically bilateral, and presents with enhancement.
The facial nerve is susceptible to injury in cases of temporal bone fractures. In transverse fractures, the facial nerve is injured in up to 40% of cases, whereas in longitudinal fractures, it is injured in about 10% to 20% of cases. CT is the modality of choice for assessing the integrity of the facial canal, while the role of MRI is limited in these situations.
CN VIII: Vestibulocochlear Nerve
Dysfunction of the vestibular branch of CN VIII presents clinically with dizziness, vertigo, disequilibrium, imbalance, ataxia, nausea, and/or vomiting. When the cochlear branch is affected, manifestations include tinnitus or ear ringing, poor hearing ability, or even deafness. Combinations of the aforementioned symptoms indicate simultaneous involvement of both nerve branches.
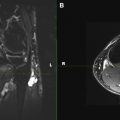
Schwannomas of the vestibulocochlear nerve (acoustic neuromas) usually develop as combined intracanalicular–cisternal masses, and less commonly as purely intracanalicular, extracanalicular, or intralabyrinthine lesions ( Figs. 6 and 7 ). The lesions show the typical signal and enhancement characteristics of schwannomas, as previously described. In the IAC, intracanalicular lesions as well as segments of mixed intracanalicular–cisternal lesions demonstrate a funnel-shaped (ice cream cone) appearance with posterolateral epicenter on axial images and a short club-shaped configuration on coronal images. In larger lesions, CT may demonstrate erosion of the temporal bone, which is limited to the boundaries of the IAC.