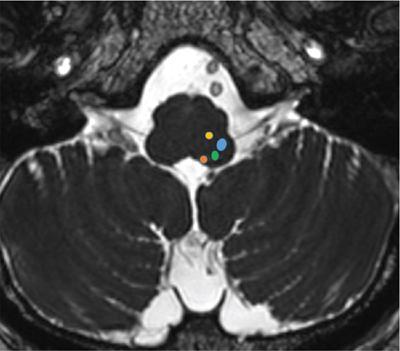
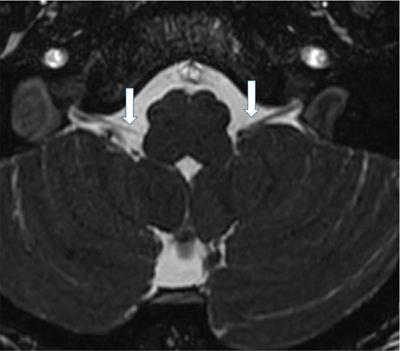
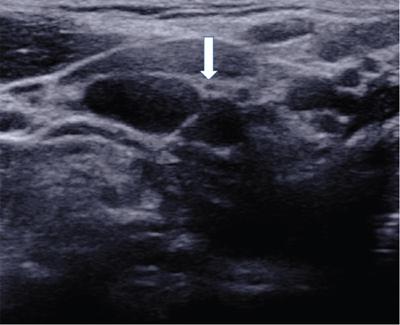
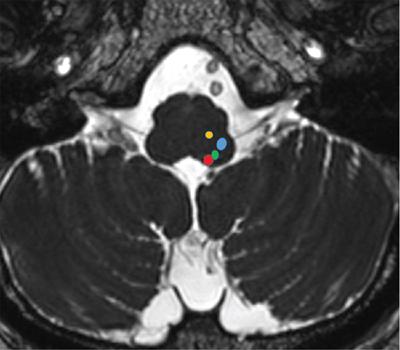
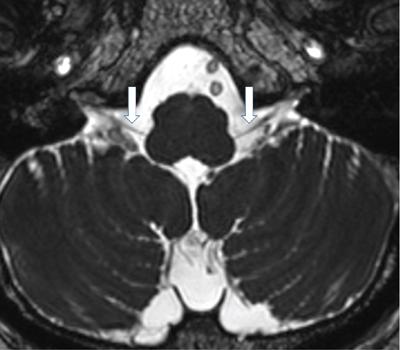
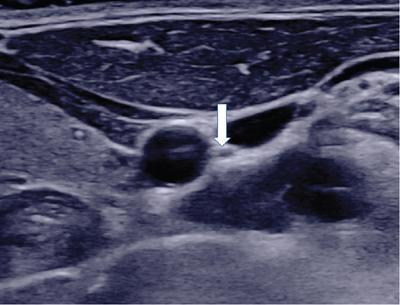
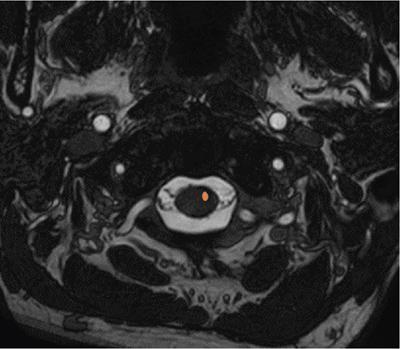
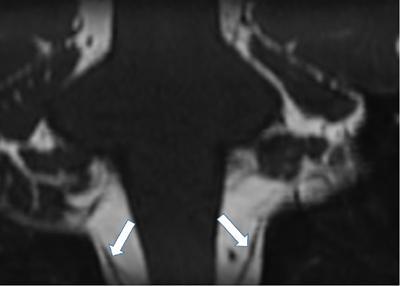
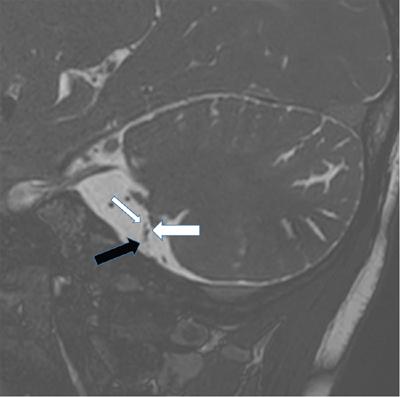
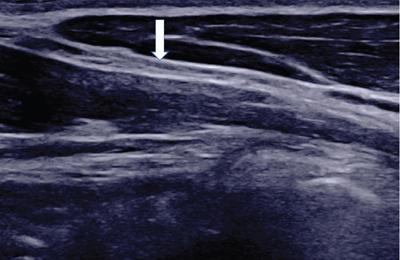
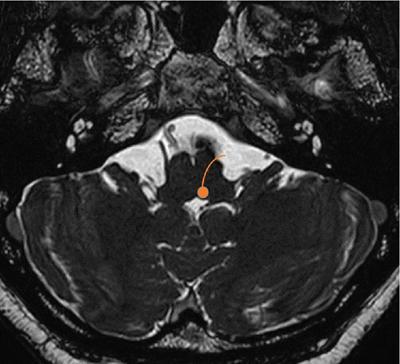
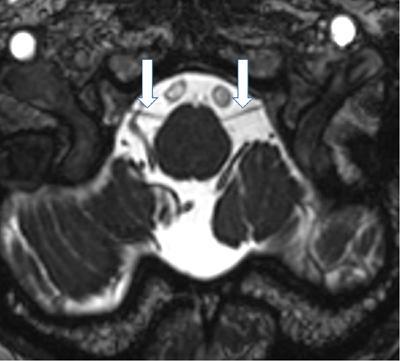
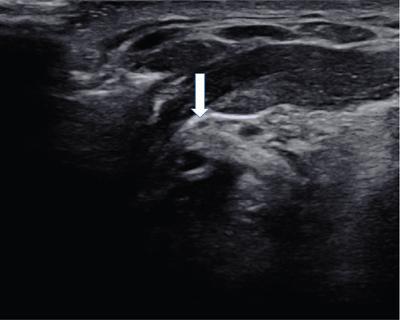
C Seetharaman, Shriram Varadharajan, Meena Nedunchelian, Athira LEARNING OBJECTIVES KEY POINTS Cranial nerves (CN) encompass 12 pairs of symmetrical nerves that arise from the supratentorial cerebrum (I, II) and infratentorial brainstem (III–XII). Lower cranial nerves (LCN) include the paired CN IX (glossopharyngeal), CN X (vagal), CN XI (accessory) and CN XII (hypoglossal) nerves. They aid (especially CN IX, X and XII) in the execution of important physiological functions like swallowing, tasting, speech, heart rate and blood pressure control, and peristalsis. Lower cranial nerves (LCNs) dysfunction may exist in isolation or in association with other symptoms or signs and can be caused by multiple pathologies. LCN imaging needs detailed anatomical knowledge and various technical considerations for proper evaluation of lower cranial nerve pathologies as well as planning the treatment. Radiologists play a major role in selecting the most appropriate imaging modality, planning the protocol and extent of coverage after detailed analysis of medical history, clinical examination and other relevant reports. In this chapter we discuss lower cranial nerves in 2 sections – intracranial and extracranial portions separately with special emphasis on applied anatomy, imaging techniques, differentials and approach to various lower cranial nerve disorders. The glossopharyngeal nerve is a mixed nerve with sensory, motor and parasympathetic functions. The glossopharyngeal nerve derives from third pharyngeal arch. The glossopharyngeal nuclei are located in upper and middle medulla. The nuclei include 1. Nucleus ambiguus (motor fibres to stylopharyngeus) 2. Inferior salivatory nucleus (preganglionic parasympathetic neurons to otic ganglion and then to parotid gland) 3. Nucleus of tractus solitarius (taste from posterior 1/3 of tongue and information from carotid sinus baroreceptors and carotid body chemoreceptors) and 4. Spinal trigeminal nucleus (Somatic sensory fibres from internal surface of tympanic membrane, middle ear, upper part of pharynx, soft palate and posterior 1/3 of tongue. Nucleus ambiguous is shared by IX, X and XI cranial nerves. The corresponding fascicular segments join to form the glossopharyngeal nerve (Fig. 3.29.1). The IX th nerve exits the brainstem in post-olivary sulcus, and courses through lateral cerebellomedullary cistern in anterolateral direction and is closely associated with flocculus of cerebellum. The glossopharyngeal nerve is closely associated with vagus and bulbar portion of accessory nerve and is difficult to see them separately in routine sequences but can be adequately visualized in thin section/3D T2 images (Fig. 3.29.2). The glossopharyngeal nerve then enters smaller anteromedial portion (pars nervosa) of jugular foramen. Still within the foramen, glossopharyngeal nerve shows two focal expansions, namely superior and inferior (Andersch) nodes, about 3 mm apart. The tympanic (Jacobson) nerve is the first branch that leaves the glossopharyngeal nerve from lower node and contributes to tympanic plexus in middle ear.The nerve can only be distinguished inside the jugular foramen on axial and reformatted coronal high-resolution post contrast T1 images. Immediately after leaving the jugular foramen, the GPN enters retro styloid (carotid) space and is located medial to internal jugular vein and behind internal carotid artery. Styloid process is the most lateral reference at this level. At the level of C1 transverse process, the nerve goes around carotid artery laterally and descends behind styloid process and stylopharyngeus muscle and comes anterior to vascular structures. When it crosses between internal carotid artery and internal jugular vein, the GPN gives off the carotid sinus and carotid body nerve (Hering’s nerve). The GPN enters the pharynx between upper and middle constrictors at the level of stylopharyngeus muscle merging with constrictor muscles and finally ends in posterior sublingual space as lingual nerve. The other nerves arising from GPN are Stylopharyngeal nerve, pharyngeal and tonsillar branches as well as communicating branch to vagus nerve. GPN is also involved in afferent limbs of gag and cough reflex. The nerve could not be normally visualized in routine CT and MRI images, but can be seen in HRUS in suprahyoid carotid space anterior to ICA and IJV. MR Neurography is also useful (Fig. 3.29.3). The vagus nerve is the longest cranial nerve in the body and is a mixed nerve with sensory, motor and parasympathetic functions. The vagus nerve arises from fourth branchial arch. Pharyngeal and laryngeal muscles, laryngeal cartilages, aortic arch and subclavian artery also develop from this arch. The vagal nerve includes axons which synapse with four nuclei in medulla. 1. Dorsal nucleus of vagus nerve (general visceral efferent fibres that sends parasympathetic signals to heart and lungs and innervate gastrointestinal smooth muscles and glands). 2. Nucleus ambiguus (efferent special visceral branchiomotor fibres that provide motor innervation for swallowing and phonation). 3. Nucleus tractus solitarius (receives afferent taste information and primary afferents from visceral organs) 4. Spinal trigeminal nucleus (receives input from pinna of the ear regarding deep touch, pain and temperature and receives sensory information from posterior cranial fossa dura and laryngeal mucosa. The corresponding fascicular segments join to form the vagus nerve. Posterior inferior cerebellar artery delivers vascular supply to the lateral portion of medulla including all the nuclei (Fig. 3.29.4). The vagus nerve exits the brainstem just below the ninth nerve in post olivary sulcus, enters the lateral cerebellomedullary cistern and courses along the inferior aspect of ninth nerve through the cistern (Fig. 3.29.5). The vagus nerve then enters larger posterolateral portion (pars vascularis) of jugular foramen along with spinal accessory nerve. The vagus nerve contains superior vagal ganglion (located in jugular foramen) and inferior vagal ganglion (located just below the skull base). Arnold nerve or auricular branch is the first branch of 10th nerve arising from superiorvagal ganglion. The nerve can be seen in the jugular foramen on contrast enhanced T1 images. The nerve descends vertically within the carotid sheath, posterolateral to internal and common carotid arteries and medial to internal jugular vein (IJV) to enter the upper mediastinum, anterior to subclavian artery on right side and anterior to aortic arch on left side. Other major branches in the neck include pharyngeal branches, carotid body branches, superior laryngeal nerve dividing into internal and external laryngeal nerves and recurrent laryngeal nerves. The recurrent laryngeal nerve ascends in tracheoesophageal groove after looping around subclavian artery on right and passing through the aortopulmonary window on left side and provides motor innervation to all laryngeal muscle except cricothyroid muscle. It finally enters the abdomen through the esophageal hiatus. HRUS can be used to track the nerve in the neck region (Fig. 3.29.6). The accessory nerve is a pure motor nerve, innervating sternocleidomastoid, and trapezius muscles. The embryological development of XI nerve is from ganglionic crest (ectoderm), same as that of vagus nerve. Interesting fact to note is that the spinal accessory nerve is the only cranial nerve to enter and exit the skull. The accessory nerve has both cranial and spinal roots. The bulbar motor fibres have their origin in nucleus ambiguous and the spinal motor fibres in spinal nucleus of accessory nerve. The spinal nucleus is situated lateral to anterior horns from C1 to C5 levels and the fibres exit cervical spinal cord in the lateral aspect between anterior and posterior roots (Fig. 3.29.7). The spinal nerve fibres then form an ascending nerve which reaches the jugular foramen after traversing through the foramen magnum. The bulbar cisternal segment is located just below the 10th nerve and exits in post olivary sulcus. The bulbar and spinal portions of the nerve join in the lateral part of basal cistern to form a single nerve. The intracranial portion is vascularized by branches of PICA and spinal roots by branches of ascending pharyngeal artery and anterior spinal artery (Figs. 3.29.8 and 3.29.9). The conjoined roots enter the larger pars vascularis of jugular foramen, posterior to IX and X CNs. Within the jugular foramen, cranial roots mix with Xth CN at the level of superior vagal ganglion. Once the XI nerve exits the jugular foramen, it separates into internal and external branches. The internal branch is composed of fibres from cranial part and contributing to vagal function of pharyngeal and laryngeal areas. The outer branch is mainly from spinal part, as well as receives innervation from C1–C4 and innervate the trapezius and sternocleidomastoid muscles. The spinal part, after its exit from the jugular foramen, runs backward in front of internal jugular vein in 2/3rd of cases and behind it in 1/3rd of cases.The XI passes along the internal surface of the sternocleidomastoid (SCM) and sends branches without penetrating the muscle (type A); a single branch, without penetrating the muscle (type B), or penetrating the muscle deeply (type C). The nerve traverses the posterior triangle and ends in deep surface of trapezius muscle. High resolution ultrasound can be used for tracing the nerve in upper neck and posterior triangle regions.Variable anastomosis between the accessory nerve and root of C1, stellate ganglion, IX cranial nerve and Vagus at level of C1 transverse process (Lobstein anastomoses) are also seen (Fig. 3.29.10). The hypoglossal nerve is a motor nerve, innervating intrinsic and extrinsic muscles of tongue except palatoglossus. Hypoglossal nerve originates from the somatic efferent column of the brainstem. The nucleus is located in lower medulla, in posterior paramedian position in the floor of fourth ventricle producing a slight bulge (hypoglossal eminence). The nucleus is seen medial to dorsal nucleus of the vagus nerve. Axons travel anterolaterally through the medullary tegmentum and exits the brainstem in pre-olivary sulcus (Fig. 3.29.11). The nerve emerges as a series of rootlets that converge to form a single or double-root hypoglossal nerve. The nerve traverses lateral cerebellomedullary cistern, in close proximity to V4 segment of vertebral artery and posterior inferior cerebellar artery (PICA). The segment is best seen on thin section/3D T2W images (Fig. 3.29.12). The nerve leaves the skull via the hypoglossal canal, located below the jugular foramen in the inferior occipital bone. At this level, the nerve is visible as linear structure surrounded by venous plexus in T2 and post contrast T1 images. The nerve exits the skull, enters carotid space and descends medial to other lower cranial nerves. The nerve leaves the carotid space at the level of posterior belly of digastric muscle, runs inferolaterally towards the hyoid bone and passes lateral to carotid bifurcation. The muscular branch then enters the tongue lateral to hyoglossus muscle in posteriors ublingual space and gives end branches for the tongue musculature. The hypoglossal nerve consists of four branches including meningeal, descending, thyrohyoid and muscular branches. Only the muscular branch is considered part of the real hypoglossal nerve originating from the hypoglossal nucleus. Other branches originate from spinal nerves (mainly C1/C2) or the cervical ganglia. High resolution ultrasound can be used for tracing the nerve in posterior sublingual region (Fig. 3.29.13 and Table 3.29.1). Pharynx (S, M) Synergic with vagus nerve Pharynx (S, M) Larynx(M) Thoracic and abdominal viscera (parasympathetic) Motor to SCM, trapezius Motor to tongue muscles Lower cranial nerve dysfunction can produce diverse abnormalities ranging from motor and sensory disturbances in laryngopharyngeal regions, tongue, neuralgia, autonomic disturbances like alterations in heart rate and blood pressure, breathing abnormalities and weakness of head rotation and shoulder elevation. These depend upon single or multiple nerve involvement as well as the segment of the nerve involvement. If additional neural or non-neural structures are involved, symptomatology may be even broader (Table 3.29.2). Lesions of the LCN can be approached in multiple different perspectives. It could be classified according to number of involved nerves (single vs multiple), depending upon loss of function (motor vs sensory), associated additional pathology of brain, spinal cord/spinal nerves, or based on cause of the lesion (like genetic, vascular, traumatic, iatrogenic, infectious, metabolic or neoplastic). However, the more practical and reproducible form of classification of LCN pathology is based on the segmental approach along the entire length of lower cranial nerves from its medullary origin to the end organs. Functional anatomy of lower cranial nerves can be considered by organizing them in various segments as follows: (1) Intraaxial segment including nuclei and fascicular nerve (2) Cisternal segment (3) Skull base segment including foramen/canal (4) Extracranial segment and (5) Infrahyoid neck or mediastinal segments. With this organization, a reasonable differential diagnosis can be achieved for pathologic findings in each segment (like infectious or inflammatory, traumatic, neoplastic, or miscellaneous, etc.) like in Table 3.29.3.
3.29: Lower cranial nerves imaging (9–12th nerves)
Abbreviations
Introduction
Imaging anatomy of lower cranial nerves
IXth cranial nerve – glossopharyngeal nerve
Intraaxial segment
Cisternal segment
Skull base segment
Extracranial (cervical) segment and its branches
Xth cranial nerve – vagus nerve
Intraaxial segment
Cisternal segment
Skull base segment
Extracranial (cervical) segment and its branches
XI cranial nerve – accessory nerve
Intra axial segment
Cisternal segment
Skull base segment
Extracranial segment
XII cranial nerve – hypoglossal nerve
Intraaxial segment
Cisternal segment
Skull base segment
Extracranial segment
Nerves
Nuclei
Exit from Medulla
Foramen
Branches
Function
IX Glossopharyngeal
Post olivary sulcus
Pars nervosa of jugular foramen
Jacobson, Hering’s, stylopharyngeal, pharyngeal, tonsillar and communicating branch to vagus
X Vagus
Post olivary sulcus
Pars vascularis of jugular foramen
Arnold, pharyngeal, carotid body branches, superior and recurrent laryngeal nerves
XI Accessory
Post olivary sulcus
Pars vascularis of jugular foramen
No collateral branches
XII hypoglossal
Hypoglossal nucleus
Preolivary sulcus
Hypoglossal canal
No collateral branches
Clinical manifestations
Imaging approach to assess lower cranial nerve pathology
Brainstem or Nuclear Segment
Cisternal
Skull Base/Foraminal
Suprahyoid Segment
Infrahyoid/Mediastinal Segment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine





