The arteries of the lower extremities are commonly affected by atherosclerosis, trauma, and thromboembolism. Advanced vascular disease frequently results in limb loss and decreased life expectancy. In this chapter, key collateral pathways, noninvasive physiologic evaluation techniques, and imaging techniques, and imaging of various vascular disorders of the lower extremity arteries are discussed.
Collateral Pathways of the Lower Extremity Arteries
Extensive collateral pathways exist between the pelvic arteries and the profunda femoris artery. In the presence of common femoral artery occlusion, the profunda femoris artery receives blood flow from the branches of the internal iliac artery through the pudendal arteries, from the lumbar arteries through the lateral circumflex iliac artery and the lateral circumflex femoral artery, and from the contralateral profunda femoris artery through the external pudendal arteries. The muscular branches of the profunda femoris artery supply the distal superficial femoral artery in the presence of proximal superficial femoral artery occlusion ( Fig. 48-1 ). Similarly, in the presence of distal superficial femoral artery occlusion, the profunda femoris artery reconstitutes the popliteal artery through the geniculate arteries. The geniculate branches of the superficial femoral artery and the muscular branches of the profunda femoris artery reconstitute the distal popliteal artery in the presence of proximal popliteal artery occlusion, whereas the sural and geniculate branches reconstitute the tibial arteries in the presence of distal popliteal artery occlusion. Similarly, the sural and geniculate arteries collateralize the tibial arteries in the presence of proximal tibial artery occlusion. Multiple cross-tibial collateral vessels exist among the anterior tibial, posterior tibial, and peroneal arteries. The plantar arch provides an excellent collateral pathway in the foot in the event of occlusion of either the dorsalis pedis artery or the posterior tibial artery.

Pearls and Pitfalls
- 1.
The profunda femoris and peroneal arteries are the key pathways in maintaining leg perfusion in the event of occlusion of the major arteries in the leg.
- 2.
Often, flow through the collateral vessels can be robust, resulting in normal pedal pulses despite occlusion of the superficial femoral artery.
- 3.
When occlusive disease affects the common femoral artery, imaging of the abdominal and pelvic vessels is important, to assess the collateral supply to the leg.
Noninvasive Physiologic Evaluation
Noninvasive evaluation of lower extremity arterial disease is important in assessing the physiologic impact of the occlusive disease because the severity of the occlusive process does not often correlate with the symptoms. For example, good collateral supply in the presence of superficial femoral artery occlusion may result in normal distal pulses, and the patient may remain asymptomatic. Noninvasive physiologic evaluation provides objective means to assess the severity of the disease and helps monitor disease progression and outcomes of various therapies. Commonly used physiologic tests include the ankle-brachial index (ABI), segmental limb pressures, and pulse volume recordings (PVR) ( Fig. 48-2 ). These tests can be performed at rest and after standardized exercise. Occlusive disease that is well compensated at rest may be unmasked on exercise testing. Physical examination is part of noninvasive evaluation; skin integrity, temperature, capillary refill, and palpable pulses can be assessed.

Ankle-Brachial Index
The ABI refers to the ratio of the highest upper arm pressure on either side to the highest ankle pressure obtained through Doppler evaluation of the dorsalis pedis and posterior tibial arteries at the ankle by using appropriately sized blood pressure cuffs and continuous wave Doppler imaging. The ABI provides information about the presence and severity of peripheral arterial disease, but it does not contain information about the level of the occlusive process. An ABI of 1 or more indicates the absence of peripheral arterial disease, and a lower ABI usually correlates with the severity of occlusive disease ( Table 48-1 ). The ABI may be falsely elevated in the presence of noncompressible arteries, as often seen in diabetes as a result of calcific medial sclerosis. In such cases, the toe-brachial index (normal >0.6) is a useful measure to assess disease severity because the digital arteries are rarely affected by calcific medial sclerosis. During exercise, the ABI remains normal or elevated in the absence of peripheral arterial disease.
| Ankle-Brachial Index | Disease Severity |
|---|---|
| >0.95 | None |
| 0.75-0.95 | Mild peripheral arterial disease |
| 0.5-0.75 | Moderate peripheral arterial disease |
| 0.3-0.5 | Severe peripheral arterial disease |
| <0.3 | Critical |
Segmental Limb Pressures
The segmental limb pressure test consists of obtaining blood pressure measurements at the thigh, calf, and ankles with appropriately sized blood pressure cuffs. A drop of 20 to 30 mm Hg pressure at any level or a difference of more than 20 mm Hg compared with the opposite side indicates hemodynamically significant occlusive disease in that vascular segment. The test is usually combined with Doppler evaluation of arterial flow at each level. Doppler analysis of the arterial waveform provides information about the presence and severity of occlusive disease. The normal Doppler pattern of peripheral arteries is triphasic. In the presence of occlusive disease, the arterial waveform becomes monophasic, with decreased amplitude.
Pulse Volume Recordings
PVRs are obtained by applying appropriately sized blood pressure cuffs at various levels in the thigh, calf, and ankle, inflating the cuffs to 60 to 65 mm Hg pressure, and recording the changes in the pressure in the cuff. The pressure changes within the cuff represent changes in the blood volume during systole and diastole. These recordings are in a waveform. The waveforms are assessed for changes in amplitude and contour. Loss of the normal dicrotic notch and flattening of waveforms indicate the presence of peripheral arterial disease at that vascular segment.
Pearls and Pitfalls
- •
Physiologic evaluation of limb arteries through the ABI, segmental limb pressures, and PVRs provides information about the presence, severity, and location of disease.
- •
In the presence of a normal ABI at rest, exercise testing provides information about occult or subclinical disease.
- •
The ABI may be falsely elevated in the presence of noncompressible arteries; in such cases, toe pressures should be obtained.
- •
Physiologic testing can be performed to assess cold-induced digital ischemia. The test should be repeated after cold exposure to the hand, to assess changes in leg perfusion.
Imaging Techniques
Imaging evaluation of the peripheral arteries is indicated to assess the presence and location of occlusive or aneurysmal disease that is suspected on physiologic evaluation or when arteriovenous shunting (fistulas or malformation or tumor) is suggested, as well as to localize a bleeding vessel. Imaging studies should be interpreted with concurrent knowledge of the patient’s symptoms, earlier surgical procedures, and results of physiologic tests. Various imaging modalities are used to assess lower extremity arteries.
Color Doppler Ultrasound
Color Doppler ultrasound allows evaluation of the superficial arteries and bypass grafts. Every arterial segment is evaluated with grayscale, color flow, and spectral Doppler imaging, with special emphasis on peak systolic velocity and Doppler waveforms. Stenosis of 50% or more is suspected when the peak systolic velocity is twice or more than that of the proximal arterial segment. A peak systolic velocity four times or more than that of the proximal arterial segment suggests 75% or more luminal narrowing. Occlusion is seen as absence of flow on color flow imaging and spectral Doppler.
On spectral Doppler imaging, peripheral arteries demonstrate a triphasic flow pattern. At the site of stenosis, the waveforms become monophasic or biphasic with increased peak systolic velocity, whereas distal to a hemodynamically significant stenosis, the waveforms become monophasic with a tardus parvus pattern ( Fig. 48-3 ). The presence of a distal arteriovenous communication results in a monophasic flow pattern with increased diastolic flow but preserved systolic upstroke. In addition, arterialized waveforms are seen in the draining veins. Color Doppler flow settings must be adjusted to evaluate arteries with slow flow distal to an occlusion and to assess the digital arteries.

Computed Tomography Angiography
Computed tomography (CT) angiography (CTA) with multidetector CT technology provides excellent soft tissue resolution. Advances in dual energy CT allow accurate identification of calcium and contrast material and thus allow less blooming artifact from dense calcium. Dual energy CTA permits excellent subtraction of calcium from contrast-enhanced arteries and therefore provides calcium-free three-dimensional (3-D) maximum intensity projections.
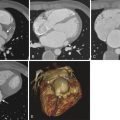
Current 64-slice scanners allow scanning of the entire abdomen and lower extremities in a few seconds, with extended scanning within a single breath hold even in sick patients. However, such fast scanning can be a problem when assessing asymmetric aortoiliac and peripheral arterial occlusive disease. The scanner may run faster than the contrast material in the diseased leg, with resulting poor contrast opacification of the distal arteries. In such cases, a delayed scan of the diseased territory is helpful, to limit false interpretation of occluded arteries. In addition, the scanner parameters must be adjusted to improve intravascular contrast and reduce the radiation dose. Such adjustments include applying lower peak kilovoltage (80 to 100 kVp instead of 120 to 140 kVp), automated current adjustment, autotriggered timing of the scan, adequate contrast material (4 to 6 mL/second, to a total volume of 90 to 120 mL), and submillimeter slice thickness. The axial scan data are reconstructed in coronal and sagittal planes, 3-D maximum intensity projections ( Fig. 48-4 ), 3-D surface shaded display, and 3-D volume rendered images. These images provide a catheter angiography–like picture of the arterial tree and allow assessment of the longitudinal extent of the occlusive disease. Reconstructed true axial scans provide accurate assessment of luminal narrowing.

Magnetic Resonance Angiography
Both noncontrast and contrast-enhanced magnetic resonance angiography (MRA) techniques provide means for assessing the lower extremity arteries. The sensitivity and specificity of contrast-enhanced MRA exceed 95% for detecting 50% or greater luminal stenosis. Noncontrast steady-state free precision MRA provides accurate assessment of large arterial steno-occlusive disease, whereas two-dimensional time of flight imaging provides reasonable assessment of distal arteries with slow flow.
Gadolinium-enhanced 3-D gradient recalled echo techniques allow rapid evaluation of the extremity arteries with a multistation technique (see Figs. 48-1 and 48-3 ). In addition, lower leg arterial evaluation can be supplemented by using time-resolved techniques such as time-resolved imaging with contrast kinetics (TRICKS). This approach provides highly accurate assessment of small vessel arteries. Moreover, it shows temporal changes in blood flow and thus allows detection of dominant collateral pathways in the presence of an occlusion and assessment of venous drainage pathways during evaluation of arteriovenous communications. MRA with protein-bound gadolinium allows high-resolution imaging of the arteries and veins for an accurate assessment of small vessel disease. In addition to vascular evaluation, MRA allows soft tissue and bone imaging to differentiate ischemic foot from soft tissue or bone infection, commonly encountered in diabetic patients.
Catheter Angiography
Catheter angiography remains the gold standard for evaluation of lower extremity arteries. Current angiography systems allow multistation overlapping imaging of both lower extremities with a catheter positioned in the lower abdominal aorta. Imaging through the delayed phase until all the collateral pathways are filled is important, to assess distal reconstitution in the presence of occlusion (see Fig. 48-2 ). As in CT, adequate contrast material injection and temporal acquisition are necessary. Distal abdominal aorta and pelvic arteries must be evaluated during assessments of the extremities for peripheral arterial disease. Selective catheter angiography provides high-resolution imaging of arteries of the foot and distal leg.
Pearls and Pitfalls
- •
Noninvasive physiologic tests should precede imaging evaluation of lower extremity arteries. Imaging tests provide morphologic assessment of steno-occlusive disease but little information about the physiologic impact of the disease.
- •
Color Doppler evaluation is sufficient in most cases, especially for assessing superficial native arteries and bypass grafts. Assessment of distal vessels in the presence of proximal occlusion can be misleading unless the technical parameters of color Doppler imaging are adjusted for slow flow.
- •
CTA provides accurate assessment of the longitudinal extent of disease; the blooming effects of calcium can be minimized by using dual energy scanners. Care must be used when studying asymmetric peripheral arterial disease with current scanners; delayed scanning is often required.
- •
Noncontrast MRA is a boon for patients with kidney disease. The technique allows accurate assessment of large and medium-sized arteries. However, small leg and foot arteries are best evaluated with high-resolution contrast-enhanced MRA.
- •
Catheter angiography should be limited to interventional procedures. Assessment of reconstituted distal arteries requires administration of contrast material above the origin of collateral pathways and delayed imaging of the territory in question.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree