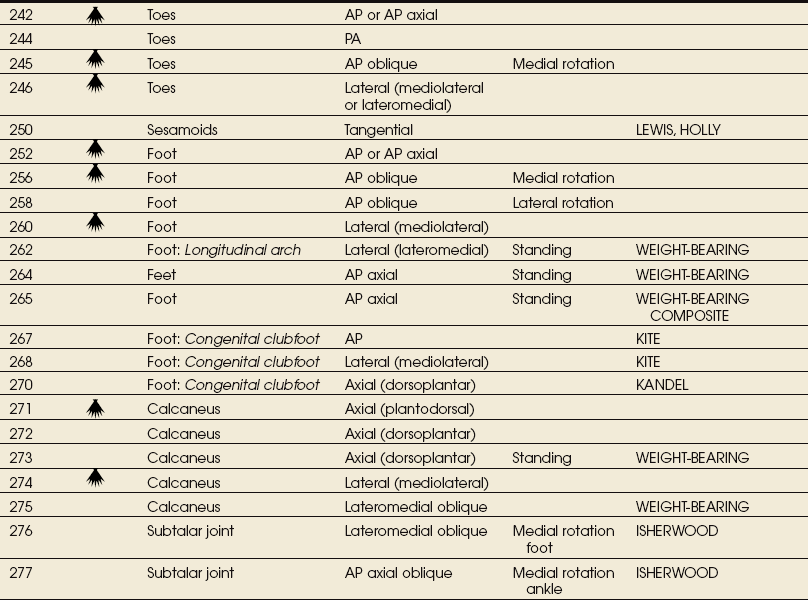
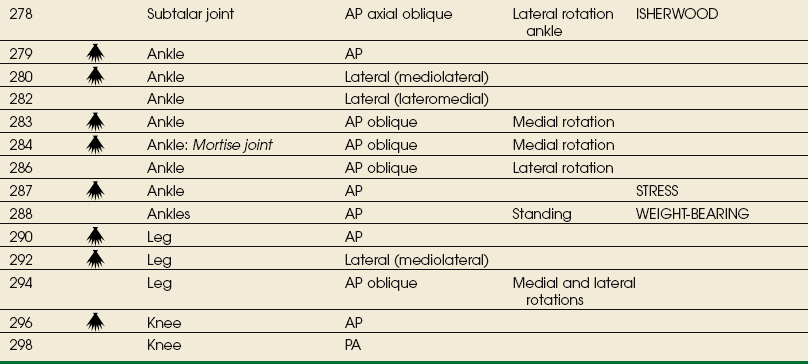
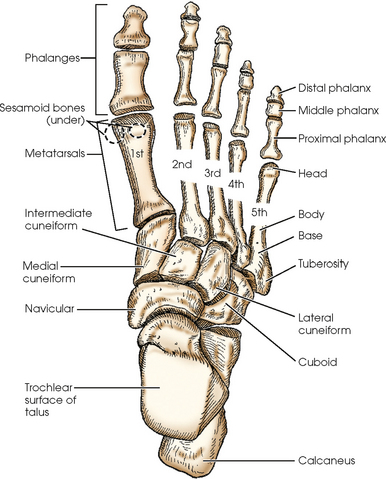
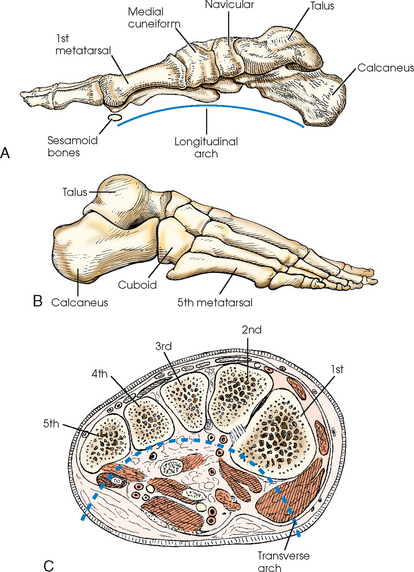
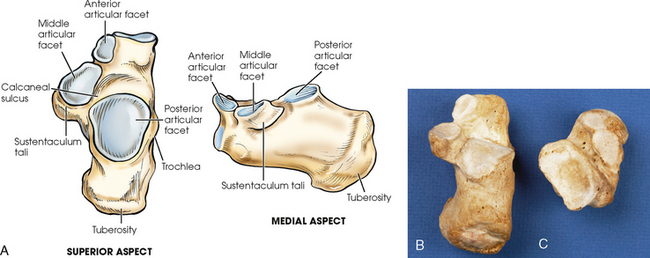
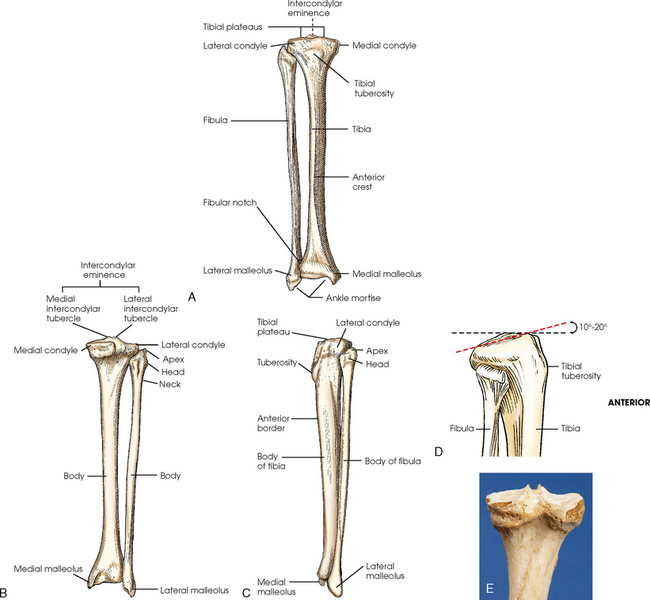
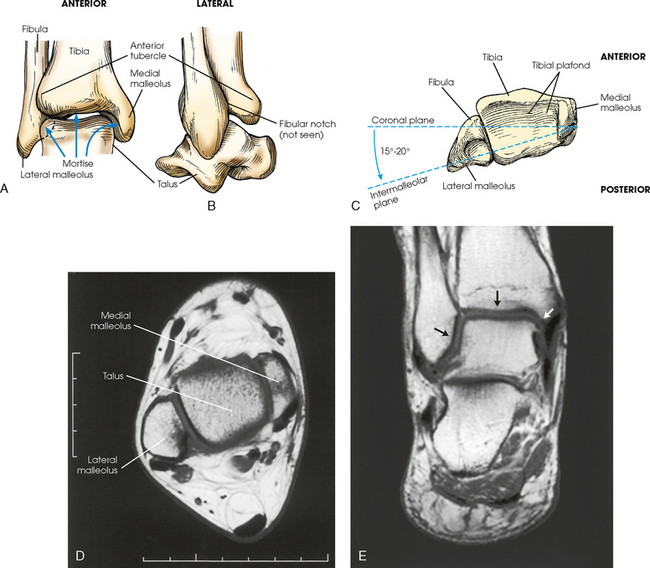
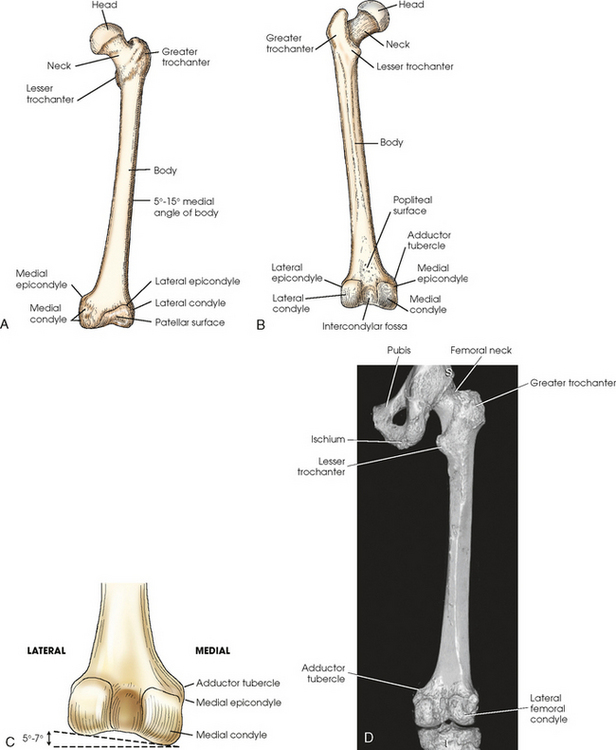
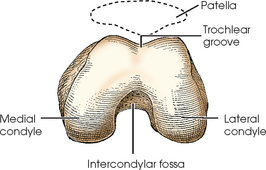
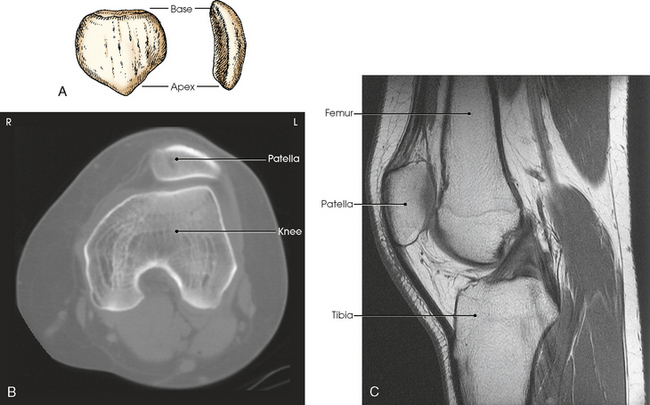
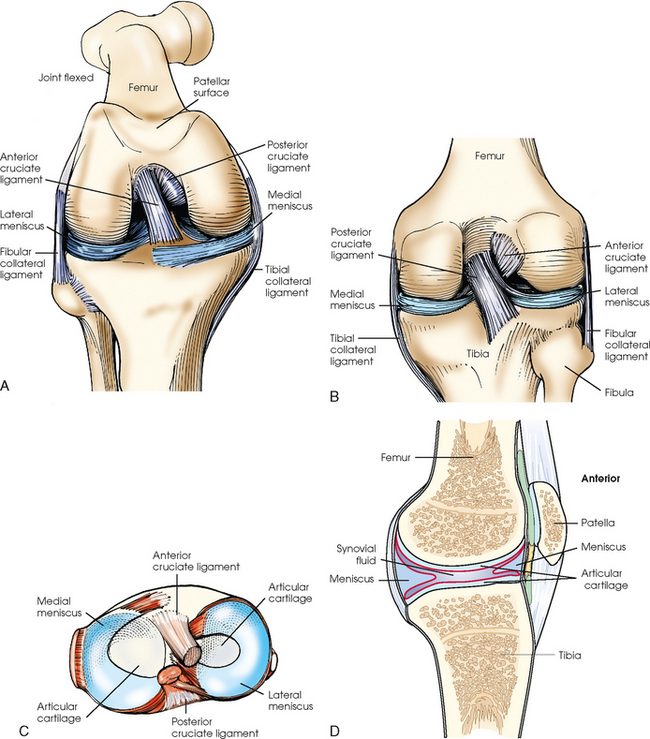
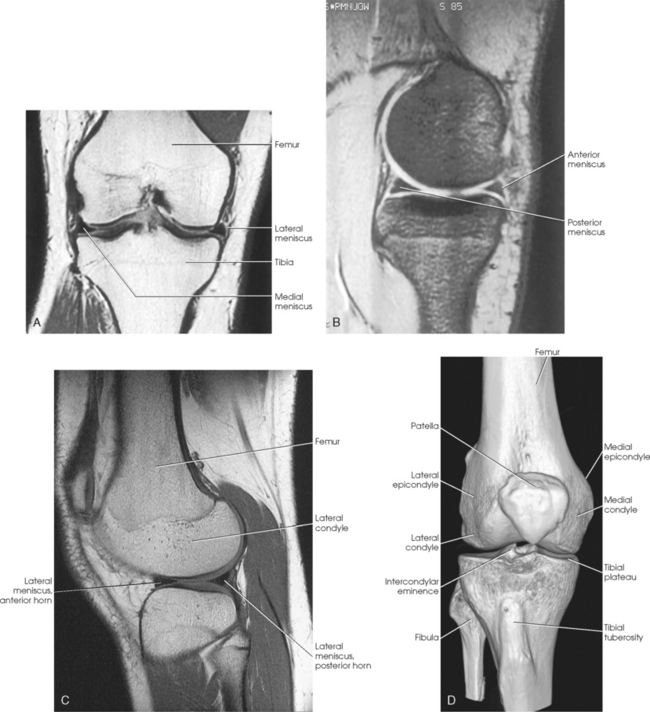
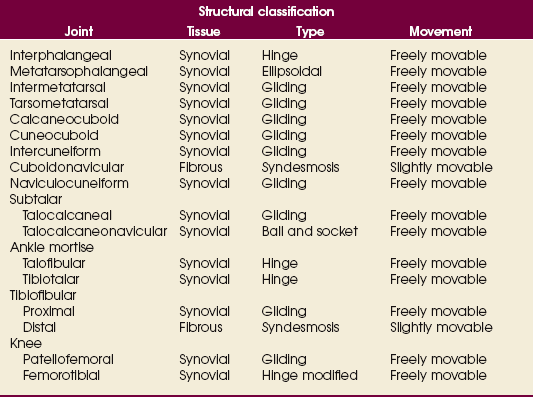
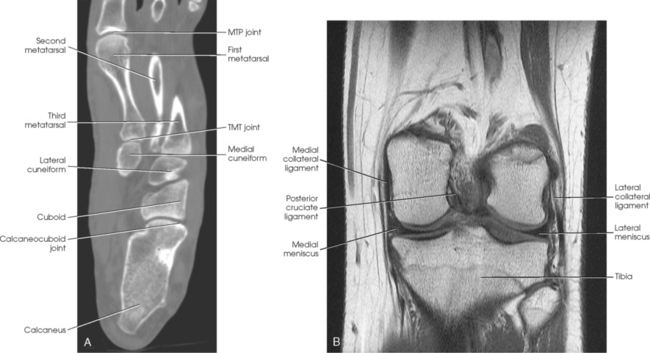
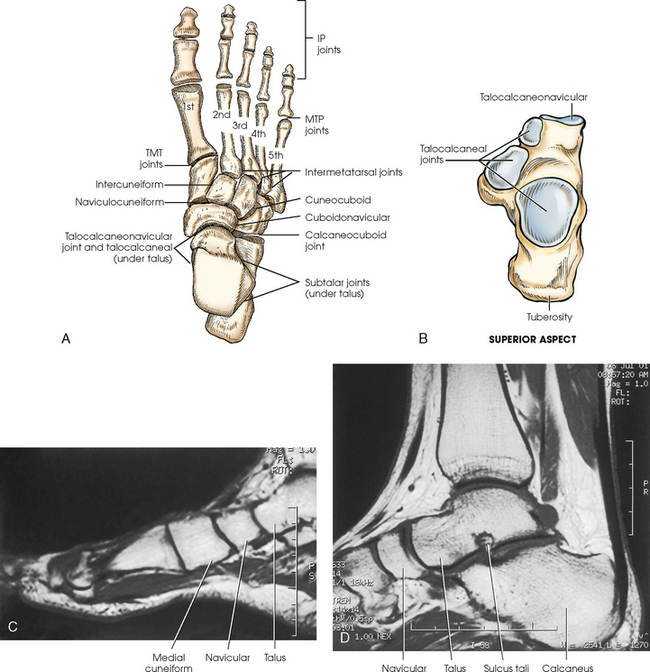
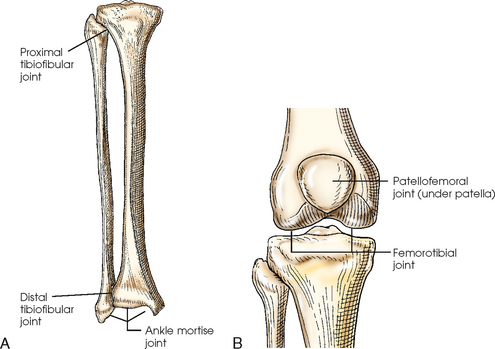
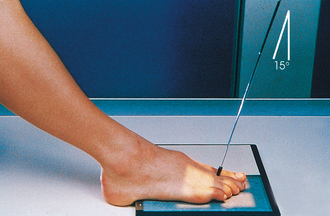
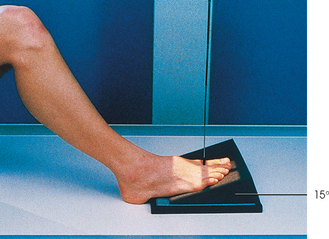
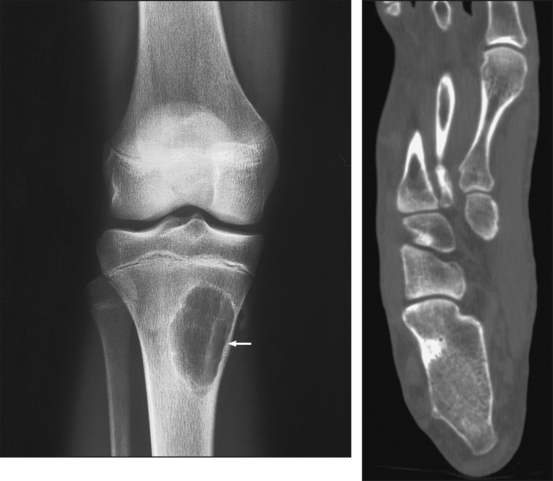
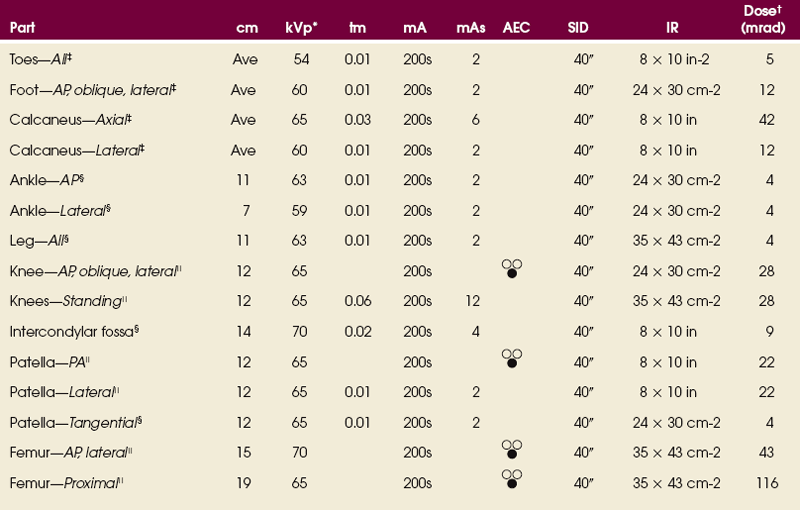
6 The lower limb, or extremity, and its girdle (considered in Chapter 7) are studied in four parts: (1) foot, (2) leg, (3) thigh, and (4) hip. The bones are composed, shaped, and placed so that they can carry the body in the upright position and transmit its weight to the ground with a minimal amount of stress to the individual parts. The foot consists of 26 bones (Figs. 6-1 and 6-2): The bones of the foot are similar to the bones of the hand. Structural differences permit walking and support of the body’s weight. For descriptive purposes, the foot is sometimes divided into the forefoot, midfoot, and hindfoot. The forefoot includes the metatarsals and toes. The midfoot includes five tarsals—the cuneiforms, navicular, and cuboid bones. The hindfoot includes the talus and calcaneus. The bones of the foot are shaped and joined together to form a series of longitudinal and transverse arches. The longitudinal arch functions as a shock absorber to distribute the weight of the body in all directions, which permits smooth walking (see Fig. 6-2). The transverse arch runs from side to side and assists in supporting the longitudinal arch. The superior surface of the foot is termed the dorsum or dorsal surface, and the inferior, or posterior, aspect of the foot is termed the plantar surface. The proximal foot contains seven tarsals (see Fig. 6-1): The calcaneus is the largest and strongest tarsal bone (Fig. 6-3). Some texts refer to it as the os calcis. It projects posteriorly and medially at the distal part of the foot. The long axis of the calcaneus is directed inferiorly and forms an angle of approximately 30 degrees. The posterior and inferior portions of the calcaneus contain the posterior tuberosity for attachment of the Achilles tendon. Superiorly, three articular facets join with the talus. They are called the anterior, middle, and posterior facets. Between the middle and posterior talar articular facets is a groove, the calcaneal sulcus, which corresponds to a similar groove on the inferior surface of the talus. Collectively, these sulci constitute the sinus tarsi. The interosseous ligament passes through this sulcus. The medial aspect of the calcaneus extends outward as a shelflike overhang and is termed the sustentaculum tali. The lateral surface of the calcaneus contains the trochlea. The talus, irregular in form and occupying the superiormost position of the foot, is the second largest tarsal bone (see Figs. 6-1 to 6-3). The talus articulates with four bones—tibia, fibula, calcaneus, and navicular bone. The superior surface, the trochlear surface, articulates with the tibia and connects the foot to the leg. The head of the talus is directed anteriorly and has articular surfaces that join the navicular bone and calcaneus. On the inferior surface is a groove, the sulcus tali, that forms the roof of the sinus tarsi. The inferior surface also contains three facets that align with the facets on the superior surface of the calcaneus. The cuboid bone lies on the lateral side of the foot between the calcaneus and the fourth and fifth metatarsals (see Fig. 6-1). The navicular bone lies on the medial side of the foot between the talus and the three cuneiforms. The cuneiforms lie at the central and medial aspect of the foot between the navicular bone and the first, second, and third metatarsals. The medial cuneiform is the largest of the three cuneiform bones, and the intermediate cuneiform is the smallest. The seven tarsals can be remembered using the following mnemonic: Beneath the head of the first metatarsal are two small bones called sesamoid bones. They are detached from the foot and embedded within two tendons. These bones are seen on most adult foot radiographs. They are a common site of fractures and must be shown radiographically (see Fig. 6-2). The tibia (Fig. 6-4) is the larger of the two bones of the leg and consists of one body and two expanded extremities. The proximal end of the tibia has two prominent processes—the medial and lateral condyles. The superior surfaces of the condyles form smooth facets for articulation with the condyles of the femur. These two flatlike superior surfaces are called the tibial plateaus, and they slope posteriorly about 10 to 20 degrees. Between the two articular surfaces is a sharp projection, the intercondylar eminence, which terminates in two peaklike processes called the medial and lateral intercondylar tubercles. The lateral condyle has a facet at its distal posterior surface for articulation with the head of the fibula. On the anterior surface of the tibia, just below the condyles, is a prominent process called the tibial tuberosity, to which the ligamentum patellae attach. Extending along the anterior surface of the tibial body, beginning at the tuberosity, is a sharp ridge called the anterior crest. The distal end of the tibia (Fig. 6-5) is broad, and its medial surface is prolonged into a large process called the medial malleolus. Its anterolateral surface contains the anterior tubercle, which overlays the fibula. The lateral surface is flattened and contains the triangular fibular notch for articulation with the fibula. The surface under the distal tibia is smooth and shaped for articulation with the talus. The fibula is slender compared with its length and consists of one body and two articular extremities. The proximal end of the fibula is expanded into a head, which articulates with the lateral condyle of the tibia. At the lateroposterior aspect of the head is a conic projection called the apex. The enlarged distal end of the fibula is the lateral malleolus. The lateral malleolus is pyramidal and marked by several depressions at its inferior and posterior surfaces. Viewed axially, the lateral malleolus lies approximately 15 to 20 degrees more posterior than the medial malleolus (see Fig. 6-5, C). The femur is the longest, strongest, and heaviest bone in the body (Figs. 6-6 and 6-7). This bone consists of one body and two articular extremities. The body is cylindric, slightly convex anteriorly, and slants medially 5 to 15 degrees (see Fig. 6-6, A). The extent of medial inclination depends on the breadth of the pelvic girdle. When the femur is vertical, the medial condyle is lower than the lateral condyle (see Fig. 6-6, C). About a 5- to 7-degree difference exists between the two condyles. Because of this difference, on lateral radiographs of the knee the central ray is angled 5 to 7 degrees cephalad to “open” the joint space of the knee. The superior portion of the femur articulates with the acetabulum of the hip joint (considered with the pelvic girdle in Chapter 7). The distal end of the femur is broadened and has two large eminences: the larger medial condyle and the smaller lateral condyle. Anteriorly, the condyles are separated by the patellar surface, a shallow, triangular depression. Posteriorly, the condyles are separated by a deep depression called the intercondylar fossa. A slight prominence above and within the curve of each condyle forms the medial and lateral epicondyles. The medial condyle contains the adductor tubercle, which is located on the posterolateral aspect. The tubercle is a raised bony area that receives the tendon of the adductor muscle. This tubercle is important to identify on lateral knee radiographs because it assists in identifying overrotation or underrotation. The triangular area superior to the intercondylar fossa on the posterior femur is the trochlear groove, over which the popliteal blood vessels and nerves pass. The patella, or knee cap (Fig. 6-8), is the largest and most constant sesamoid bone in the body (see Chapter 3). The patella is a flat, triangular bone situated at the distal anterior surface of the femur. The patella develops in the tendon of the quadriceps femoris muscle between 3 and 5 years of age. The apex, or tip, is directed inferiorly, lies ½ inch (1.3 cm) above the joint space of the knee, and is attached to the tuberosity of the tibia by the patellar ligament. The superior border of the patella is called the base. The knee joint is one of the most complex joints in the human body. The femur, tibia, fibula, and patella are held together by a complex group of ligaments. These ligaments work together to provide stability for the knee joint. Although radiographers do not produce images of these ligaments, they need to have a basic understanding of their positions and interrelationship. Many patients with knee injuries do not have fractures, but they may have torn one or more of these ligaments, which can cause great pain and may alter the position of the bones. Fig. 6-9 shows the following important ligaments of the knee: The knee joint contains two fibrocartilage disks called the lateral meniscus and medial meniscus (Fig. 6-10; see Fig. 6-9). The circular menisci lie on the tibial plateaus. They are thick at the outer margin of the joint and taper off toward the center of the tibial plateau. The center of the tibial plateau contains cartilage that articulates directly with the condyles of the knee. The menisci provide stability for the knee and act as a shock absorber. The menisci are commonly torn during injury. Either a knee arthrogram or a magnetic resonance imaging (MRI) scan must be performed to visualize a meniscus tear. The joints of the lower limb are summarized in Table 6-1 and shown in Figs. 6-11 and 6-12. Beginning with the distalmost portion of the lower limb, the articulations are as follows. The distal heads of the metatarsals articulate with the proximal ends of the phalanges at the metatarsophalangeal (MTP) articulations to form synovial ellipsoidal joints, which have movements of flexion, extension, and slight adduction and abduction. The proximal bases of the metatarsals articulate with one another (intermetatarsal articulations) and with the tarsals (tarsometatarsal [TMT] articulations) to form synovial gliding joints, which permit flexion, extension, adduction, and abduction movements. The intertarsal articulations allow only slight gliding movements between the bones and are classified as synovial gliding or synovial ball-and-socket joints (see Table 6-1). The joint spaces are narrow and obliquely situated. When the joint surfaces of these bones are in question, it is necessary to angle the x-ray tube or adjust the foot to place the joint spaces parallel with the central ray. The calcaneus supports the talus and articulates with it by an irregularly shaped, three-faceted joint surface, forming the subtalar joint. This joint is classified as a synovial gliding joint. Anteriorly, the calcaneus articulates with the cuboid at the calcaneocuboid joint. This joint is a synovial gliding joint. The talus rests on top of the calcaneus (see Fig. 6-12). It articulates with the navicular bone anteriorly, supports the tibia above, and articulates with the malleoli of the tibia and fibula at its sides. Each of the three parts of the subtalar joint is formed by reciprocally shaped facets on the inferior surface of the talus and the superior surface of the calcaneus. Study of the superior and medial aspects of the calcaneus (see Fig. 6-3) helps the radiographer to understand better the problems involved in radiography of this joint. The intertarsal articulations are as follows: The ankle joint is commonly called the ankle mortise, or mortise joint. It is formed by the articulations between the lateral malleolus of the fibula and the inferior surface and medial malleolus of the tibia (Fig. 6-13, A). The mortise joint is often divided specifically into the talofibular and tibiofibular joints. These form a socket type of structure that articulates with the superior portion of the talus. The talus fits inside the mortise. The articulation is a synovial hinge type of joint. The primary action of the ankle joint is dorsiflexion (flexion) and plantar flexion (extension); however, in full plantar flexion, a small amount of rotation and abduction-adduction is permitted. The mortise joint also allows inversion and eversion of the foot. Other movements at the ankle largely depend on the gliding movements of the intertarsal joints, particularly the one between the talus and calcaneus. The fibula articulates with the tibia at its distal and proximal ends. The distal tibiofibular joint is a fibrous syndesmosis joint allowing slight movement. The head of the fibula articulates with the posteroinferior surface of the lateral condyle of the tibia, which forms the proximal tibiofibular joint, which is a synovial gliding joint (see Fig. 6-13, A). The patella articulates with the patellar surface of the femur and protects the front of the knee joint. This articulation is called the patellofemoral joint; when the knee is extended and relaxed, the patella is freely movable over the patellar surface of the femur. When the knee is flexed, which is also a synovial gliding joint, the patella is locked in position in front of the patellar surface. The knee joint, or femorotibial joint, is the largest joint in the body. It is called a synovial modified-hinge joint. In addition to flexion and extension, the knee joint allows slight medial and lateral rotation in the flexed position. The joint is enclosed in an articular capsule and held together by numerous ligaments (see Figs. 6-9 and 6-13, B). *kVp values are for a three-phase, 12-pulse generator or high frequency. †Relative doses for comparison use. All doses are skin entrance for average adult at cm indicated. ‡Tabletop, extremity IR. Screen-film speed 100. §Tabletop, standard IR. Screen-film speed 300 or equivalent CR. Protecting the patient from unnecessary radiation is a professional responsibility of the radiographer (see Chapter 1 for specific guidelines). In this chapter, the Shield gonads statement at the end of the Position of part sections indicates that the patient is to be protected from unnecessary radiation by restricting the radiation beam, using proper collimation, and placing lead shielding between the gonads and the radiation source. Because of the natural curve of the toes, the IP joint spaces are not best shown on the AP projection. When demonstration of these joint spaces is not critical, an AP projection may be performed (Figs. 6-14 and 6-15). An AP axial projection is recommended to open the joint spaces and reduce foreshortening (Figs. 6-16 and 6-17). • With the patient in the supine or seated position, flex the knees, separate the feet about 6 inches (15 cm), and touch the knees together for immobilization. • Center the toes directly over one half of the IR (see Figs. 6-14 and 6-16), or place a 15-degree foam wedge well under the foot and rest the toes near the elevated base of the wedge (Fig. 6-18). • Adjust the IR half with its midline parallel to the long axis of the foot, and center it to the third MTP joint. • Perpendicular through the third MTP joint (see Fig. 6-14) when showing the joint spaces is not critical. To open the joint spaces, either direct the central ray 15 degrees posteriorly through the third MTP joint (see Fig. 6-16), or if the 15-degree foam wedge is used, direct the central ray perpendicularly (Fig. 6-19). • Place the toes in the appropriate position by elevating them on one or two small sandbags and adjusting the support to place the toes horizontal. • Place the IR half under the toes with the midline of the side used parallel with the long axis of the foot, and center it to the third MTP joint (Fig. 6-20). • Perpendicular to the midpoint of the IR entering the third MTP joint (see Fig. 6-20). The IP joint spaces are shown well because the natural divergence of the x-ray beam coincides closely with the position of the toes (Fig. 6-21).
LOWER LIMB
ANATOMY
Foot
TARSALS
Chubby
Calcaneus
Twisted,
Talus
Never
Navicular
Could
Cuboid
Cha
Cuneiform—medial
Cha
Cuneiform—intermediate
Cha
Cuneiform—lateral
SESAMOID BONES
Leg
TIBIA
FIBULA
Femur
Patella
Knee Joint
Lower Limb Articulations
SUMMARY OF PATHOLOGY
Condition
Definition
Bone cyst
Fluid-filled cyst with a wall of fibrous tissue
Congenital clubfoot
Abnormal twisting of the foot, usually inward and downward
Dislocation
Displacement of a bone from the joint space
Fracture
Disruption in the continuity of bone
Pott
Avulsion fracture of the medial malleolus with loss of the ankle mortise
Jones
Avulsion fracture of the base of the fifth metatarsal
Gout
Hereditary form of arthritis in which uric acid is deposited in joints
Metastases
Transfer of a cancerous lesion from one area to another
Osgood-Schlatter disease
Incomplete separation or avulsion of the tibial tuberosity
Osteoarthritis or degenerative joint disease
Form of arthritis marked by progressive cartilage deterioration in synovial joints and vertebrae
Osteomalacia or rickets
Softening of the bones owing to vitamin D deficiency
Osteomyelitis
Inflammation of bone owing to a pyogenic infection
Osteopetrosis
Increased density of atypically soft bone
Osteoporosis
Loss of bone density
Paget disease
Chronic metabolic disease of bone marked by weakened, deformed, and thickened bone that fractures easily
Tumor
New tissue growth where cell proliferation is uncontrolled
Chondrosarcoma
Malignant tumor arising from cartilage cells
Enchondroma
Benign tumor consisting of cartilage
Ewing sarcoma
Malignant tumor of bone arising in medullary tissue
Osteochondroma or exostosis
Benign bone tumor projection with a cartilaginous cap
Osteoclastoma or giant cell tumor
Lucent lesion in the metaphysis, usually at the distal femur
Osteoid osteoma
Benign lesion of cortical bone
Osteosarcoma
Malignant, primary tumor of bone with bone or cartilage formation
EXPOSURE TECHNIQUE CHART ESSENTIAL PROJECTIONS
Radiation Protection
Toes
PA PROJECTION