Chapter 10 Lumbar Transforaminal Epidural Steroid Injection, Supraneural (Traditional) Approach
Note: Please see page ii for a list of anatomical terms/abbreviations used in this book.
The transforaminal epidural steroid injection preferentially delivers injectate to the ventral epidural space.1,2 Optimally, the medication is placed at the suspected pathologic site that correlates anatomically with the patient’s clinical and radiographic presentation. Since the traditional supraneural transforaminal epidural steroid injection is performed for potentially therapeutic value, the medication should ideally spread medially around the pedicle to enter the epidural space with coverage of the exiting spinal nerve.
Other terminology has also been used to describe this procedure: spinal nerve root block, selective nerve root block, and segmental nerve root block. Although this terminology implies that the procedure has diagnostic value, recent literature has called the diagnostic value into question, as it is dependent on many factors.1,3–10
Historically, the transforaminal approach to epidural steroid injection was accomplished with a traditional supraneural (subpedicular) needle position. The technique described in this chapter differs from the subpedicular approach described in the ISIS guidelines.15 Instead, the needle is not advanced completely to the ventral aspect of the vertebral body, thus theoretically reducing the likelihood of vascular injection.
The “safe triangle” was described as a location where an injection could be accomplished with minimal risk of intrathecal or vascular injection and neural injury.12 Although complications are rare, conus infarct has been reported with this approach.13,14 It has been suggested that needle placement in the inferior aspect of the foramen (i.e., Kambin’s triangle) is a theoretically safer approach.13 The infraneural (i.e., retrodiscal or preganglionic) approach is presented in Chapter 11.
 Trajectory View
Trajectory View
 Confirm the level (see Chapter 1).
Confirm the level (see Chapter 1).
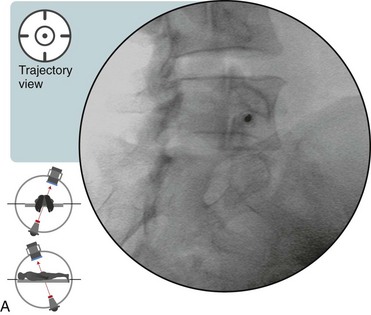
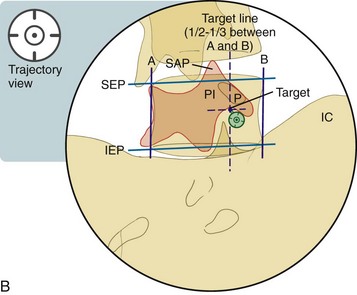
 Tilt the fluoroscope cephalad or caudad to line up the corresponding superior endplate (SEP). The SEP should appear as a straight line (Figure 10–1). Preferentially lining up the SEP rather than the IEP gives more of an inferior-to-superior needle trajectory (with the tip more likely to end up supraneural).
Tilt the fluoroscope cephalad or caudad to line up the corresponding superior endplate (SEP). The SEP should appear as a straight line (Figure 10–1). Preferentially lining up the SEP rather than the IEP gives more of an inferior-to-superior needle trajectory (with the tip more likely to end up supraneural).
 Line up the corresponding SEP.
Line up the corresponding SEP.
 Oblique the fluoroscope ipsilaterally to allow for the proper visualization of the “safe triangle” and therefore of the optimal trajectory for supraneural needle placement (see Figure 10–1).
Oblique the fluoroscope ipsilaterally to allow for the proper visualization of the “safe triangle” and therefore of the optimal trajectory for supraneural needle placement (see Figure 10–1).
 The target needle destination is just below the “chin” of the “Scotty dog” (i.e., adjacent to the pars interarticularis and inferior to the pedicle).
The target needle destination is just below the “chin” of the “Scotty dog” (i.e., adjacent to the pars interarticularis and inferior to the pedicle).
 The needle is placed approximately one half to one third of the distance between the vertical edges of the vertebral body (respectively, lines A and B in Figure 10–1B). It largely depends on whether the ISIS approach is followed, which is minimal oblique rotation based on the laminar border rather than movement to any set vertebral body position. This is to keep the needle from going too far medially and pithing the dural sheath. A more medial final needle tip placement requires a more oblique approach.
The needle is placed approximately one half to one third of the distance between the vertical edges of the vertebral body (respectively, lines A and B in Figure 10–1B). It largely depends on whether the ISIS approach is followed, which is minimal oblique rotation based on the laminar border rather than movement to any set vertebral body position. This is to keep the needle from going too far medially and pithing the dural sheath. A more medial final needle tip placement requires a more oblique approach.
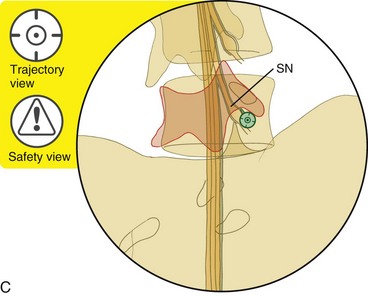
![]() Trajectory View Safety Consideration
Trajectory View Safety Consideration
Avoid the spinal nerve by staying in the superior one-sixth of the foramen.
 Identify a direct path to reach the target needle position.
Identify a direct path to reach the target needle position.
 Place the needle parallel to the fluoroscopic beam.
Place the needle parallel to the fluoroscopic beam.
![]() Notes on Positioning
Notes on Positioning
 A more oblique trajectory view results in a more medial final needle tip position. This approach may facilitate access to the neural foramen in individuals with foraminal stenosis.
A more oblique trajectory view results in a more medial final needle tip position. This approach may facilitate access to the neural foramen in individuals with foraminal stenosis. In the scoliotic spine, lining up the SEP may not result in an optimal needle trajectory. The needle trajectory may need to be further “tuned” by adjusting the tilt cephalad or caudad position. (See “Tuning” an Oblique View for Optimal Needle Trajectory page 29, Fig. 3–14A–C.)
In the scoliotic spine, lining up the SEP may not result in an optimal needle trajectory. The needle trajectory may need to be further “tuned” by adjusting the tilt cephalad or caudad position. (See “Tuning” an Oblique View for Optimal Needle Trajectory page 29, Fig. 3–14A–C.) For levels at and superior to L3, avoid the artery of Adamkiewicz (i.e., arteria radicularis magnus or ARM), which provides vascular supply to the conus medullaris.
For levels at and superior to L3, avoid the artery of Adamkiewicz (i.e., arteria radicularis magnus or ARM), which provides vascular supply to the conus medullaris.