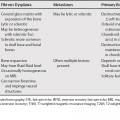
61 The only absolute contraindications to single lung transplantations are chronic pulmonary sepsis and uncorrectable cardiac defects. Table 61.1 provides an overview of the complications associated with lung transplantation. The spectrum of expression ranges from a mild, benign polyclonal proliferation of lymphatic tissue with few if any signs and symptoms to non-Hodgkin’s lymphoma. The incidence of post-transplant lymphoproliferative disorders (PTLD) after lung transplantation ranges from 6.2 to 9.4% and is twofold higher than what is seen after transplantation of other organs. Almost all cases of this disorder result from a combination of Epstein-Barr virus (EBV), stimulation of B-lymphocyte proliferation associated with a cyclosporin-inhibited regulatory mechanism of T-lymphocyte proliferation. A higher incidence of PTLD in children as compared with adults has been attributed to a greater susceptibility to EBV infection. A unique feature of this entity is that lymphoid masses may regress or disappear when immunosuppressive therapy is stopped or reduced. Intrathoracic PTLD is most commonly characterized by the presence of discrete nodules, more often multiple than solitary. The nodules are frequently distributed in peribronchovascular and subpleural locations involving the lower and middle lung zones. The intrathoracic computed tomography (CT) findings of PTLD are similar in immunocompromised patients with or without AIDS and are usually extranodal. Less frequently, mediastinal or hilar lymph node enlargement can be a manifestation of PTLD. Thymic, pericardial, and pleural involvement has also been reported.
Lung Transplantation
Indications
Single Lung Transplantations
Bilateral Lung Transplantations
Heart-Lung Transplantations
Complications
Lymphoproliferative Disorders
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree