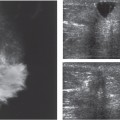
13 Lymph Nodes The preoperative awareness of lymph node metastases is essential for overall treatment planning. In the past, the surgical treatment of breast cancer was far more radical than today and generally included removal of the pectoralis major muscle and the level I–III lymph nodes. Removal of parasternal internal mammary nodes was not uncommon. Current opinion favors breast conservation where possible and in general, a less radical and more selective approach to treatment to reduce surgical morbidity and other side effects. With sentinel node imaging and more frequent utilization of gadolinium-enhanced breast MRI, the risk of leaving residual viable tumor in the breast or lymph nodes of patients has lessened. There is decreased likelihood also of apparent early recurrences within a year or two of initial surgical excision. Many such “recurrences” reflect continued activity of residual carcinoma left behind after removal of the index lesion. If sentinel node imaging is negative, in patients with no clinical evidence of level I axillary nodal involvement, many surgeons do not dissect the axilla at all. The internal mammary nodes are almost never exposed in the absence of compelling clinical concerns. This policy is questionable when we consider that the lymph nodes in the parasternal region are almost never palpable. Muscle fasciae are broadly attached to the sternum in this region, and enlarged lymph nodes deep in the intercostal spaces are virtually undetectable by physical examination. Because the fasciae create a firm boundary layer, nodal metastases in this region tend to expand inward between the ribs toward the pleura, causing indentation of the pleural cavity. As a result, these metastases remain clinically occult for a long time but can be seen with MRI or ultra-sound. In principle, a tumor located anywhere in the breast can seed malignant cells to lymph nodes in this region, but it is more likely to occur with tumors located in the medial breast. It should also be remembered that the lymphatic pathways can cross behind the sternum to the opposite side to form metastases in the contralateral breast and axilla. Although palpation of the axilla has been the traditional mainstay for clinical staging, studies have shown that preoperative detection of nodal metastases through physical examination is nonspecific. In approximately 40% of cases, metastatic lymphadenopathy is suspected clinically in the absence of histologic metastasis. Reports vary widely on the palpability of histologically confirmed metastases, but it is reasonable to assume that only approximately 50% of nodal metastases are palpable. Size is an unreliable predictor of malignancy: the sizes of normal and metastatic lymph nodes are highly variable. In one large series, an average diameter of 6.5 mm was determined for uninvolved lymph nodes and 9.7 mm for metastatic nodes, with a range from 1.8 to 40.6 mm. Thus, while larger lymph nodes tend to correlate with metastasis, even small lymph nodes a few millimeters in diameter may contain micrometastases defined as metastatic foci of diameters of 2 mm more or less. With regard to pathways of spread, it should be noted that laterally situated tumors are drained first by the level I axillary lymph nodes, located lateral to the pectoralis minor. From there drainage proceeds medially to the level II nodes (behind the pectoralis minor muscle) and level III nodes (infraclavicular nodes medial to the pectoralis minor). If nodal metastases have developed in this region, there is a high probability of spread to the supraclavicular space and the cervical nodes. It is also very likely that tumor cells have gained access to the bloodstream, leading to hematogenous metastasis. The sonographic features of normal lymph nodes are described in Chapter 4. The cortices of normal lymph nodes are isoechoic with the axillary fat and unless the node can be identified by its more echogenic hilar fat, axillary lymph nodes may not be conspicuous with ultrasound. Nodes that are palpable and have cortices wider than 2–3 mm on ultrasound can ordinarily be found sonographically. When the cortex of a node is widened uniformly, a benign, reactive type of adenopathy is the most common explanation. The histologic interpretation of these nodes when biopsied is often “sinus histiocytosis,” a reaction that can be encountered in association with breast cancers that have not metastasized. Benign reactive adenopathy also occurs in response to fibrocystic change, immune disorders, infections, and any process, such as recent biopsy, that activates the reticuloendothelial system, even if there is no clinically apparent cause. The reactive lymph node usually displays its central echogenic hilum, which marks the entry point of the vascular pedicle. This location of these vessels should be considered in color Doppler imaging, which is occasionally used for additional support if nodal metastasis is suspected. The afferent lymph vessels pass over the convex surface of the lymph node as they approach and enter it, and the efferent vessel exits the node at the central hilum. The echogenic hilum is surrounded by a zone of low echogenicity representing the sinuses and the corticomedullary lymphatic tissues. In reactive lymph nodes, the echogenic hilum is ordinarily symmetrically positioned in the center of the node and surrounded by a cortical zone of low echogenicity (Figs. 13.1a, b, 13.2; Table 13.1).
Clinical Significance
Diagnostic Criteria
Findings for Normal and Benign Lymph Nodes
Hilum | Central, hyperechoic |
Cortical zone | Hypoechoic rim of uniform width |
Findings for Malignant Lymph Nodes
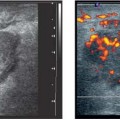
Advanced nodal metastasis is easily detected with ultrasound (Table 13.2). Once the hilum is invaded, the lymph node acquires a homogeneous, hypoechoic pattern (Fig. 13.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree