Clinical Presentation
The patient is a 65-year-old male who presented with low back pain (visual analog scale [VAS] = 6/10) and report of mild bilateral knee pain for the last 6 months. There are no radicular symptoms. Patient states that his pain decreases when he is standing and flexing forward at the waist. Pain is worse at night or any time he is recumbent. There are no constitutional symptoms. Complete blood count (CBC) is normal. Patient has no history of cancer.
Imaging Presentation
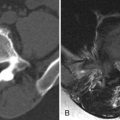
Imaging demonstrates a large soft tissue mass in the retroperitoneal space, anterior to the L2 and L3 vertebral bodies, which displaces the inferior vena cava anteriorly and laterally and encircles a portion of the aorta. There is no evidence of adjacent bone destruction. The findings represent a conglomerate of lymph nodes ( Fig. 45-1 ) .

Discussion
Lymph node evaluation is often performed with computed tomography (CT) or magnetic resonance imaging (MRI). Solitary retroperitoneal lymph nodes greater than 1.0 cm in long axis diameter or greater than 8 mm in short axis diameter are likely to be pathologic. If multiple lymph nodes between 0.8 and 1.0 cm in diameter are present, then adenopathy should be suspected. Pathologically enlarged lymph nodes can be caused primarily by lymphoma or may be metastatic resulting from a primary neoplasm. Pelvic retroperitoneal lymphadenopathy may be seen from spread of cervical, prostate, and bladder cancers. Testicular cancer can spread to the renal perihilar regions on the left and the paracaval region just inferior to the right renal vein. Colon, pancreatic, renal, lung, breast cancers, and melanoma frequently metastasize to the retroperitoneal lymph nodes. It can be difficult to differentiate metastatic lymphadenopathy from retroperitoneal lymphoma. The presence of lymph node necrosis favors metastatic disease.
Retroperitoneal lymphadenopathy can be a cause of back pain and extremity pain. Woll and Rankin demonstrated a series of patients who each suffered from severe back pain for several months that was interfering with their sleep. Lying flat was unbearable for these patients, and the only time the symptoms were lessened or relieved was when they were sitting forward. Retroperitoneal adenopathy was found in these cases, and it was not until these patients began their anticancer treatment with shrinkage of the lymph nodes that their pain subsided. Accordingly, any young patient with severe, persistent back pain that is relieved by sitting forward and without a history of trauma should be evaluated for malignant retroperitoneal lymphadenopathy. Smith and colleagues have had a similar experience in that new abdominal lymphadenopathy was discovered after patients with small cell bronchogenic carcinoma complained of new-onset back pain.
The etiology of lymphadenopathy-induced back pain is uncertain; however, it has been hypothesized that it may be due to direct neural compression or vascular compromise. Retroperitoneal metastatic adenopathy and lymphoma can affect the lumbosacral plexus. The lumbar plexus is formed from the anterior rami of the T12-L5 nerve roots and the sacral plexus is formed by the lumbosacral trunk and the anterior rami of the S1-S5 nerve roots. The lumbar plexus is formed within the psoas major muscle, anterior to the transverse processes of the L2-L5 vertebrae. The lumbosacral plexus can be affected by enlarged lymph nodes by extrinsic compression of the plexus causing low back pain and monoradicular or polyradicular symptoms.
Imaging Features
Ultrasound has been widely used in imaging lymph nodes; however, there are inherent limitations of the use of ultrasound secondary to the depth in evaluating retroperitoneal lymph nodes and therefore is not the imaging modality of choice. A normal lymph node is a somewhat oval-shaped, hypoechoic, usually hypovascular structure with varying amounts of hilar fat ( Fig. 45-2 ) . When a node is infiltrated with malignancy, the node becomes rounded and demonstrates peripheral or mixed vascularity ( Fig. 45-3 ) . Using these criteria, the accuracy of differentiating benign from malignant nodes is in the range of 84% to 94%.



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree