Lymphoproliferative Disorder
Jud W. Gurney, MD, FACR
Key Facts
Terminology
Lymphoproliferative disorders strongly related to either autoimmune diseases or immunosuppressed conditions
Follicular bronchiolitis
Small nodules and mediastinal lymphadenopathy common
Lymphocytic interstitial pneumonia (LIP)
Thin-walled cysts (80%), may be isolated finding
Nodular lymphomatoid hyperplasia
Air-space mass (consolidation with air-bronchograms)
Inflammatory myofibroblastic tumor
Solitary round to ovoid mass 1-12 cm in size
Mild homogeneous contrast enhancement
Castleman disease
Nodes may have intense enhancement (usually hyaline vascular form)
Angioimmunoblastic T-cell lymphoma (AILT)
Nodes may have avid contrast enhancement
Pleural effusion (40%)
Post-transplant lymphoproliferative disorder (PTLD)
Mediastinal adenopathy (50%), thymic involvement rare but relatively specific
Encompasses nonneoplastic and neoplastic lesions
Top Differential Diagnoses
Sarcoidosis
Hodgkin Lymphoma
Non-Hodgkin Lymphoma
Clinical Issues
Dysproteinemias clue to underlying lymphoid disorder
TERMINOLOGY
Definitions
Lymphoproliferative disorder (LPD)
Encompasses neoplastic and nonneoplastic lesions
May regress spontaneously or progress to malignant lymphoma
Strongly related to either autoimmune diseases or immunosuppressed conditions
Bronchus associated lymphoid tissue (BALT) extends from nodal clusters in airway bifurcations to lymphocyte cluster at proximity of lymphatics in respiratory bronchiole
BALT has extensive distribution, positioned to handle a large number of inhaled or circulating antigens
Polyclonal proliferation consistent with benign disease; monoclonal proliferation of lymphocytes consistent with lymphoma
Clonal groups determined by special stains
Specific LPD entities include
Follicular bronchiolitis
Lymphocytic interstitial pneumonia (LIP)
Nodular lymphomatoid hyperplasia (pseudolymphoma)
Inflammatory myofibroblastic tumor (plasma cell granuloma or inflammatory pseudotumor)
Castleman disease
Angioimmunoblastic T-cell lymphoma (AILT)
Post-transplant lymphoproliferative disorder (PTLD)
IMAGING FINDINGS
General Features
Best diagnostic clue
Abnormalities of lymphoid tissue from
Mediastinum: Enlarged mediastinal hilar lymph nodes
Lung: Thickening bronchovascular vessels, centrilobular nodules, septal thickening
LPD entities often focal and do not involve all lymphoid tissue
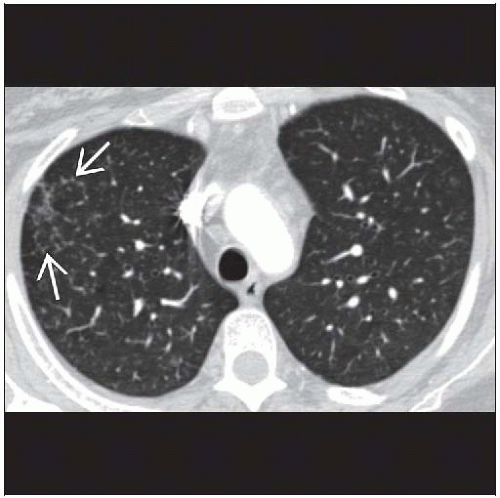
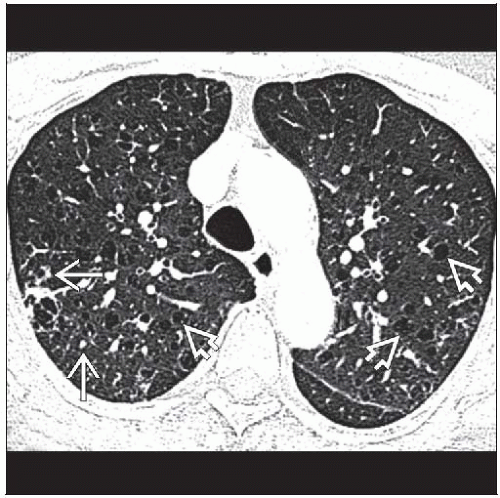
CT Findings
Mediastinal or hilar adenopathy
May involve 1 or more lymph node groups
Nodes may enhance and occasionally calcify
Focal lung disease
Nodule(s), mass, or focal consolidation
Margins usually indistinct, may have ground-glass halos
Cavitation and calcification uncommon
Usually located along bronchovascular bundles
Lymphoid tissue usually soft
Does not cause obstruction or infarcts
Air-bronchograms often persist (consolidated lung pattern)
Diffuse lung disease
Perilymphatic pattern: Accentuates normal course of lymphatic system
Thickening of bronchovascular bundles, interlobular septa, and centrilobular nodules
May lead to signs of bronchiolar injury
Tree-in-bud opacities, mosaic attenuation, centrilobular nodules, thin-walled cysts
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree