In pediatric patients, the high resolution and excellent soft-tissue contrast of magnetic resonance (MR) imaging allows for complete evaluation of osseous and soft-tissue structures around the knee joint, and its lack of ionizing radiation makes it a preferred modality for advanced imaging. Older children and adolescents are most commonly imaged to evaluate athletic and traumatic injuries, whereas in infants and school age children MR imaging is used to evaluate developmental conditions such as Blount disease or assess for causes of atraumatic pain such as infection or inflammatory arthritis. A thorough understanding of normal skeletal development is necessary to avoid misdiagnoses.
Key points
- •
Marrow conversion begins in the epiphyses 6 months after the radiographic appearance of the secondary ossification center. Transition to fatty marrow then continues from the mid-diaphysis toward the metaphyses.
- •
Irregular ossification involving the posterior femoral condyle epiphysis should be considered normal variation rather than an osteochondral lesion (OCD) in the absence of overlying cartilage abnormality and underlying bone marrow edema.
- •
Unlike adults who are more likely to suffer from ligamentous and meniscal injuries, trauma in pediatric patients characteristically involves the physis and adjacent bones.
- •
In contrast to adult OCDs, the hyperintense signal between the osteochondral fragment and native bone must mirror joint fluid to suggest instability in children.
- •
Synovial sarcoma is the most underrecognized malignant tumor that commonly occurs about the knee; lack of recognition is due to its seemingly benign magnetic resonance imaging characteristics.
Introduction
In pediatric patients, the knee is the most common joint to be assessed with magnetic resonance (MR) imaging. MR imaging of the knee is performed in children and adolescents to evaluate various traumatic, inflammatory, developmental, and neoplastic conditions. Its high resolution and excellent soft-tissue contrast allow for complete evaluation of both osseous and soft-tissue structures around the knee joint, and its lack of ionizing radiation makes it a preferred modality for advanced imaging in children. At younger ages, sedation is often necessary to obtain diagnostic images, presenting risks that must be taken into account when deciding on the necessity of the study. Furthermore, one must have a solid understanding of the normal skeletal development and variations in development of the distal femur, proximal tibia, and proximal fibula to avoid misdiagnoses.
Older children and adolescents are most commonly imaged to evaluate athletic and traumatic injuries. From infancy through school age, however, MR imaging is more often performed to evaluate developmental conditions such as Blount disease or to assess for causes of atraumatic pain such as infection or inflammatory arthritis. Neoplasms, both benign and malignant, commonly occur about the knee throughout childhood. Only the most common benign tumors and the most underdiagnosed malignancy are discussed in this article.
Introduction
In pediatric patients, the knee is the most common joint to be assessed with magnetic resonance (MR) imaging. MR imaging of the knee is performed in children and adolescents to evaluate various traumatic, inflammatory, developmental, and neoplastic conditions. Its high resolution and excellent soft-tissue contrast allow for complete evaluation of both osseous and soft-tissue structures around the knee joint, and its lack of ionizing radiation makes it a preferred modality for advanced imaging in children. At younger ages, sedation is often necessary to obtain diagnostic images, presenting risks that must be taken into account when deciding on the necessity of the study. Furthermore, one must have a solid understanding of the normal skeletal development and variations in development of the distal femur, proximal tibia, and proximal fibula to avoid misdiagnoses.
Older children and adolescents are most commonly imaged to evaluate athletic and traumatic injuries. From infancy through school age, however, MR imaging is more often performed to evaluate developmental conditions such as Blount disease or to assess for causes of atraumatic pain such as infection or inflammatory arthritis. Neoplasms, both benign and malignant, commonly occur about the knee throughout childhood. Only the most common benign tumors and the most underdiagnosed malignancy are discussed in this article.
Normal skeletal maturation
To appropriately interpret pediatric musculoskeletal images, one must be aware of normal changes that occur with skeletal maturation. The epiphyses at both ends of tubular bones are positioned between the primary physis (growth plate) and the joint. Initially, the epiphysis is entirely cartilaginous. The secondary ossification center forms through endochondral ossification, beginning at the center of the epiphysis. Whereas the primary physis is responsible for longitudinal growth of the bone at each metaphysis, the secondary physis surrounding the secondary ossification center is responsible for spherical growth.
The normal sequence of marrow conversion in pediatric patients must be understood, so as not to delay the diagnosis of infiltrative malignancy, such as leukemia, when imaging children who present with vague joint pain, swelling, or even pathologic fracture. At birth the marrow is entirely hematopoietic, resulting in relatively low signal intensity that is similar to or slightly higher than that of skeletal muscle on T1-weighted images. Normal marrow is usually higher in signal intensity than marrow infiltrated by disease. On T2-weighted images, hematopoietic marrow shows high signal intensity which is less than that of simple fluid and similar to that of muscle. Therefore, very low signal intensity marrow on T1-weighted images and increased signal intensity on water-sensitive sequences is concerning for malignancy.
During the first year of life, conversion from hematopoietic to fatty marrow begins. This marrow conversion progresses from the periphery to the center of each bone in the appendicular skeleton. Epiphyseal conversion occurs first, within 6 months of the radiologic appearance of the secondary ossification center. Transition to fatty marrow then continues, beginning at the mid-diaphysis and progressing toward the metaphyses. Hematopoietic marrow can be seen into early adulthood within the proximal metaphyses of the femora and humeri, as these are the last sites to convert. The transition back to red marrow in patients with anemia or who are receiving growth factors occurs in the reverse order, extending from the metaphyses centrally to the diaphysis before conversion in the epiphyses occurs. Residual hematopoietic marrow about the knee will appear flame-shaped, with a base adjacent to the physis.
The periosteum is a thin, linear, hypointense structure paralleling the bone. It is tightly bound at the level of the physis but loosely attached along the shaft of the bone. Blood, pus, or tumor easily elevates the periosteum. In children, a layer of fibrovascular tissue separates the periosteum, resolving after physeal closure. This feature is most evident in long bones at the level of the metaphysis, and is best seen along the posterior distal femoral metaphysis as high signal intensity on water-sensitive sequences with intense contrast enhancement ( Fig. 1 ). This “metaphyseal stripe” should not be mistaken for a subperiosteal fluid collection.
Normal signal characteristics of the physeal structures on T2-weighted images vary. From distal to proximal, the cartilage of the primary physis (growth plate) is hyperintense, with the adjacent zone of provisional calcification appearing as a thin hypointense line. Immediately proximal resides the primary spongiosa of the metaphysis, which is hyperintense because of its vascularity. The hyaline cartilage of the unossified epiphysis appears hypointense compared with the overlying articular cartilage. During early ossification, increased signal within the distal femoral epiphyseal cartilage may occur, ranging from patchy to focal. The signal intensity along the weight-bearing surface of the distal femoral epiphyseal cartilage, however, is decreased, presumably because of water loss (see Fig. 1 ). Contrast administration shows vascular channels radiating peripherally through the epiphyseal cartilage, which will appear more prominent in diseases such as inflammatory arthritis in which the synovium is hyperemic.
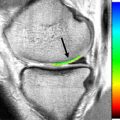
Focal bone marrow edema centered at the physis can be seen in the central distal femur ( Fig. 2 ), proximal tibia, or proximal fibula of adolescents, termed focal periphyseal edema pattern (FOPE). All reported patients with FOPE have unfused but narrowed physes. Because this periphyseal edema pattern is seen in patients presenting with pain and incidentally in asymptomatic patients, it is postulated that this may represent normal signal changes related to physeal fusion. Areas of fused physis have relatively less flexibility, possibly resulting in localized microtrauma, accounting for the pain that some patients experience.
Variation in epiphyseal ossification and signal intensity is most evident along the distal femoral condyles. The development of low signal intensity along the weight-bearing surface of the epiphyseal cartilage begins as soon as the child becomes ambulatory. During the preschool years (ages 3–5 years), increasing signal intensity develops in the posterior condylar cartilage and is initially poorly defined, occurring before radiographically identifiable calcification. This increase in signal intensity becomes more focal as the child grows, and appears radiographically as single or multiple ossification centers that eventually coalesce with the underlying bone. Gebarski and Hernandez have described 4 different normal variations in ossification of the posterior femoral condyles. The first they describe as a puzzle-piece configuration whereby an osseous defect in the posterior femoral condyle is filled with an ossification that fills the defect. The second is an incomplete puzzle-piece configuration whereby the ossification does not completely fill the defect. The posterior condyle can also have a spiculated appearance ( Fig. 3 ) or have many adjacent small ossifications (see Fig. 3 ; Fig. 4 ). Unlike OCD lesions, there is no bone marrow edema seen with any of these variants to suggest abnormality. In addition, these normal variants reside more posteriorly along the non–weight-bearing surface of the femoral condyle. In the absence of adjacent bone marrow edema, these developmental variations should not be mistaken for osteochondritis dissecans.
Trauma
Unlike adults who are more likely to suffer from ligamentous and meniscal injuries, trauma in children and adolescents characteristically involves the physis and adjacent bones, which are the weakest link in skeletally immature patients. Thus the pediatric knee is susceptible to multiple types of fractures in addition to chronic repetitive stress injuries. There are various acute and chronic knee injuries unique to the growing pediatric patient. As increasingly more children are involved in competitive sports at a younger age, these injuries are becoming more prevalent. The most common indications for MR imaging of the knee following trauma are refusal to bear weight, persistent pain, or hemarthrosis in the presence of negative radiographs, suggesting internal derangement or occult fracture.
Acute
Ligamentous injuries are overall less common in pediatric patients than in adults, owing to ligamentous laxity in combination with relative weakness of the physis; as such, osseous injuries are more common. The most common ligament injured in the pediatric population is the anterior cruciate ligament (ACL). ACL tears are more common in girls, likely related to a combination of hormonal influence, valgus alignment, and increased joint laxity. MR criteria for the diagnosis of ACL tear is the same as that in adults, with loss of parallelism with the Blumensaat line being a more sensitive finding than fiber discontinuity in this age group. Unlike adults, the classic pattern of bone marrow edema involving the lateral femoral condyle and posterolateral tibial plateau (“kissing contusions”) is not always associated with an ACL tear in pediatric patients, owing to normal ligamentous laxity.
In even younger patients, the same mechanism of injury produces tibial spine avulsion fractures rather than ACL tears, especially if the intercondylar notch is wide. Type I tibial spine avulsion fractures are, at most, minimally displaced and are managed conservatively. The remaining types require surgical intervention. Type II fractures show anterior elevation from the parent bone. Type III and IV fractures show progressive separation of the fragment ( Fig. 5 ). Type V fractures are displaced and have a rotational component. Hinged or displaced avulsion fractures require surgery. Posterior cruciate and collateral ligament injuries are uncommon, as severe valgus or varus stress on the knee joint more likely result in physeal fracture.
Before physeal fusion occurs, meniscal injury is uncommon. Meniscal tears in pediatric patients appear similar to those in adults: linear increased signal within the meniscus extending to the articular surface, abnormal morphology, or displaced meniscal fragments. Longitudinal tears and peripheral detachments are the most common, with the posterior horns more often injured. Normal vascular tissue can produce increased signal within the meniscus, but differs from a tear in that the increased signal intensity does not extend to the articular surface. Most meniscal injuries in children younger than 10 years are due to discoid meniscus (see later discussion).
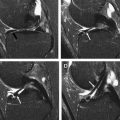
Fractures involving the distal femoral or proximal tibial physes are considered high risk for causing abnormal growth ( Figs. 6–9 ). These Salter-Harris fractures can be subtle on radiographs, and often require subsequent MR imaging to further define the extent of the fracture and associated soft-tissue injuries. Metaphyseal fractures in the distal femur or proximal tibia appear as linear foci of high signal intensity with surrounding marrow edema on fluid-sensitive sequences. The injured portion of the adjacent physis shows high signal intensity and widening. Periosteal elevation and disruption are commonly seen adjacent to the injured physis. Periosteum may even become trapped within the fracture. Associated effusions, predominantly suprapatellar, are common. Salter-Harris type II fractures of the distal femur are the most common type diagnosed on MR imaging. Follow-up imaging may be indicated to evaluate for premature physeal fusion, either with radiographs, computed tomography, or MR imaging.
Acute extensor mechanism injuries include transient patellar dislocation (TPD), patellar sleeve fractures, and tibial tubercle avulsion fractures. TPD usually occurs between the ages of 14 and 16 years during a twisting injury of the mildly flexed knee with the foot planted, resulting in the quadriceps muscle pulling the patella laterally. During lateral dislocation, the inferomedial patellar facet impacts the trochlear articular surface, resulting in osteochondral defects in both the inferomedial patella and lateral trochlea. Of note, the patellar lesion should be seen on at least 2 consecutive images. As the patella relocates during leg extension, it impacts the anterolateral femoral condyle, resulting in the characteristic bone contusions of the medial patella and anterolateral femoral condyle. The femoral contusion is located just anterior to the trochlear osteochondral lesion, more anterior and superior to those seen in older adolescents and adults with ACL injury.
It is also imperative to evaluate the images for evidence of medial patellar restraint injury. Both the medial patellar retinaculum (MPR) and the medial patellofemoral ligament (MPFL) require scrutiny. Previously, disruption of the MPR at its patellar insertion was thought to be of greatest importance. More recent studies, however, have demonstrated that the MPFL is the major ligament limiting lateral patellar movement. The vastus medialis obliquus muscle (VMO) also plays an important role, as it acts as a dynamic stabilizer, counteracting the pull of the vastus lateralis muscle. The MPFL provides 50% to 80% of the medial restraint of the patella ; therefore, injury to this structure often results in persistent instability. The MPFL travels anteriorly from the region of the adductor tubercle on the medial femoral condyle deep to the VMO to attach to the superomedial patella. MPFL tears are common after TPD and usually occur at its femoral attachment. As this structure is difficult to discretely identify, the secondary signs of substantial edema at its origin near the adductor tubercle and elevation of the VMO by edema are used to diagnose a tear. Edema may also be seen on occasion in the adductor tubercle itself. The medial retinaculum is seen as a low signal intensity band extending posteriorly from the medial patella and becoming continuous with the fascia of the VMO. The medial retinaculum may be torn at its patellar attachment, possibly with an associated cortical avulsion fragment, or along its mid-substance. T2 hyperintense edema adjacent the medial patellar pole indicates retinacular injury. Wrinkling of the MPR indicates a tear. Additional MR findings in patients with TPD include joint effusion, hemarthrosis, lateral patellar subluxation or tilt, patella alta, and trochlear dysplasia.
Predisposing factors for TPD include genu valgum, ligamentous laxity, trochlear dysplasia, patellar tilt, patella alta, and a dysplastic, flattened patella. Trochlear dysplasia can be diagnosed when the trochlear line lies anterior to the lateral femoral condyle on a well-positioned lateral radiograph (the trochlear crossover sign). On a mid-sagittal MR image, a sharp, step-like transition from the anterior femoral cortex to the trochlear articular surface is seen rather than a smooth one. Trochlear depth can be evaluated on an axial image 3 cm above the weight-bearing surface of the condyles. If the depth measures 3 to 5 mm or less, the trochlea can be called shallow and is associated with patellar instability.
Patellar sleeve avulsion fractures are osteocartilaginous injuries at the inferior patellar pole ( Fig. 10 ) and occur most commonly between the ages of 8 and 12 years. Cartilage surrounding the ossifying patella blends directly with patellar tendon fibers rather than by distinct Sharpey fibers that are found in adults. For this reason, patellar tendon injury in children occurs at the proximal or distal ends of the tendon, rather than at the mid-substance. MR imaging helps distinguish between this entity and Sinding-Larsen-Johansson (SLJ) syndrome following episodes of trauma, as radiographs will show bone fragments adjacent to the inferior patellar pole in both entities. With patellar sleeve avulsion fracture, the fragment includes both bone and apophyseal cartilage. The extent of the cartilaginous injury is often significantly underestimated on radiographs. This aspect has clinical implications, as SLJ is managed symptomatically, whereas patellar sleeve avulsion fractures require open reduction and internal fixation for displaced fractures or at least immobilization and non–weight-bearing if nondisplaced.