The magnetic resonance (MR) imaging presentations of arthritis of the knee are important for radiologists to recognize because these disorders are often clinically unsuspected. When they are known or clinically suspected, knowledge of imaging features allows for the confirmation and characterization of the extent of disease. This article reviews the fundamental MR imaging manifestations of rheumatologic disorders of the knee and their presentation in specific arthropathies.
Key points
- •
Synovitis is a nonspecific finding that may be confused with effusion.
- •
Erosions in the knee occur in tight recesses. Multiple ill-defined erosions are an indication of an aggressive arthropathy.
- •
Enthesitis may be an indication of a seronegative spondyloarthropathy.
- •
Correlation with radiography is important for evaluation of low T2-signal intra-articular or periarticular processes.
- •
Accurate diagnosis of an arthropathy on magnetic resonance imaging is possible when imaging findings are correlated with distribution of disease and clinical presentation.
Introduction
Radiologists must be able to recognize and characterize the magnetic resonance (MR) imaging manifestations of arthropathies of the knee regardless of whether the diagnosis is known, suspected, or unsuspected, because arthropathies are an important source of knee pain. In some instances, the referring clinician may presume internal derangement as the cause of joint symptoms and not be aware of an underlying arthritis, in which case the radiologist can provide a helpful differential diagnosis. In other situations, the diagnosis of arthritis is suspected or known and the radiologist’s role changes from suggesting a diagnosis to defining the extent of disease. The purpose of this article is to discuss the general MR imaging manifestations of arthritis in the knee and to review their presentation in specific diseases.
Introduction
Radiologists must be able to recognize and characterize the magnetic resonance (MR) imaging manifestations of arthropathies of the knee regardless of whether the diagnosis is known, suspected, or unsuspected, because arthropathies are an important source of knee pain. In some instances, the referring clinician may presume internal derangement as the cause of joint symptoms and not be aware of an underlying arthritis, in which case the radiologist can provide a helpful differential diagnosis. In other situations, the diagnosis of arthritis is suspected or known and the radiologist’s role changes from suggesting a diagnosis to defining the extent of disease. The purpose of this article is to discuss the general MR imaging manifestations of arthritis in the knee and to review their presentation in specific diseases.
Basic principles
The key presentation of arthritis, both clinically and radiologically, is that the disease is centered on the joint and typically involves both sides of it. Arthritis can solely involve the synovium, ligaments, tendons, cartilage, or bone of an involved joint, but more commonly the disease affects multiple components of the joint. The character of the involvement of these structures not only permits the gross characterization of an arthropathy but also may lead to a specific diagnosis.
Synovium/Synovitis
The synovium is the lining of the joint and is normally only a few cell layers thick. Therefore, the synovium should not be visible in the normal patient. Inflammation leads to thickening of the synovium at histology and on imaging. The diseased synovium is leaky, and effusion commonly accompanies synovitis. Synovitis is a nonspecific finding that can be seen in many arthropathies including inflammatory, crystal-induced, septic, and degenerative etiology. The radiologist needs to recognize the MR imaging manifestations of synovitis and characterize both its imaging features and extent, because the presence of synovitis commonly correlates with pain.
Synovitis may manifest diffusely, focally, or in a mass-like pattern in any location in the knee joint. Diffuse inflammatory synovitis is most commonly recognized in the posterior aspect of the knee (posterior cruciate ligament recess), The Hoffa fat pad, and the suprapatellar bursa. On T1-weighted images, inflammatory synovitis may be visualized as thickening of the joint capsule that can be differentiated from the lower signal of adjacent joint fluid ( Fig. 1 ). Inflammatory synovitis is typically high in signal on fluid-sensitive sequences. Sometimes in more advanced stages, one can manipulate window and level on a PACS (Picture Archiving and Communication System) workstation to recognize synovitis as fronds that have lower signal than adjacent high-signal effusion on fat-suppressed proton-density or T2-weighted sequences ( Fig. 2 ). Noncontrast depiction of the extent of synovitis in a joint can be improved with diffusion-weighted imaging. However, the true extent of synovitis is characterized best with intravenous gadolinium. Normal synovium enhances, but this enhancement should not be visible to the naked eye. Active synovitis enhances rapidly, and the extent of inflammation can be characterized on dynamic contrast-enhanced sequences. The true extent of synovitis should be assessed within 10 minutes following the administration of intravenous contrast, because rapid diffusion of gadolinium into the adjacent effusion may preclude distinction of synovitis adjacent to the effusion later.
The signal characteristics of the thickened synovium also should be assessed for patterns that deviate from the typical intermediate T1 and high T2 signal of acute synovitis. Synovitis that is low in signal on T2-weighted images is usually an indication of either increased collagen in chronic synovitis or hemosiderin in the synovium in entities such as pigmented villonodular synovitis (PVNS) or chronic hemorrhage in the joint from a coagulopathy (eg, hemophilia) ( Fig. 3 ). Hemosiderin is the most likely cause of low T2-signal synovitis if blooming artifact is appreciated on a gradient-echo sequence. Amyloid should also be considered in the differential diagnosis of low T2-signal synovitis. It is very important to review a radiograph to ensure that calcification is not the source of low T2 signal.
Chronic synovitis also may demonstrate fat signal pattern (high T1 and low on fat-suppressed sequence). Fatty replacement of the synovitis is reported as lipoma arborescens ( Fig. 4 ). This nonspecific pattern of chronic synovitis is most commonly seen in the setting of osteoarthritis (OA), but can also be seen in patients with burned-out inflammatory arthritis.
Bone Manifestations
Arthropathies may affect the osseous components of an involved articulation. Osseous manifestations of arthritis may include erosions, bone marrow edema–like lesions, subchondral cysts, and osteonecrosis.
Erosion is a relatively uncommon manifestation of an arthropathy in the knee because of the capacious nature of this joint. Acute erosions are usually a manifestation of an aggressive inflammatory arthritis such as septic arthritis, rheumatoid arthritis (RA), or reactive arthritis. Acute erosions have ill-defined margins and are seen adjacent to tight spaces in the joint such as the meniscal recesses, on the articular surfaces, or superior to the posterior condyles ( Fig. 5 ). The cortical disruption and replacement of adjacent normal fat marrow is best recognized on T1-weighted images. Increased T2 signal on fat-suppressed images in the marrow adjacent to an erosion is an indication of an aggressive process.
Chronic erosions that are well corticated suggest a slowly progressive process such as gout, PVNS, synovial chondromatosis, or amyloidosis. Chronic erosions also usually are appreciated in the tight recesses of the joint rather than adjacent to the suprapatellar bursa.
Bone marrow edema–like lesions may be seen in the inflammatory arthropathies or OA. In the setting of OA, bone marrow edema–like lesions correlate with pain in most patients, and may be an indication of remodeling of subchondral bone in response to abnormal mechanics. Subchondral cysts are also a nonspecific finding that can be appreciated in many arthropathies. Their development can be due to direct erosion or be a reparative response to subchondral microfracture.
Bone infarction or osteonecrosis can be a secondary manifestation resulting from steroid therapy. Systemic lupus erythematosus should be considered in the setting of suspected rheumatologic disease, particularly when the infarcts are multiple and there is no history of steroid administration.
Tendons and Ligaments
Careful evaluation of the tendons and ligaments is important in the setting of atraumatic knee pain. Diffuse or mass-like infiltration of a tendon or ligament of the knee may be an indication of crystal deposition disease such as gout, hydroxyapatite deposition disease (HADD), or, less commonly, calcium pyrophosphate deposition disease. The signal characteristics of crystal deposition disease are variable (see later more detailed discussion).
Enthesopathic changes at the attachment of ligaments and tendons to bone are classically associated with a seronegative spondyloarthropathy such as reactive arthritis or psoriatic arthritis (PsA). Increased T2 signal in the bone at the site of attachment of the tendon or ligament is an indication of enthesitis.
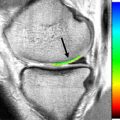
Cartilage
Loss of articular cartilage is a nonspecific indicator of an arthropathy. The articular cartilage of the knee is adequately evaluated in most cases on a fat-suppressed fast spin-echo proton-density sequence or steady-state gradient-echo sequence. Diffuse loss of articular cartilage is usually an indication of an inflammatory arthritis. Focal loss of articular cartilage is most commonly an indication of OA.
MR imaging manifestations in specific arthropathies
Arthritis can be subdivided into major categories: inflammatory, deposition disease, OA, neuropathic, collagen vascular disease, and mass-like arthropathies. The MR imaging findings associated with specific arthropathies are discussed, but MR imaging features of neuropathic and collagen vascular disease involving the knee are not covered in this article.
Inflammatory Arthropathies
Inflammatory arthropathy includes septic arthritis, RA, PsA, and reactive arthritis. Much research has been directed at identification of MR imaging features that can differentiate septic from other inflammatory arthritides. Many of the findings have demonstrated too much overlap to allow a specific diagnosis by imaging alone. Both infectious and noninfectious joint inflammation results in the development of varying degrees of joint effusion, pericapsular edema, synovial hypertrophy, and enhancement, all of which can lead to the development of marginal erosions and cartilage loss. The features that may help to narrow the differential diagnosis and direct further diagnostic evaluation are covered in this section. The number of joints involved, distribution of disease, and clinical features of the disease presentation are all crucial factors in arriving at a correct diagnosis.
Septic arthritis
Septic arthritis of the knee presents with one of two primary clinical pictures. With pyogenic organisms a swollen, red, painful joint develops within days of inoculation. In nonpyogenic infections, the presentation may be more indolent with swelling and pain occurring over the course of weeks to months. Though septic arthritis must be excluded in any monoarticular arthropathy, 2 or more joints are involved simultaneously in up to 19% of cases. This oligoarticular involvement, especially in nonpyogenic infections, can result in confusion of the diagnosis with inflammatory arthritis. The classic clinical and laboratory features of septic arthritis, which include fever, rigors, increased systemic white blood cell count, and elevated sedimentation rate, are each only present in about one-half to two-thirds of patients. The appropriate initial imaging study is conventional radiography. However, radiographs are often normal or show only nonspecific joint effusion and symmetric soft tissue swelling in the early phase of disease. Even joint effusion may be absent in as many as one-third of infected joints. As such, a lack of joint effusion should not be used to exclude septic arthritis. Joint aspiration remains the primary means of diagnosis of septic arthritis. The most important predictor of morbidity is the time from symptom development to initiation of treatment, with improved outcomes when treatment is initiated in the first 7 days.
MR imaging is a sensitive means of additional evaluation of the joint and surrounding soft tissues when the diagnosis is unable to be established through aspiration or when complicating features are of concern. The most helpful imaging sequences include T1-weighted and fat-suppressed T2-weighted imaging, or short-tau inversion recovery (STIR) imaging followed by fat-suppressed T1-weighted imaging after intravenous gadolinium administration.
Pyogenic septic arthritides
Fifty percent of cases of septic arthritis of the knee are bacterial. Most bacterial cases of septic arthritis are the result of a single organism, with Staphylococcus aureus the causative organism in 50% to 80% of cases across all age groups. Intravenous drug use, the presence of indwelling catheters, and underlying immunocompromised states in addition to preexisting joint arthropathy, such as RA, serve as predisposing factors for the development of a septic arthritis. Beyond S aureus , a variety of organisms should be considered, based on patient age and clinical scenario ( Table 1 ), some of which have special culture requirements or lower diagnostic yields on synovial fluid evaluation.
| Patient Population | Organisms |
|---|---|
| Children <2 y old | Kingella kingae , Haemophilus influenzae , group A Streptococcus |
| Young adult | Neisseria gonorrhoeae , Streptococcus |
| Infectious diarrhea | Shigella , Salmonella , Campylobacter , Yersinia |
| Human immunodeficiency virus | Streptococcus pneumoniae , Mycobacterium , fungal |
| Joint prosthesis in place >3 mo | Streptococcus , gram-negative aerobes, anaerobic infections |
On MR imaging, bone erosions, cartilage loss, bone marrow edema, and erosion enhancement are more often seen in the setting of bacterial infection ( Fig. 6 ). Development of adjacent osteomyelitis may be difficult to exclude on MR imaging. Most cases progressing to osteomyelitis demonstrate diffuse marrow edema on T2-weighted imaging adjacent to the septic joint, but this finding can also present in one-third of cases of septic arthritis without osteomyelitis. Although abnormal intermediate T1 signal increases specificity, normal T1 marrow signal does not exclude osteomyelitis.
Nonpyogenic arthritides
Lyme arthritis
Lyme disease is the result of the tick-transmitted infection with the spirochete Borrelia burgdorferi . The disease has been reported throughout the United States but with the highest incidence in the mid-Atlantic and northeast states during the spring and summer months. Up to half of individuals will manifest the pathognomonic erythema chronicum migrans rash within days to a month from the time of the tick bite. Left untreated, carditis, neurologic symptoms, and an oligoarthritis may develop within weeks to years. The knee is involved in Lyme arthritis in 80% of patients. Massive recurrent joint effusions are a classic presentation, with few patients progressing to chronic synovitis. The massive joint effusions may be associated with large popliteal cysts. Progression from marginal erosions to uniform cartilage loss from all compartments can occur. Enthesitis at the patella attachments of the quadriceps and patella tendons also has been described occasionally, and is conjectured to be related to traction as a result of recurrent massive joint effusions.
MR imaging features that have been reported more frequently in Lyme arthritis than in other arthritides are the presence of popliteal fossa lymphadenopathy and popliteus muscle myositis ( Fig. 7 ). Pericapsular soft-tissue edema is reported as occurring less commonly in Lyme arthritis than in other infections. Serologic tests or polymerase chain reaction of synovial fluid can be confirmatory, and treatment with oral or intravenous antibiotics is curative in most cases.
Tuberculous arthritis
The musculoskeletal system is involved in 1% to 3% of patients with extrapulmonary Mycobacterium tuberculosis (TB), most cases involving the spine. The hip and knee joints are the 2 most common sites for extraspinal musculoskeletal infection with TB. The clinical presentation is often indolent and nonspecific, and may mimic an inflammatory arthritis such as rheumatoid or juvenile inflammatory arthritis. A history of travel to endemic areas should be sought. Although the diagnosis of tuberculous arthritis is not possible based solely on the clinical or imaging findings, there are features that may suggest the diagnosis. The classic radiographic findings (Phemister’s triad) of juxta-articular osteoporosis, marginal erosions, and gradual joint space loss may be seen radiographically. At MR imaging, in addition to the nonspecific findings of synovial thickening, perisynovial edema, joint effusion, and marginal erosions, fibrinoid “rice bodies,” similar to what may be seen in RA, may be encountered. The synovitis present may also demonstrate a relatively low T2 signal, which may help suggest TB arthritis. Periarticular “cold abscesses” presenting as soft-tissue fluid collections or fluid extensions from the joint may be seen, with an appearance similar to that of synovial cysts encountered in RA. Over time, these collections may form marginally enhancing draining sinus tracts to the skin surface, which is not a common development in synovial cysts in other inflammatory arthropathies.
Rheumatoid arthritis
RA is a chronic systemic inflammatory disorder producing synovitis and cartilage destruction. Since the advent of disease-modifying antirheumatic drugs (DMARDs), early diagnosis and initiation of treatment, before radiographically evident erosive changes, has demonstrated a significant impact on slowing disease progression and the long-term disability associated with RA. Though classically a bilateral symmetric polyarthropathy with wrist or metacarpal phalangeal joint involvement, RA also frequently involves the knees and may serve as an initial site of involvement in 13% of patients. Involvement of a single joint may occur for weeks to months before presentation of classic polyarticular involvement. As in septic arthritides, during flares of acute inflammation elevation of nonspecific inflammatory serum markers (C-reactive protein, erythrocyte sedimentation rate) can occur. Seropositivity for rheumatoid factor (RF) is seen in 70% to 80% of cases.
MR imaging not only permits early identification of synovitis but also allows for reproducible quantification of the synovitis that is a strong predictor for the development of future erosions. MR imaging has also demonstrated usefulness in assessing the response to therapy or reactivation of disease. Postcontrast imaging most accurately demonstrates the extent of synovitis ( Fig. 8 ). Dynamic gadolinium enhancement in an early phase (30–60 seconds) has been shown to accurately correlate with active synovial inflammation. When not performing dynamic gadolinium imaging, images should be acquired within 10 minutes of gadolinium injection because contrast will diffuse into the joint fluid, thus limiting the reliable distinction of synovium from effusion.
Besides the common features of infectious or inflammatory arthropathies already described, additional features that may suggest RA include the following. (1) Rice bodies consist of sloughed fibrinous material and necrotic debris. These rod-shaped (1–3 mm) intermediate T1 and T2 signal bodies may be seen in the joints or involved bursae. Though also seen in tuberculous arthritis, rice bodies are most frequently encountered in RA and are less common in other inflammatory arthritides ( Fig. 9 ). (2) Synovial cysts are synovial lined fluid collections that may have long extensions from the joint into the adjacent soft tissues. About the knee, these most commonly originate from popliteal Baker cyst. Synovial cysts may also gain access to the medullary cavity of the bones through erosions and create lytic, endosteal eroding lesions that will image as low T1, high T2 central fluid signal with peripheral rim enhancement, as would be expected of a cyst. The cysts are not specific and may develop with any long-standing large joint effusion, but in the setting of a polyarthropathy are most common in RA. (3) Low T2-signal synovitis. Most inflammatory synovitis demonstrates low to intermediate T1 and intermediate to increased T2 signal. Chronic RA may result in fibrosis within the pannus that shows low signal on both T1 and T2 imaging.
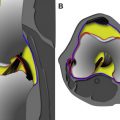
Seronegative arthropathies
Psoriatic and reactive arthritis
PsA is an HLA B27–associated arthropathy that has several diverse clinical presentations. The most common (70%) is that of an asymmetric oligoarthritis that frequently includes involvement of the knee. Approximately 5% to 8% of patients with psoriatic skin changes will develop PsA, at a mean age of diagnosis of 40 years. Conversely, at the time of PsA development, most patients will have dermatologic findings of psoriasis, although in 15% arthritis will precede visible skin changes. Similar to other inflammatory arthropathies, PsA produces synovitis, marginal erosions, and often pericapsular inflammatory changes.
Reactive arthritis (formerly Reiter syndrome) is an HLA B27–associated autoimmune inflammatory arthropathy that is triggered by a genitourinary or gastrointestinal infection. The result is a triad of clinical symptoms that includes (1) arthropathy, in association with (2) urethritis and (3) conjunctivitis or uveitis. Joint involvement is typically an oligoarthropathy that is more common in the lower extremities.
On MR imaging, the seronegative arthropathies may demonstrate synovitis and erosions, beginning marginally, with progression to diffuse cartilage destruction. As is seen with other infectious or inflammatory arthropathies, varying degrees of perisynovial edema signal on T2 images and enhancement in addition to adjacent soft-tissue and marrow edema may be seen. Relatively unique to the seronegative arthropathies, the inflammation at the joint may begin first in the entheses, resulting in increased T2-signal inflammatory changes and postgadolinium enhancement at or in these tendinoligamentous insertions, and within the underlying marrow and adjacent soft tissues ( Fig. 10 ). When present, this enthesitis may help to differentiate the seronegative arthropathies from RA. Manifestation of enthesitis may be limited to peritendinous or periligamentous edema.