Tumors of the small intestine represent less than 5% of all gastrointestinal tract neoplasms. Magnetic resonance (MR) imaging is rapidly increasing clinical acceptance to evaluate the small bowel and can be the initial imaging method to investigate small bowel diseases. MR examinations may provide the first opportunity to detect and characterize tumors of the small bowel. Intraluminal and extraluminal MR findings, combined with contrast enhancement and functional information, allow accurate diagnoses and consequently characterization of small bowel neoplasms. This article describes the MR findings of primary small bowel neoplasms and the MR findings for the differential diagnosis are discussed.
Key points
- •
Small bowel tumors are rare neoplasms, representing less than 5% of all gastrointestinal tract tumors.
- •
Intraluminal and extraluminal magnetic resonance (MR) findings, combined with contrast enhancement and functional information, allow accurate diagnoses and characterization of small bowel neoplasms.
- •
MR enteroclysis is an imaging modality that combines the advantages of enteroclysis and multiplanar MR and should be recommended for the initial investigation in suspected small bowel tumors.
Introduction
Although the small intestine encompasses more than 90% of the mucosal surface area of the gastrointestinal tract, small bowel neoplasms are rare, accounting for 3% to 6% of all gastrointestinal tract neoplasms.
Patients with bowel tumors can be asymptomatic or may present vague symptoms such as abdominal pain, weight loss, or gastrointestinal bleeding.
The diagnosis is complicated further by the nonspecific nature of these symptoms and commonly by a low index of clinical suspicion, which makes the detection of these neoplasms a challenge for physicians and radiologists.
Inadequate radiologic examinations or incorrect interpretation of radiologic findings may cause further delays in diagnosing primary neoplasms of the small intestine.
Either benign or malign tumors may cause complications such as intussusception, obstruction, or perforation.
Although conventional enteroclysis and capsule endoscopy are the most common procedures for visualizing mucosal abnormalities of the small bowel, they cannot evaluate the mural and extramural extent of small bowel neoplasms, with no possibility of complete staging of the tumor. Computed tomography (CT) and magnetic resonance (MR) are frequently used in suspicion of tumor of the small bowel.
Common small bowel tumors typically are well evaluated with cross-sectional imaging modalities such as CT and MR, but accurate identification and differentiation can be challenging. Differentiating normal bowel from abnormal tumor depends on imaging modality and the particular technique.
Although endoscopic evaluation is typically more sensitive for the detection of intraluminal tumors that can be reached, CT and MR, as well as select nuclear medicine studies, remain superior for evaluating extraluminal neoplasms.
MR imaging offers numerous advantages with its excellent soft tissue contrast resolution, multiplanar imaging capability, and a lack of ionizing radiation. Furthermore, data acquisition can be repeated over time for functional evaluation of small bowel mobility, which is helpful for diagnosing low-grade stenosis and determining the level of obstruction.
Understanding the imaging characteristics of typical benign and malignant small bowel tumors is critical, because of overlapping features and associated secondary complications.
Small bowel tumors
The most common benign tumors are lipoma, adenoma, leiomyoma, hemangioma, and gastrointestinal stromal tumor (GIST; this also exists in a malignant form), whereas the most frequent malignant tumors are lymphoma, neuroendocrine tumor, metastatic disease, and primary small bowel adenocarcinoma.
The appearance of the lesions on MR imaging, combined with the contrast enhancement behavior and the characteristics of stenosis, can help to differentiate neoplasms of the small bowel (the main features are shown in Table 1 ).
| Histology | Common Site | T 1 Signal | T 2 Signal | Contrast Enhancement | MR Fluoroscopy |
|---|---|---|---|---|---|
| Adenoma | Jejunum | Low | High | Marked homogeneous | Intraluminal submucosa |
| Leiomyoma | Proximal ileum | Low | Low | Marked homogeneous | Intraluminal submucosal/extraluminal |
| Lipoma | Ileum | High | High; low at fat saturation | Absence | Intraluminal |
| Hemangioma | Jejunum | Low | High | Marked heterogeneous | Normal |
| GIST | Jejunum | Low | High heterogeneous | Marked heterogeneous | Extramural |
| Adenocarcinoma | Jejunum | Low | Low | Mild heterogeneous | Annular narrowing |
| Carcinoid | Distal ileum | Low | Low | Marked homogeneous | Intraluminal submucosal narrowing kinking |
| Lymphoma | Ileum | Low | Low | Mild heterogeneous | Stenosis or dilatation |
Benign tumors
Adenoma
Adenoma is the most common benign tumor of the small bowel. Adenomas are generally small (<2 cm) but may grow large enough to lead to obstruction or intussusception. The risk of malignant transformation in small bowel adenomas increases when their size exceeds 1 cm.
Adenoma may present with 3 possible patterns: a polypoid pedunculated mass on a stalk, a sessile mass (broad based and without a stalk), and a mural nodule within the mucosa.
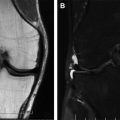
It appears as an intraluminal homogeneous enhancing mass on gadolinium-enhanced fat-suppressed images, confined within the boundaries of intestinal lumen. Single shot fast spin echo (ssFSE) and Steady state GRE sequences show a rounded low-signal-intensity intraluminal mass, whereas MR fluoroscopy sequences show an intraluminal filling defect with mild narrowing of the lumen, which is not usually associated with proximal dilatation ( Fig. 1 ).

Leiomyoma
Small bowel leiomyomas are rare mesenchymal neoplasms with a predilection for the esophagus, although, in the small bowel, they are more frequently in the jejunum than in the ileum.
Depending on their location, leiomyomas may protrude into the lumen or produce a mass effect on adjacent bowel. A small bowel leiomyoma appears as a homogeneous focal round mass with intense uniform enhancement.
Leiomyoma shows benign features with uniform enhancement greater than that of adjacent bowel on postgadolinium images, without mesenteric involvement or metastases. On MR fluoroscopy, leiomyoma appears as a smooth, round, or semilunar mural defect that is demarcated by sharp angles to the intestinal wall.
Lipoma
Lipomas are mature adipose tissue proliferations arising in the submucosa of the bowel wall; the ileum is the most frequent location. They usually grow intraluminally but occasionally extend outward in the mesenteric surface.
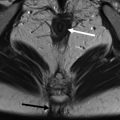
Submucosal lipomas appear as sharply demarcated, sessile, small intraluminal lesions with high signal on T 1 -weighted images and isointensity comparable with intra-abdominal fat on T 2 -weighted images. On T 1 -weighted and T 2 -weighted fat-suppressed images these lesions show a loss of signal intensity. After gadolinium injection, lipomas show no enhancement ( Fig. 2 ).

Hemangioma
Intestinal hemangiomas are usually submucosal tumors, most frequently located in the jejunum, and are sessile or pedunculate.
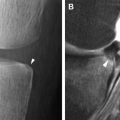
Hemangiomas show low signal intensity on T 1 -weighted images and marked hyperintensity on T 2 -weighted images; marked nodular enhancement is seen within the tumor in the arterial phase and homogeneous enhancement in the delayed phase ( Fig. 3 ).

Diffuse angiomatosis of the ileum appears as multiple nodules with low signal intensity on T 1 -weighted images and marked hypersignal on T 2 -weighted images; central nodular enhancement is seen within the tumor in the arterial phase with centrifugal enhancement on delayed phase.
Benign/malignant tumors
Gastrointestinal Stromal Tumor
GIST is the most common mesenchymal neoplasm of the gastrointestinal tract, including both benign and malignant varieties, and they are most commonly seen in patients more than 40 years of age.
GISTs arise from interstitial cells of Cajal and almost always express a specific tyrosine kinase growth factor receptor known as c-KIT (cluster of differentiation [CD] 117), which differentiates them from true leiomyomas. Seventy percent of GISTs are located in the stomach, 20% to 30% in the small bowel, and 7% in the anus or rectum.
Unlike adenocarcinomas, GISTs usually have an exophytic growth with involvement of the outer muscular layer of the bowel. Ulceration of the mucosa is seen in 50% of cases.
On MR imaging, a GIST typically appears as an exophytic, sometimes bulky mass that can extend to several centimeters in size, displacing the adjacent bowel loops.
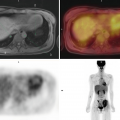
Following intravenous administration of contrast media, GISTs are typically enhancing masses with areas of low attenuation from hemorrhage, necrosis, or cyst formation.
Unlike adenocarcinoma, GIST does not involve the bowel wall concentrically and consequently bowel obstruction is rare, despite its large size. The intraluminal component accounts for a small proportion of tumors. The primary lesion is large and is the predominant finding. Mesenteric masses are usually well defined with a smooth surface without spiculation or indrawing of mesentery. Like lymphoma, GIST can also show aneurysmal dilatation of the bowel.
Tumor diameter greater than 10 cm and local invasion are strong indicators of malignancy. However, even larger tumors tend to displace adjacent structures rather than invade. Malignant GISTs can present with metastases to the liver, omentum, and peritoneum ( Figs. 4 and 5 ).


Malignant tumors
Adenocarcinoma
Primary small bowel carcinoma is rare, representing less than 2% of all gastrointestinal tumors, but is the most common primary small bowel malignancy. More than 50% of tumors are located in the duodenum, followed by the jejunum and then the ileum. Those arising from the jejunum are most often within 30 cm of the ligament of Trietz.
Small bowel primary adenocarcinoma of small bowel has an aggressive clinical nature with poor prognostic indicators including T3 disease (tumor, node, metastasis [TNM] staging: tumor has penetrated through the mucosa, submucosa, and muscularis propria and into the subserosa but not through the serosa) and T4 disease (tumor has penetrated through the serosa and may have invaded nearby tissues or organs), N1 and N2 lymph node metastasis, and distal metastasis.
Adenocarcinomas may be polypoid, infiltrating, or stenosing. Duodenal adenocarcinomas are often more circumscribed, with polypoid or protuberant appearance, whereas jejunal or ileal lesions tend to be larger, annular, constricting tumors with circumferential involvement of the intestine wall. It is common to find fully parietal penetration and involvement of the serosal surface.
On MR imaging, adenocarcinomas may appear as infiltrative lesions that cause luminal stenosis and obstruction with prestenotic dilatation, whereas polypoid intraluminal masses are less common; ulceration is a common feature ( Fig. 6 ).