Interventional MR uses rapid imaging to guide diagnostic and therapeutic procedures. One of the attractions of MR-guidance is the abundance of inherent contrast mechanisms available. Dynamic procedural guidance with real-time imaging has pushed the limits of MR technology, demanding rapid acquisition and reconstruction paired with interactive control and device visualization. This article reviews the technical aspects of real-time MR sequences that enable MR-guided interventions.
Key points
- •
Interventional MR imaging requires a specialized environment and work-flow.
- •
Rapid image acquisition and rapid image reconstruction are a prerequisite for all MR-guided interventions.
- •
High frame-rate real-time imaging can be achieved for dynamic procedural guidance.
- •
Imaging can be accelerated using parallel imaging or efficient k-space trajectories.
- •
MR imaging can enable simultaneous device and tissue visualization.
Introduction
Interventional MR imaging is valuable for real-time dynamic procedural guidance and intraprocedural imaging during diagnostic or therapeutic procedures, including surgery, tissue biopsy, ablation therapy, endovascular procedures, and device placement. The flexibility of MR image contrast is appealing for procedural guidance; however, the demands of MR-guided interventions are unique and require a specialized environment.
Diagnostic MR imaging is well established in the clinic to provide high-resolution images with excellent soft-tissue contrast, designed to assess pathologic tissue and derive quantitative metrics. Typically diagnostic MR imaging uses long scan times to generate the desired image contrast, and may require offline image reconstruction or processing.
Interventional MR imaging, on the other hand, demands much faster image acquisition, reconstruction, and processing. Furthermore, procedural guidance uses interactive parameter control and requires the simultaneous visualization of tissue and interventional devices (eg, biopsy needles, guide wires, catheters, stents, occluders, forceps). Table 1 summarizes the differing demands of diagnostic and interventional MR imaging.
| Diagnostic MR Imaging | Interventional MR Imaging |
|---|---|
| Scans run in batch mode | Interactive environments are used to modify real-time imaging on-the-fly |
| Long scan times | Short scan times |
| Offline reconstruction and postprocessing is possible | Reconstruction and processing must be performed with low latency |
| Image quality is of utmost importance | Imaging speed is of utmost importance |
| Used for anatomic imaging | Used for anatomic imaging and device imaging |
| Cardiac and respiratory gating and/or breath-holding can be used to compensate for motion | Real-time imaging is not gated or breath held |
Introduction
Interventional MR imaging is valuable for real-time dynamic procedural guidance and intraprocedural imaging during diagnostic or therapeutic procedures, including surgery, tissue biopsy, ablation therapy, endovascular procedures, and device placement. The flexibility of MR image contrast is appealing for procedural guidance; however, the demands of MR-guided interventions are unique and require a specialized environment.
Diagnostic MR imaging is well established in the clinic to provide high-resolution images with excellent soft-tissue contrast, designed to assess pathologic tissue and derive quantitative metrics. Typically diagnostic MR imaging uses long scan times to generate the desired image contrast, and may require offline image reconstruction or processing.
Interventional MR imaging, on the other hand, demands much faster image acquisition, reconstruction, and processing. Furthermore, procedural guidance uses interactive parameter control and requires the simultaneous visualization of tissue and interventional devices (eg, biopsy needles, guide wires, catheters, stents, occluders, forceps). Table 1 summarizes the differing demands of diagnostic and interventional MR imaging.
| Diagnostic MR Imaging | Interventional MR Imaging |
|---|---|
| Scans run in batch mode | Interactive environments are used to modify real-time imaging on-the-fly |
| Long scan times | Short scan times |
| Offline reconstruction and postprocessing is possible | Reconstruction and processing must be performed with low latency |
| Image quality is of utmost importance | Imaging speed is of utmost importance |
| Used for anatomic imaging | Used for anatomic imaging and device imaging |
| Cardiac and respiratory gating and/or breath-holding can be used to compensate for motion | Real-time imaging is not gated or breath held |
Imaging protocols
Interventional MR imaging encompasses preprocedural imaging for planning, intraprocedural imaging to assess progress, and real-time imaging for dynamic procedural guidance. The preprocedural and intraprocedural imaging is used to assess anatomy, physiology, or pathology relevant to the procedure. This article focuses primarily on the technical details of the rapid real-time imaging used during dynamic procedural guidance.
Real-Time Imaging
Imaging efficiency is crucial during MR-guided interventions, especially when competing against established interventional modalities such as radiography and ultrasonography. Radiography generates approximately 15 frames/s with a pixel matrix of 1024 × 1024. In comparison, 5 to 10 frames/s are used for MR imaging during procedural guidance with a much smaller pixel matrix of 128 × 128 or 144 × 192. Real-time imaging is not gated nor breath held, and the entire image is acquired in a single shot. Fig. 1 shows the single-shot real-time image acquisition running continuously, with multiple slices updating in rapid succession. Throughout an interventional procedure, slice geometry and image contrast are interactively controlled, either by interventionists in the MR suite or by operators in the control room.
For real-time procedural guidance, the challenge is to generate adequate tissue contrast and sufficient image quality in terms of signal-to-noise ratio (SNR) and artifact, while also maintaining short imaging times. Typically, balanced steady-state free precession (bSSFP) imaging is used to accomplish this. bSSFP uses magnetization efficiently to provide high SNR with short repetition times, and the resulting images have T2/T1-weighted contrast with bright blood and fat signal, and darker muscle tissue. Fully sampled bSSFP images can achieve a temporal resolution of 377 milliseconds per image or 2.6 frames/s (echo time [TE]/repetition time [TR] = 1.27/2.62 milliseconds, matrix = 192 × 144). Using parallel imaging, the temporal resolution can be pushed to 94 milliseconds per image or 10.6 frames/s (acceleration factor 4, see Parallel Imaging section). Banding artifacts in bSSFP are not usually a concern for these short TR sequences; however, real-time bSSFP does suffer from undesirable bright signal from fat. If needed, fat suppression for bSSFP can be accomplished using radiofrequency (RF) cycling and TR alternation. Real-time imaging can also be achieved using spoiled gradient echo sequences, although these are used less frequently because of the lower SNR.
A magnetization preparation module can be programmed into the pulse sequence such that it is toggled on/off interactively while the single-shot acquisition runs continuously. For example, nonselective saturation prepulses can be added to the sequence to enhance gadolinium contrast while suppressing tissue signal (see Device Visualization section). Furthermore, flow-sensitive saturation preparations can produce dark-blood images to enhance the gadolinium contrast and preserve tissue signal. Inversion pulses can be inserted into the real-time pulse sequence for infarct imaging. Interactive color-flow MR imaging using phase contrast has been implemented to rapidly visualize cardiac and vascular flow. Virtual dye angiography uses volume-selective saturation pulses that can be turned on/off interactively to provide flow visualization, mimicking contrast angiography during endovascular procedures ( Fig. 2 ). These interactive magnetization preparation modules modify image contrast, as needed, throughout the procedure.
Parallel Imaging
Parallel imaging can be used to accelerate real-time imaging by skipping some phase-encoding lines throughout the acquisition and exploiting multichannel signal receiver arrays during reconstruction for added spatial encoding. By eliminating some phase-encoding steps, the resulting images are aliased. Parallel imaging describes a family of reconstruction techniques that allows recovery of images from the aliased ones. The 2 most common methods used in the clinic are SENSE and GRAPPA. Excellent reviews of parallel imaging techniques are available.
Each point in an aliased single-coil image is a linear signal superposition with weights according to the coil sensitivity profile ( Fig. 3 ). SENSE reconstruction unambiguously unfolds aliased images by solving a linear system using knowledge of coil sensitivity maps calibrated at the beginning of the examination. TSENSE is an alternative algorithm, which uses interleaved undersampling to integrate the coil sensitivity maps with the image acquisition. TSENSE is specifically designed for dynamic imaging and is critical for high frame-rate imaging.
GRAPPA aims to regenerate the missing phase-encoding lines from the raw k-space data using information about a given data point contained within the neighboring points in k-space. GRAPPA requires a fully sampled region of k-space known as the autocalibration signal that is used to calculate a kernel to regenerate all missing k-space points. GRAPPA is robust in cases where sensitivity maps are difficult to generate, for example, when the prescribed field of view is too small for the imaged object and there are regions with aliasing in the calibration data.
In general, acceleration rates of 4 are robustly used in a clinical setting, and both SENSE and GRAPPA reconstructions are available with vendor-supplied reconstruction software.
Compressed sensing algorithms show potential for further accelerating image acquisition, but are currently limited in their application to interventional MR imaging by prohibitively long reconstruction times.
Efficient k-Space Trajectories
More efficient k-space trajectories can also be used to speed up image acquisitions ( Fig. 4 ). Echo planar imaging (EPI) is an accelerated Cartesian acquisition whereby multiple phase-encoding steps are acquired following an RF pulse. Using single-shot EPI the entire image can be acquired following a single RF pulse. EPI has found clinical utility for interventional and real-time applications.
Spiral imaging and radial imaging are examples of non-Cartesian acquisitions used for MR-guided interventions. Spiral imaging is particularly attractive for high frame-rate applications in the interventional MR imaging environment. Oversampling of the k-space center in non-Cartesian sampling patterns results in flow and motion insensitivity and robustness to aliasing artifacts. Either spoiled gradient echo or bSSFP contrast can be achieved with spiral and radial trajectories.
Spiral and radial k-space trajectories do not lie on a Cartesian grid and, therefore, require samples to be interpolated onto a grid during image reconstruction in a process called regridding. Typically regridding uses a Kaiser-Bessel kernel or, in the case of nonuniform fast Fourier transformation, using least-squares design of interpolation coefficients. Because sampling density is nonuniform over k-space, density compensation is applied before regridding. Alternatively, radial acquisitions can be reconstructed using back-projection methods originally designed for computed tomography reconstruction.
Parallel imaging can be combined with non-Cartesian acquisitions. Undersampling is achieved by omitting spiral interleaves or radial projections from the acquisition. For non-Cartesian trajectories, the resulting aliasing is irregular and classic SENSE unfolding is impossible. Instead, an iterative method, namely, conjugate gradient SENSE, is used to solve the linear system. GRAPPA reconstruction can also be performed with undersampled non-Cartesian data sets ; however, non-Cartesian GRAPPA schemes are currently incompatible with the interventional environment because of the large number of fully sampled calibration frames required. Approaches to reduce the number of calibration scans are under development. Readers are directed to reviews on non-Cartesian imaging for further details.
Keyhole Imaging
Keyhole imaging increases apparent frame rate by reconstructing consecutive images combining newly acquired data with data acquired from previous frames. Non-Cartesian sampling patterns are better suited to keyhole reconstruction because the center of k-space is reacquired with each interleaf/projection, and a full range of spatial frequencies is contained in both new and old data.
Fast Reconstruction
For interventional applications, fast acquisition is only valuable if it is paired with fast reconstruction. MR system vendors provide the capability to reconstruct Cartesian images with standard parallel imaging in real time. However, for more complicated reconstructions (eg, non-Cartesian imaging, complex parallel imaging schemes, or iterative reconstructions), additional reconstruction tools are necessary.
Imaging with large coil arrays is computationally costly. Several algorithms have been proposed for coil selection to choose the most suitable subset of coils for reconstruction, and array compression to combine channels for reducing reconstruction time. Most notably, principal component analysis has been used for array compression without the need for coil sensitivity maps.
Graphics processing unit (GPU) accelerated computing has been used for significant improvements in reconstruction speed, has been applied to advanced 3-dimensional reconstructions, parallel imaging, and nonuniform FFT. An 85-fold acceleration compared with a state-of-the-art 64-bit central processing unit has been reported. GPU-accelerated computing requires additional hardware that may not be available on the vendor-supplied reconstruction system.
An open-source software package (Gadgetron, http://gadgetron.github.io ) for medical image reconstruction has recently been made available. The software contains standard reconstruction tools, iterative solvers, and GPU components; it is designed to run on either the local MR computer, an external workstation, or multiple nodes in a distributed computing environment. Images may be piped directly to the host computer for online display. This framework permits complicated reconstructions in a reasonable time frame, with image display on the MR imaging host computer.
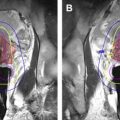
Device Visualization
Real-time device visualization is also necessary during MR imaging–guided interventions. Passive visualization uses the intrinsic material properties. For example, metallic devices (eg, biopsy needles, guide wires, stents, occluders) create a signal void on real-time MR images because they distort the local magnetic field, leading to local signal dephasing. Signal voids can be emphasized using long TE gradient echo sequences. Alternatively, positive contrast techniques whereby the metallic device appears bright compared with the background signal can be used for real-time visualization. Nonmetallic devices, such as plastic catheters, can be made visible on real-time imaging by filling the lumen with gadolinium, although it restricts use of the lumen to deliver other devices or agents. Balloon catheters filled with air, gadolinium, or carbon dioxide have been used to guide right heart catheterization under MR-guidance. Saturation prepulse modules are used to enhance gadolinium contrast of catheter devices ( Fig. 5 ).