Clinical Presentation
The patient is a 63-year-old female with a history of thyroid cancer who presented with a recent 3-day history of neck pain, left arm weakness, and numbness of the left upper extremity. There are no symptoms involving the right upper extremity or lower extremities. She has no difficulty walking. There are no bowel or bladder symptoms.
Imaging Presentation
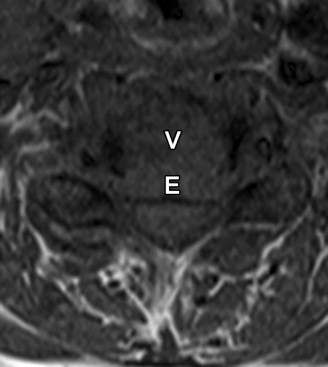
Sagittal T1-weighted and fat-saturated, T2-weighted images of the cervical spine show collapse of the C5 vertebral body with retropulsion of bone into the spinal canal causing compression and subtle increased T2 signal intensity within the cervical cord. The entire C5 vertebral body is replaced by abnormal decreased T1/increased T2 signal intensity compatible with metastatic disease in this patient with primary thyroid cancer. The increased cord signal intensity is consistent with spinal cord ischemia ( Fig. 46-1 ) .

Discussion
Spinal fractures are common lesions and are a cause of significant back pain, which can lead to mechanical instability and neurologic deficits, ranging from radiculopathy to spinal cord compression and cauda equina syndrome. Differentiating between malignant and benign causes of a vertebral fracture is a problem that every radiologist faces. Referring physicians often press the radiologist to commit to a diagnosis although often a diagnosis is not obvious. Particularly difficult is the solitary fracture of a vertebral body in an elderly patient with a history of malignancy after minor or no trauma. The patient’s advanced age puts him or her at a higher risk for a benign (osteoporotic) fracture; however, the history of malignancy increases the chance that the fracture is pathologic. The correct diagnosis is important with regard to clinical staging (if malignant), treatment, and prognosis.
Both malignant and benign vertebral fractures are just that, fractures, with imaging demonstrating varying degrees of loss of vertebral height. The most common cause of malignant vertebral collapse is metastatic disease from breast carcinoma, bronchogenic carcinoma, prostatic carcinoma, or renal carcinoma. The spine is a common site for metastatic disease. Up to 39% of all bone metastases are in the spine. Malignant collapse can also occur as a result of a primary bone neoplasm such as multiple myeloma, solitary plasmacytoma, or lymphoma. Benign compression fractures are typically caused by osteoporosis. Other benign causes include trauma, eosinophilic granuloma, Paget’s disease, and hemangioma.
Imaging Features
Short of evaluating tissue for pathology via percutaneous or open biopsy, the radiologist can make a best guess as to the benignancy or malignancy of a vertebral lesion. Magnetic resonance (MR) imaging is the method of choice for evaluating a marrow infiltrative process such as a pathologic fracture although computed tomography (CT) can be used as well.
MR imaging findings that are suggestive of a malignant compression fracture include a convex bulging of the posterior cortex of the fractured vertebral body (found in 74% of metastatic fractures versus 20% of acute osteoporotic fractures), abnormal signal intensity extending into the pedicle (found in 85% of metastatic fractures versus 51% of acute osteoporotic fractures), or posterior elements (found in 59% of metastatic fractures versus 24% of acute osteoporotic fractures), an epidural mass (found in 74% of metastatic fractures versus 25% of acute osteoporotic fractures), and an associated paraspinal mass (found in 41% of metastatic fractures versus 7% of acute osteoporotic fractures).
MR imaging findings that are suggestive of an acute osteoporotic compression fracture include a low signal intensity band on T1-weighted images that parallel the vertebral endplate (found in 93% of acute osteoporotic fractures versus 44% of metastatic fractures), a region of spared normal bone marrow signal intensity (found in 85% of acute osteoporotic fractures versus 19% of metastatic fractures), a retropulsed posterior bone fragment (found in 60% of acute osteoporotic fractures versus 11% of metastatic fractures), and multiple compression fractures (found in 58% of acute osteoporotic fractures versus 33% of metastatic fractures). A new fracture in a patient with multiple chronic fractures with normal signal intensity makes the new fracture more likely to be an osteoporotic fracture; however, each new fracture must be individually evaluated, because malignant fractures and osteoporotic fractures can exist in the same patient.
CT can be useful for distinguishing between benign and malignant acute vertebral compression fractures. Cortical fractures without associated cortical destruction suggest a benign etiology. This is seen in nearly all acute osteoporotic compression deformities and in only 9% of malignant compression deformities. Fracture of the cortical bone of a vertebral body has a high diagnostic accuracy (95%) of an osteoporotic fracture, and cortical destruction has a high diagnostic accuracy (97%) for malignancy. Retropulsion of a bone fragment into the spinal canal is seen in 35% of patients with benign compression fractures and in only 3% with malignant compression fractures. Retropulsion of a bone fragment must be distinguished from posterior convex bulging of the cortex seen with malignancy. Gas seen within the fractured vertebral body (gas cleft) is suggestive of a benign etiology, seen in 15% of osteoporotic acute compressions and rarely in malignant compressions. Traditionally, it has been taught that a paraspinal soft tissue mass associated with a fracture is a sign of a malignant fracture. However, osteoporotic fractures can often be associated with small paraspinal soft tissues masses in their acute phase. The paraspinal mass with osteoporotic fractures generally surrounds the entire vertebral body, is less than 10 mm in thickness, and is of equal thickness all the way around or slightly more predominant anteriorly. Malignant paraspinal masses are typically more eccentric in shape and involve only a portion of the periphery of the vertebral body.
The CT findings more frequently found in malignant acute vertebral compression fractures are destruction of cortical and cancellous bone, destruction of a pedicle, an associated epidural mass, and an eccentric paraspinal mass. Destruction of cancellous bone and the paraspinal mass have a lower specificity for malignancy than destruction of cortical bone, pedicle destruction, and epidural mass. Destruction of cancellous bone can be seen in up to 29% of patients with osteoporotic acute compression deformities.
MR imaging is the preferred modality for evaluating acute vertebral compressions not only for diagnosing malignant versus benign causes, but also to identify the relationship of the fracture to the spinal cord and nerve roots. Acute malignant compressions demonstrate complete/near complete replacement of the vertebral body with low T1 signal intensity ( Fig. 46-1, A , and 46-2 ). Complete replacement is the rule because malignant fractures usually do not occur until the entire vertebral body is affected. T2 signal can be variable, depending on the type of cancer and whether the lesion is sclerotic, and also depends on whether a fat-suppression technique was used (see Fig. 46-1, B ). There is often diffuse or patchy heterogeneous enhancement ( Fig. 46-3 ) . Similar signal abnormality may be identified involving the pedicles ( Fig. 46-4 ) . There may be an associated paraspinal soft tissue or epidural mass. With malignant fractures, the T1 signal intensity does not revert back to normal fatty marrow signal intensity as it does with osteoporotic fractures.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








