CHAPTER 4 ![]()
Mammographic Technique and Image Evaluation
Summary of Important Points
ROUTINE BREAST IMAGING
Breast Compression
Breast compression is under the discretion of the mammographer and will depend on the patient’s breast sensitivity and size. In general, the breast should be compressed until taut to fingertip pressure to ensure adequate compression. Often, after the automatic compression stops, manual compression must be applied to adequately immobilize and compress the breast. Although too little compression will compromise image quality, the compression should not be applied to cause the patient severe pain.
Main Reason for Breast Compression
• Compression allows a uniform density by flattening the posterior breast to the same degree as the more anterior regions, permitting optimal imaging of the entire breast on 1 exposure.
Added Advantages of Breast Compression
• The tissue thickness of the compressed breast is less than that of the uncompressed breast which means that lower radiation is needed to penetrate the compressed breast allowing reduced radiation dose to the patient.
• Compression brings lesions closer to the detector for more accuracy when evaluating fine detail.
• Compression reduces the possibility of motion by immobilizing the breast during the exposure.
• Compression allows the use of lower peak kilovoltage (kVp) which allows increased contrast.
• Compression separates superimposed areas of glandular tissue by spreading apart overlapping tissue, allowing visualization of the borders of circumscribed lesions.
• Compression assists in capturing the breast tissue to include the posterior chest wall anatomy.
Routine Breast Imaging Projections
Typically, the routine 4-projection series in mammography involves imaging in the craniocaudal (CC) and the mediolateral oblique (MLO) of both breasts. The CC and MLO projections are complementary. The idea behind the 4-projection routine in mammography is to image both breasts with minimal radiation dose to the patient and to include the maximum amount of breast tissue possible.
Areas Best Demonstrated on the CC Projection
The CC projection breast demonstrates the anterior, central, medial, and posteromedial portions of the breast, but is poor at visualizing the lateral breast tissue. It is critical to include the medial breast on the CC projection. The medial breast may be inadvertently eliminated on the MLO because the breast is less mobile and cannot be stretched at its medial aspect (the sternum side).
Key Points of the CC Projection
• Position the detector at the level of the raised inframammary crease. The breast must be elevated before positioning the detector.
• Turn the patient’s head away from the side being examined.
• Position the patient’s feet apart with weight equally distributed.
• The ipsilateral arm is positioned by patient’s side.
• The contralateral arm is raised and the patient can hold the machine for support.
• Optimal compression is achieved if the patient is relaxed. To aid relaxation of the shoulder, place your hand on the ipsilateral shoulder and gently push down.
• Expose on suspended respiration but try to avoid telling the patient to take a deep breath before the exposure.
CC Evaluation
• The nipple should be in profile.
• The nipple should be centered on the radiograph; however, do not eliminate breast tissue to center the nipple.
• The medial and lateral aspects of the breast must be included in the collimated area.
• If possible, include the cleavage and a small amount of contralateral breast at the medial margin.
• The pectoralis major muscle is seen in approximately 30%-40% of the cases. If the pectoral muscle is seen on all cases imaging may be losing medial breast tissue.
• Appropriate markers and labeling must be used as required by Mammography Quality Standard Act (MQSA).
• The CC should include, within 1 cm, the posterior nipple line (PNL) measurement of the MLO.
• Dense areas of the breast should be adequately penetrated.
Areas Best Demonstrated on the MLO Projection
• The MLO projection demonstrates the extreme posterior and upper-outer quadrant but there is distortion of the anterior, central, and medial breast tissue.
• In imaging in the MLO projection, the detector must be parallel to the pectoralis muscle, which can vary from 30 to 60 degrees.
• The more parallel the detector is to the pectoralis muscle the more tissue will be included in the image.
Key points of the MLO Projection
• The degree of tube angulation will vary between 30 and 60 degrees, depending on the patient’s body habitus. Thin patients require steeper angulation than heavier patients.
• The correct detector or compression paddle size is needed to avoid stretching the pectoralis major muscle.
• Too much pectoral muscle under the compression plate, especially when imaging the male breast, will reduce compression to the anterior portions of the breast.
• The ipsilateral arm should be draped over the top of the detector.
• The detector should rest in the armpit, posterior to the midaxilla and anterior to the latissimus dorsi muscle.
• Compression must adequately support the anterior breast tissue to preventing sagging and distortion of the ductal architecture.
• Appropriate markers and labeling must be used, as required by MQSA.
• Expose on suspended respiration, but try to avoid telling the patient to take a deep breath before the exposure.
MLO Evaluation
• The pectoral muscle should be wide superiorly with a convex anterior border and should extend to or below the level of the PNL.
• The inframammary fold should be open.
• Dense areas of the breast should be adequately penetrated.
• There should be no drooping of the anterior breast and distortion of the architectural structures.
• Abdominal tissue should not overlap the breast tissue.
Supplementary Projection
• Supplementary projections become useful when the standard projections are inadequate.
• Supplementary projections can be used to image a patient when medical or surgical history or body build makes the standard projections difficult to obtain.
• Supplementary projections can be used to provide more details of a suspicious lesion or microcalcifications.
Supplementary Projections, Recognized by the ACR and ARRT
• 90-degree mediolateral (ML)
• 90-degree lateromedial (LM)
• Lateromedial oblique (LMO)
• Tangential projection (TAN)
• Exaggerated craniocaudal lateral or medial (XCCL or XCCM)
• Caudocranial or from below (FB)
• Cleavage or “valley view” (CV)
• Axillary tail (AT)
• Superoinferior oblique (SIO)
Other Modified Positions
• Rolled medial (RM) or rolled lateral (RL)
• Rolled inferior (RI) or rolled superior (RS)
• Magnification (M)
• Spot compression
The ACR also accepts that ruling out an abnormality could involve imaging the breast using any manipulation or technique that is not a part of the routine or supplementary series.
Mediolateral
This is a 90-degree lateral projection of the breast with the x-ray beam passing medial to lateral.
• Used to improve detail of a lesion located in the lateral aspect of the breast.
• Used to verify a finding or to localize a lesion in another dimension, e.g., during localization.
• Used to image breast tissue missed on the MLO, e.g., at the inframammary fold area.
• To triangulate a lesion seen on the MLO but not seen on the CC projection. When comparing the MLO and ML projections:
• Medial lesions move up on the lateral from their position on the MLO.
• Lateral lesions move down on the lateral from their position on the MLO.
• Central lesions will not change significantly from the MLO to the ML.
• Used to prove benign breast calcifications, e.g., milk of calcium.
Lateromedial
This is a 90-degree lateral projection of the breast with the x-ray beam passing lateral to medial.
• Used to improve details of a lesion located in the medial aspect of the breast.
• Used to verify a finding or to localize a lesion in another dimension. (e.g., during localization).
• Used during preoperative localization, giving a true representation of inferior and/or lateral lesions.
• Used to replace the MLO when imaging patients with difficult body habitus although the study may be limited because it does not image as much posterior breast as the routine MLO projection.
Lateromedial Oblique
This is a true reverse of the MLO projection with the x-ray beam directed inferolateral to superomedial.
• Used to evaluate the medial aspect of the breast.
• Used when the standard MLO projection is difficult to obtain because of patient body build such as prominent sternum.
• Used when the patient has a pacemaker or chest surgery to avoid pulling at the scar tissue and causing discomfort.
Tangential
This provides a profile projection of the area of interest, avoiding superimposition on other breast tissue. The x-ray beam skims the skin surface of interest.
• Used to confirm or locate skin calcification or skin lesions. A BB or lead spot marker can be placed over the area of interest during the exposure.
Exaggerated Craniocaudal Lateral or Medial
This is a CC projection of the posterior or medial breast tissue. The x-ray is directed superior to inferior with the patient positioned first for the CC then turned laterally or medially.
• Used to locate lesions in the lateral or medical aspect of breast not seen on the CC projection.
Caudocranial or From Below
This is a reverse of the CC projection, with the x-ray beam traveling inferior to superior. The tube is rotated 180 degrees with detector to the top.
• Used to better visualize lesions in the superior or upper quadrants of the breast.
• Used to image small breasts or the male breast.
• Used to image the kyphotic patient or patients with pacemakers.
The Cleavage or Valley View
This projection visualizes the deep medial breast tissue with the x-ray beam directed superior to inferior.
• Used to show lesions deep in the medial aspect of the breast, the area closest to the chest wall.
The Axillary Tail
This is an oblique projection of the tail of the breast that is customized, with the angle depending on the patient’s body habitus and/or radiologist request. The beam passes superomedial to inferolateral, perpendicular to the angle of the axillary tail.
• Used to visualize the tail of the breast.
The Superoinferior Oblique Projection
This is an oblique projection with the x-ray beam directed superolateral to inferomedial.
• Used to demonstrate the upper-inner quadrant and the lower-outer quadrant of the breast, free of superimposition.
• The 45-degree SIO is useful in providing a projection perpendicular to the MLO to help distinguish pseudomass from malignant lesions.
• The 45-degree SIO is useful when imaging the most posterior and inferior portion of the lower-outer quadrant of the breast.
• The 60-degree SIO can be used to visualize the breast free of implants using the Eklund technique.
Rolled Lateral or Rolled Medial
In these positions the breast is rolled laterally or medially after the patient is positioned for the CC projection. The idea is useful in removing superimposed tissue when imaging dense breast. The lesion is “rolled” off or away from the dense tissue.
• RL—after positioning the patient for the CC, the superior portion of the breast is rolled laterally and the inferior (lower) portion is rolled medially.
• RM—after positioning the patient for the CC, the superior portion of the breast is rolled medially and the inferior (lower) portion is rolled laterally.
Rolled Superior or Rolled Inferior
These are lateral positions used to remove superimposed tissue. The breast surface away from the detector is then rolled superiorly or inferiorly.
• RS—after positioning the patient for the ML, the medial portion of the breast is rolled superiorly and the lateral portion of the breast is rolled inferiorly.
• RI—after positioning the patient for the ML lateral, the medial portion of the breast is rolled inferiorly and the lateral portion of the breast is rolled superiorly.
Spot Compression
With spot compression more compression is applied to a localized area of interest using a small compression paddle. Spot compression can be performed in any projection or with or without magnification. It is not recommended for imaging of lesions directly behind the nipple; the small compression paddle will push or displace the lesion posteriorly.
• Used for localization of suspected abnormalities.
• Useful in applying additional compression when evaluating a suspicious area.
Magnification Mammography
Magnification images the breast with an increased OID which results in magnification of the part. A small focal spot must be used with magnification to improve the resolution and sharpness to compensate for the large OID. However, the large OID acts as an air gap in reducing the amount of scattered radiation reaching the detector. A grid is therefore not necessary.
• Used to improve visualization of fine details especially when analyzing calcifications.
• Used to evaluate the margins of lesions or the density of masses.
• Used to image specimens or surgical sites.
IMAGING IMPLANTS
The standard series of projections for a patient with an implant is the routine CC and MLO projections with limited compression, plus the Eklund projections which are often called implant-displaced (ID) projections. Most implants can be displaced by using the ID projections. The result is an 8-projection series.
• The “implant in place” imaging refers to the standard projection taken to demonstrate the posterior breast tissue surrounding the margins of the implant. Compression is used for immobilization only. Vigorous compression should not be applied to the implant.
• The implant-displaced technique requires pulling the natural breast tissue forward while simultaneously, pushing the implant back toward the chest wall. Maximum compression is therefore applied only to the breast tissue anterior to the implant.
• ID technique will work on all implants regardless of whether the implant is placed in front of the pectoral muscle (subglandular or retromammary implants) or behind the pectoral muscle (subpectoral implants), as long as the implant is not encapsulated.
Technique
• Before beginning positioning the mammographer must locate the extent of the implant by feeling for the edges (how far it extends).
• Next have the patient stand in the position for a routine CC or MLO.
• The patient then steps back, slightly away from the detector.
• The mammographer locates the anterior edge of the implant and places the detector anterior to the edge of the implant.
• The mammographer can use thumb and fingers to grasp the breast anterior to the implant and pull breast tissue forward.
• Compression begins while holding and pulling the breast tissue forward.
• The edge of the detector and the compression plate will help keep the implant posterior to the breast tissue and displaced from the field of view.
• The breast free of implant is compressed normally.
• If there is sufficient breast tissue to cover the detector, automatic exposure control can be use. However, if enough breast tissue does not cover the detector, manual technique must be used.
SPECIAL IMAGING SITUATIONS
Small Breast
• Manual technique is needed if the breast does not cover enough of the detector.
• The MLO is generally easier to perform and beginning the exam with the MLO will generally allow for using the AEC. Using the information provided from the MLO exposure will assist in choosing a manual technique for the CC images.
• Use a spatula if necessary.
• Roll or tilt the patient to the affected side.
• The FB can replace the CC.
Male Breast
• Imaging is similar to that of a small female breast.
• The FB is an option if the patient is mobile and especially when there is chest hair.
• Chest hair and too much pectoral muscle can present problems.
Large or Wide Breast
• Sectional imaging may be necessary.
• In any sectional imaging there must be at least 2.5 cm (1 inch) of breast tissue overlap.
• All images must be clearly labeled for proper evaluation, e.g., MLO upper or MLO lower.
Kyphotic Patients
• The FB can replace the CC or the XCCL and XCCM can be used.
• The LMO can replace the MLO.
• The LM, documented as a limited study, can replace the MLO.
Pectus Excavatum (Depressed Sternum)
• The XCCL and XCCM can replace the CC projection to image medial and lateral portions of the breast.
• The CV can be used to image medial breast.
• The LMO can replace the MLO.
• The LM, documented as a limited study, can replace the MLO.
Pectus Carinatum (Pigeon Chest—Prominent Sternum) and Barrel Chest (Prominent Ribs and Sternum)
• The XCCL and XCCM can replace the CC projection to image medial and lateral portions of the breast.
• The routine MLO plus AT can be used.
Postsurgical Breast
• Postlumpectomy imaging can include CC and ML or MLO imaging of the surgical site.
• Magnification can be used to evaluate calcifications.
• Other imaging may include a spot compression of the area of concern, and/or an AT projection.
Irradiated Breast
• Mammograms can be performed 6-12 months after completion of radiation treatment.
• Infection control is critical.
Stretcher/Cart Patients
• The CC imaging can be performed with the patient supine and the tube rotated 90 degrees.
• The FB can replace the CC with the patient supine and the tube rotated 90 degrees.
• The ML or LM, documented as a limited study, can replace the MLO with the patient lateral and the tube positioned at 0 degrees.
Wheelchair Patients
• The ML or LM, documented as a limited study, can replace the MLO.
• A bolster behind the patient can help straighten the spine and allow better positioning.
• If the chair arm is removed, the patient must be carefully monitored or supported.
Elderly Patient
• A chair examination may be necessary.
• The patient should be allowed to keep all walking aids, such as walkers or canes.
• All limitations should be documented.
Nipple Not in Profile
• Always image the entire breast first, then if necessary, image the nipple separately using nipple in profile projections.
• Using nipple markers can eliminate the need for added projections.
Skin Folds or Wrinkling of the Breast
• Skin folds or wrinkling may be impossible to avoid in the elderly.
• Smooth folds or wrinkles using the index finger during compression.
• Avoid pushing breast tissue outside of the compression field to eliminate a fold or wrinkle.
• Added projections will be needed if any breast tissue is eliminated when removing wrinkling or folds.
Breast Thickness
• When imaging for the MLO projection, the detector must be parallel to the pectoral muscle.
• Two images, the MLO and AT or the MLO and ML, for each routine projection may be necessary to image the posterior and anterior breast. Imaging the anterior portion of the breast to improve compression may be designated as “anterior compression” projections.
• Flex paddles can be used to avoid overcompression of posterior breast tissue to achieve adequate compression of anterior breast.
Protruding Abdomen
• CC and MLO imaging should start with the patient standing away from the unit and leaning forward.
• MLO imaging may need reduced tube angulation for better control of the anterior breast.
Frozen Shoulder
• The LMO or the LM can replace the MLO.
• Imaging for the MLO can be performed with the patient’s ipsilateral arm down.
• Any limitations should be documented.
Specimen Imaging
The specimen is the breast tissue sample removed during a biopsy. A radiograph of the specimen is necessary to ensure the area under suspicion is totally removed and the margins are clean. In imaging the specimen:
• Speed and efficiency are important because the patient may be under anesthesia.
• Always use compression when imaging larger specimens.
• Magnification may help to visualize microcalcifications.
MQSA IMAGING REQUIREMENT
MQSA requirements for image identification include:
• Name of patient and additional patient identifier, such as hospital number or medical records number.
• Date of examination.
• Projection indicator and right or left marker, placed near the axilla using standardized codes approved by the FDA.
• Facility name and location to include city, state, and zip code.
• Mammographer’s identification.
• Mammography unit identification if there is more than 1 unit at the facility.
• Cassette/screen identification for analog units.
Questions
1. Which of the following statements is true?
(A) Compression increases image sharpness by reducing the focal spot size.
(B) Compression decreases subject contrast by reducing the thickness of the penetrated tissue.
(C) Compression increases the uniformity of the breast, making diagnosis easier.
(D) The compressed breast requires increase kVp to penetrate the thicker tissue.
2. The maximum compression force applied to the breast should not exceed _______.
(A) 111 N (25 lb)
(B) 178 N (40 lb)
(C) 200 N (45 lb)
(D) none of the above
3. In assessing the degree of compression for any one patient, the mammographer should take into consideration
1. the maximum to which the patient’s breast can actually be compressed
2. the amount of compression the patient can tolerate
3. compression that should be just sufficient to immobilize the breast
(A) 1 only
(B) 1 and 2 only
(C) 1 and 3 only
(D) 2 and 3 only
4. Manual compression in mammography
(A) has a fixed upper and lower limit
(B) depends solely on breast size
(C) depends on breast size and the patient’s pain tolerance
(D) generally depends on the patient’s pain tolerance
5. Some considerations that could be given to women with painful breasts include
1. having the patient take ibuprofen prior to the mammogram
2. scheduling the mammogram during the menstrual cycle
3. explaining, before the examination, the importance of compression
(A) 1 only
(B) 1 and 2
(C) 2 and 3
(D) 1 and 3
6. When imaging using the FB, the area of the breast that will likely be missed is the
(A) medial
(B) lateral
(C) inferior
(D) posterior
7. Compression allows reduced radiation to the breast by
(A) providing a uniform breast thickness
(B) decreasing breast thickness
(C) decreasing motion unsharpness
(D) separating superimposed areas of glandular tissue
8. What principle does compression use to visualize the borders of circumscribed lesions?
1. It brings the lesion closer to the detector.
2. It spreads apart overlapping tissue.
3. It separates superimposed areas of glandular tissue.
(A) 1 only
(B) 1 and 2 only
(C) 2 and 3 only
(D) 1, 2, and 3
9. Ideally, breast compression is maximized when
1. accompanied by a thorough explanation to increase patient cooperation
2. the exposure is made on arrested inspiration to reduce motion
3. the patient recognizes the advantage of compression in reducing radiation dose
(A) 1 and 2 only
(B) 2 and 3 only
(C) 1 and 3 only
(D) 1, 2, and 3
10. Magnification can be used to assess the
(A) margins of a lesion
(B) size of a lesion
(C) location of a lesion
(D) density of a lesion
11. With calcifications, magnification can be used to assess
1. the number
2. morphology
3. distribution
(A) 1 only
(B) 1 and 2 only
(C) 2 and 3 only
(D) 1, 2, and 3
12. The last degree of compression should be applied
(A) using manual compression
(B) after the breast is released from compression
(C) with the automatic compression device
(D) with the mammographer’s hand between the breast and the compression paddle
13. Which projection is used to determine if a lesion is medial or lateral to the nipple?
(A) CC
(B) MLO
(C) TAN
(D) ML
14. If any breast tissue is poorly imaged on the MLO projection, it is likely to be
(A) medial breast tissue
(B) lateral breast tissue
(C) inferior breast tissue
(D) superior breast tissue
15. The length of the posterior nipple line (PNL), visualized on the CC, should be within how many centimeters of the PNL on the MLO?
(A) 0.25
(B) 0.50
(C) 1.00
(D) 1.50
16. Which of the following conditions must be met when imaging the breast in the MLO?
1. The pectoral muscle should extend to or below the PNL.
2. Visualized fat should be posterior to all the fibroglandular tissues.
3. The inframammary fold (IMF) should be open.
(A) 1 and 2 only
(B) 2 and 3 only
(C) 1 and 3 only
(D) 1, 2, and 3
17. In positioning for the CC projection, if the C-arm of the mammography unit is raised too high the IMF is overelevated, resulting in loss of
1 superior breast tissue
2. inferior breast tissue
3. posterior breast tissue
(A) 1 and 2 only
(B) 2 and 3 only
(C) 1 and 3 only
(D) 1, 2, and 3
18. The single projection that will best visualize the maximum amount of breast tissue is the
(A) CC
(B) MLO
(C) ML
(D) XCCL
19. In general, when imaging tall, thin patients the angulation is adjusted to
(A) below 30 degrees
(B) between 30 and 40 degrees
(C) close to 60 degrees
(D) over 70 degrees
20. The position used to determine whether an abnormality is superior or inferior to the nipple is the
(A) CC
(B) MLO
(C) XCCL
(D) TAN
21. The principle of mobile versus fixed tissue is used in mammography positioning to image the maximum
(A) medial breast on the MLO projection
(B) inferior breast on the CC projection
(C) superior breast on the MLO projection
(D) medial tissue on the CC projection
22. In the CC projection of the breast, the detector is positioned
(A) at the level of the raised inframammary crease
(B) below the level of the raised inframammary crease
(C) at the level of the inframammary crease
(D) just below the level of the inframammary crease
23. In positioning for the MLO, the tube is always angled
(A) 90 degrees
(B) 60 degrees
(C) 50 degrees
(D) none of the above
24. What position is shown in Figure 4-1?
(A) CC
(B) MLO
(C) CV
(D) XCCL
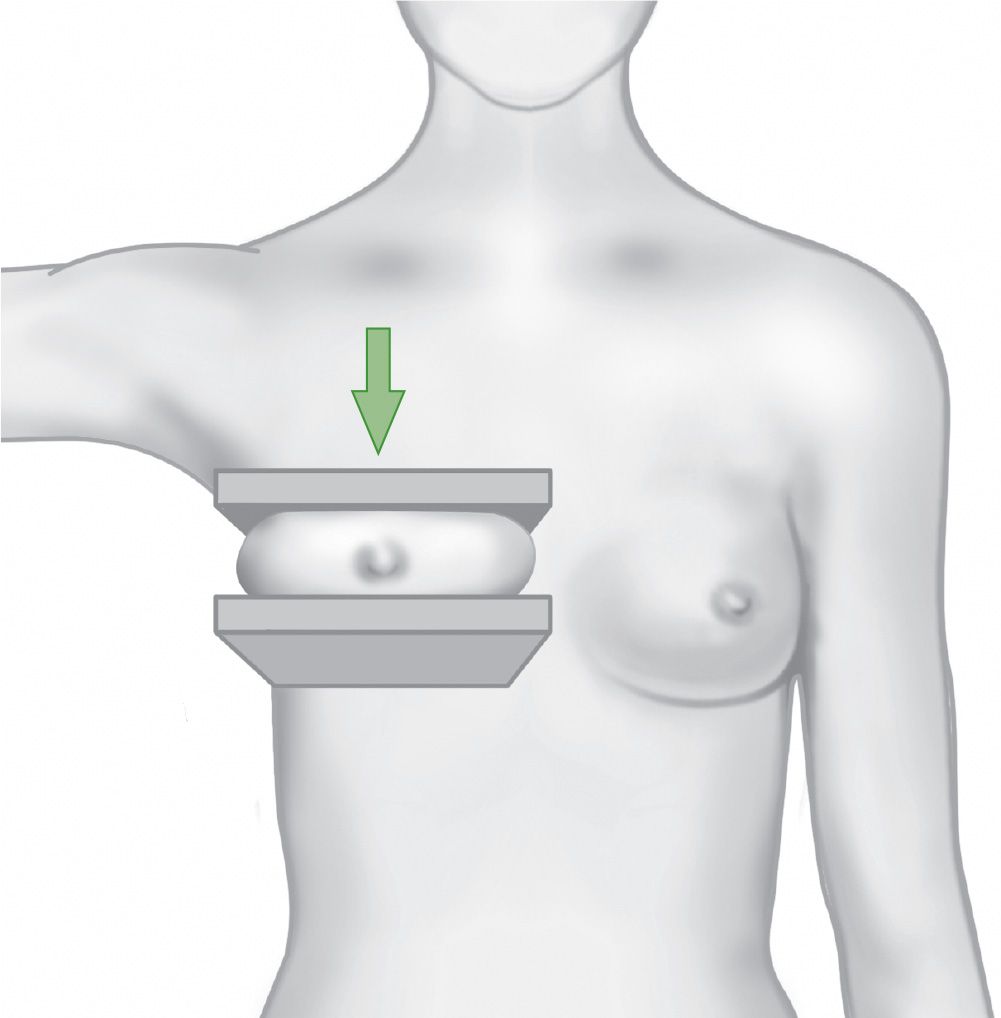
Figure 4-1.
25. When positioning for the right CC, where is the patient’s left arm placed?
(A) Brought back. This action rotates the shoulder to remove it from the imaging area.
(B) Brought forward. The patient can hold the handle bar of the unit.
(C) Brought forward. The patient can hold the detector.
(D) Remains at the patient’s side.
26. Your patient has had recent chest surgery and has a scarred and painful area running along the sternum. With the medial aspect of the breast immobile, which of the following is an alternative to the RMLO?
(A) RLMO
(B) LMLO
(C) LLM
(D) RML
27. Which projection is best used to visualize the tail of the breast?
(A) LMO
(B) TAN
(C) LM
(D) AT
28. Calcifications seen on the mammogram are suspected to be in the skin. The best projection necessary to prove this theory is the
(A) LMO
(B) TAN
(C) LM
(D) AT
29. The projection best used to demonstrate details of the medial breast structures of the breast is the
(A) LM
(B) AT
(C) ML
(D) TAN
30. A lesion on the lateral aspect of the breast is not seen on the CC. An additional projection used to image the lesion could be the
(A) CV
(B) XCCL
(C) FB
(D) TAN
31. Which projection can be used instead of the CC to image patients with severe kyphosis?
(A) ML
(B) TAN
(C) FB
(D) CV
32. A lesion moved up on the ML projection from its original position on the MLO. The location of the lesion within the breast is
(A) lateral
(B) medial
(C) inferior
(D) superior
33. Which projection can be used to prove breast calcifications are benign (teacup shaped)?
(A) CC
(B) XCCL
(C) FB
(D) ML
34. Which projection can be used to give a profile image of the area in question without superimposition of breast tissue?
(A) CV
(B) TAN
(C) LMO
(D) AT
35. Identify the projection shown in Figure 4-2.
(A) FB
(B) XCCL
(C) ML
(D) AT

Figure 4-2.
36. A barrel-chested patient whose chest wall protrudes outward may have breast tissue extending laterally under the arm. What projection, used to image the breast with the beam directed superiorly to inferiorly, should be taken in addition to the CC?
(A) AT
(B) XCCL
(C) CV
(D) MLO
37. The FB projection can be useful in imaging
1. patients with extreme kyphosis
2. abnormalities high on the chest wall or superior aspect of breast
3. inferior lesions or lesions near the IMF
(A) 1 and 2 only
(B) 2 and 3 only
(C) 1 and 3 only
(D) 1, 2, and 3
38. Identify the position shown in Figure 4-3.
(A) MLO
(B) CV
(C) LM
(D) ML

Figure 4-3.
39. Why is the MLO preferred to the ML as a routine projection?
(A) The MLO visualizes the medial breast.
(B) The ML does not visualize the medial breast.
(C) The ML poorly visualizes the posterior and lateral breast.
(D) The MLO does not distort the anterior structure of the breast.
40. Which projection best shows the extreme medial aspect of the breast?
(A) CC
(B) MLO
(C) ML
(D) CV
41. In which modified projection is the superior aspect of the breast rolled medially?
(A) RM
(B) RL
(C) M
(D) LM
42. In the LMO projection, the beam is directed from the
(A) upper-inner aspect to the lower-outer aspect of the breast
(B) inner-outer aspect to the upper-outer aspect of the breast
(C) lower-outer aspect to the upper-inner aspect of the breast
(D) superolateral aspect to the inferomedial aspect of the breast
43. Identify the projection shown in Figure 4-4.
(A) MLO
(B) CV
(C) LM
(D) ML
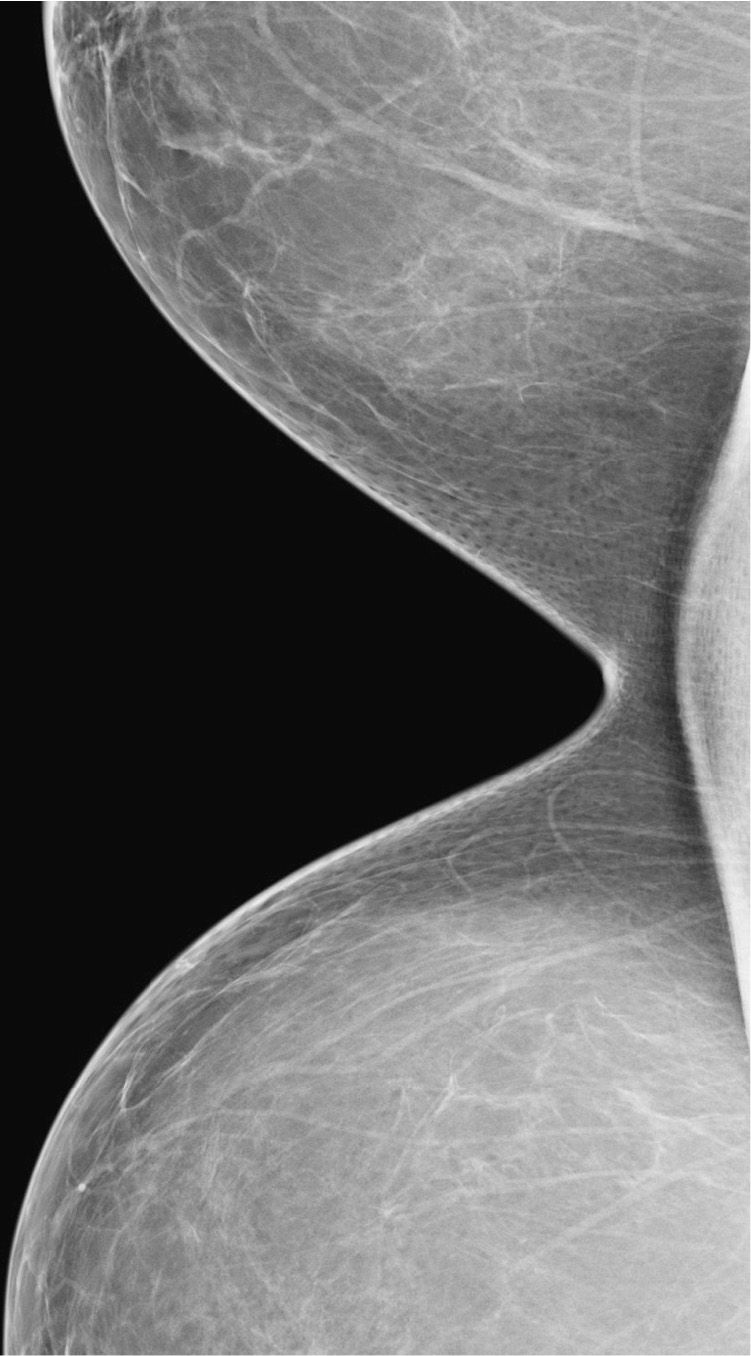
Figure 4-4.
44. Identify the position shown in Figure 4-5.
(A) RM
(B) CV
(C) RL
(D) MLO
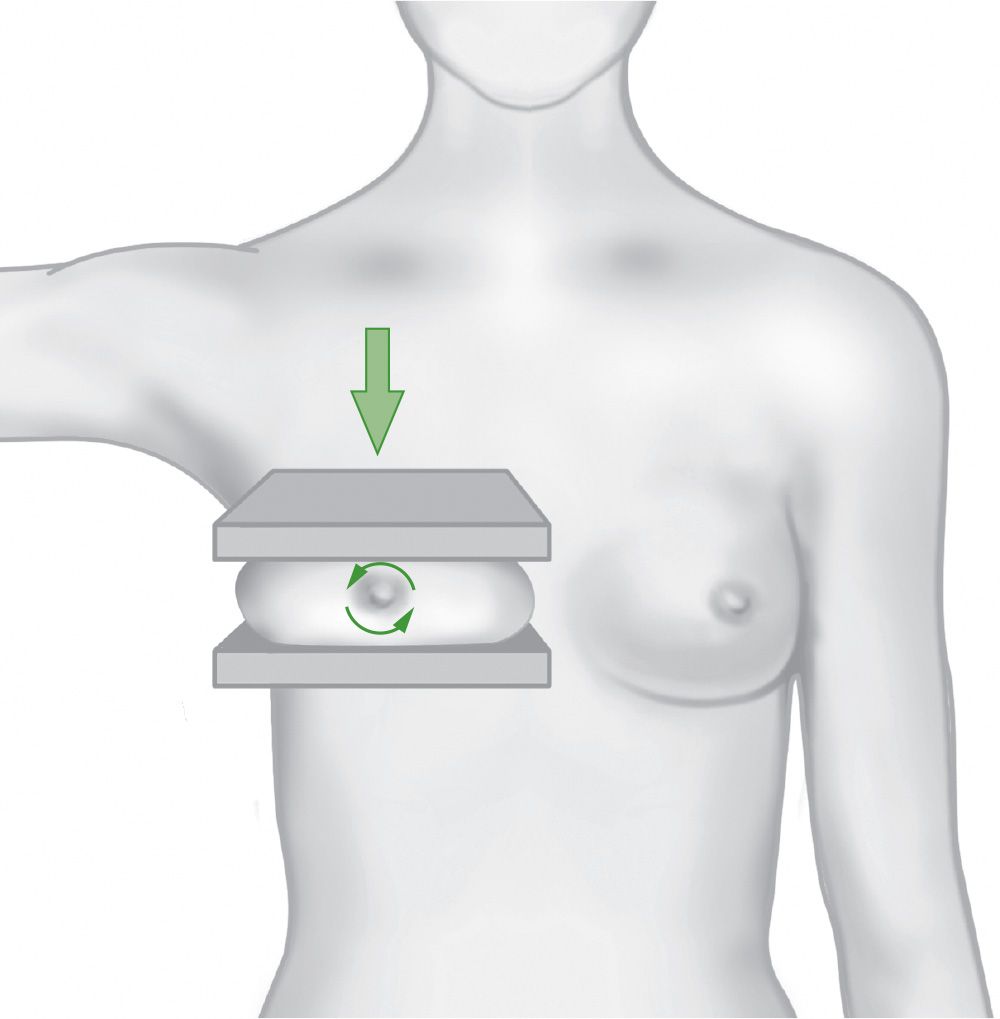
Figure 4-5. (Reproduced with permission from Peart O: Mammography and Breast Imaging PREP: Program Review and Exam Prep. New York, NY: McGraw-Hill Education; 2012.)
45. Which projection is especially useful when analyzing calcifications?
(A) RM
(B) M
(C) LM
(D) ML
46. Identify the position shown in Figure 4-6.
(A) RM
(B) CV
(C) RL
(D) MLO
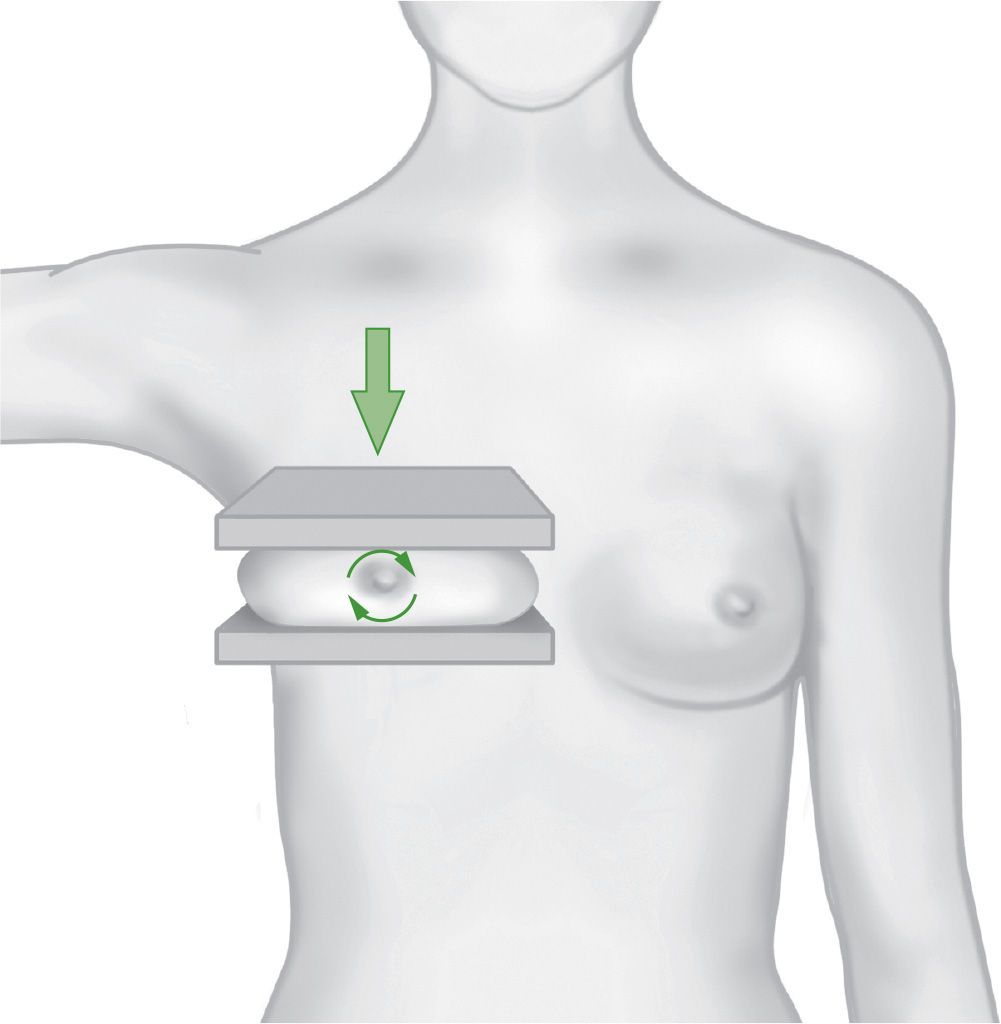
Figure 4-6. (Reproduced with permission from Peart O: Mammographyand Breast Imaging PREP: Program Review and Exam Prep. New York, NY: McGraw-Hill Education; 2012.)
47. All of the following statements about magnification are true except
(A) With magnification, patient dose increases.
(B) Magnification can be used to image specimen radiographs.
(C) Magnification can be used to assess suspicious lesions.
(D) Magnification images the entire breast with 1 exposure.
48. In the RS position, the surface __________ the detector is rolled _______.
(A) furthest from/inferiorly
(B) closest to/superiorly
(C) furthest from/superiorly
(D) closest to/inferiorly
49. Which technique accurately describes how the breast is rolled for the RM?
(A) The superior surface is rolled medially and the inferior surface does not move.
(B) The superior surface is rolled laterally and the inferior surface is rolled medially.
(C) The inferior surface is rolled medially and the superior surface does not move.
(D) The inferior surface is rolled laterally and the superior surface is rolled medially.
50. A patient with pectus excavatum may present a positioning problem because the patient has
(A) extensive pectoral muscle
(B) barrel chest
(C) kyphosis
(D) depressed sternum
51. In imaging the augmented breast in the CC position, using the implant-displaced technique, the breast tissue is pulled/pushed
(A) anteriorly
(B) posteriorly
(C) inferiorly
(D) superiorly
52. A routine series on patients with encapsulated implants could include an additional projection such as the
(A) TAN
(B) CC
(C) MLO
(D) ML
53. Which of the following is used to spread out the tissue and improve resolution on a localized area of interest?
(A) CV
(B) AT
(C) TAN
(D) spot compression
54. How many projections are routinely required to image a patient with implant augmented breasts?
(A) 5
(B) 6
(C) 7
(D) 8
55. When is imaging of the irradiated breast recommended?
(A) immediately after treatment
(B) 1-2 months after treatment
(C) 6-12 months after treatment
(D) 1-2 years after treatment
56. Which of the following projections or positions can be performed with any patient orientation, with or without magnification?
(A) spot compression
(B) XCCL
(C) AT
(D) CV
57. In addition to the routine series, many postlumpectomy patients can also be imaged using the
(A) CC
(B) MLO
(C) ML
(D) CV
58. The “implant in place” projections taken on patients with breast implants requires compression
(A) for immobilization only
(B) to separate the breast tissue
(C) to provide a uniform tissue thickness
(D) for improved spatial resolution
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree