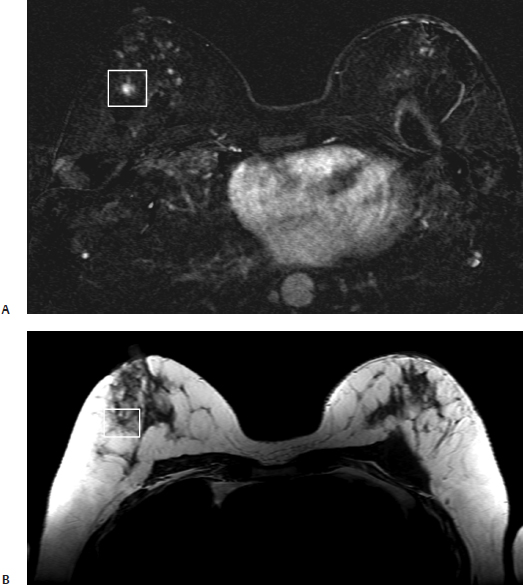
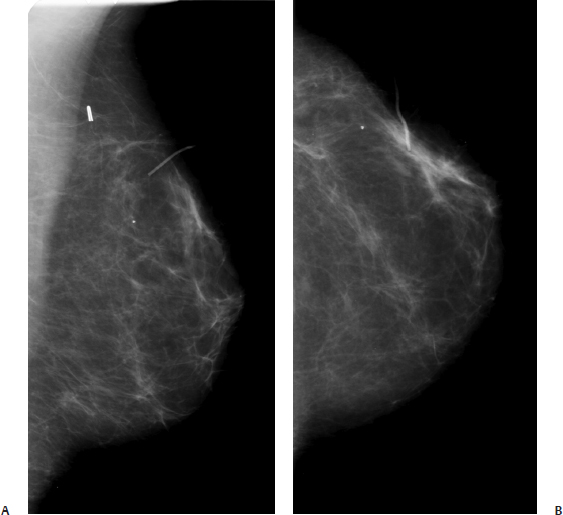
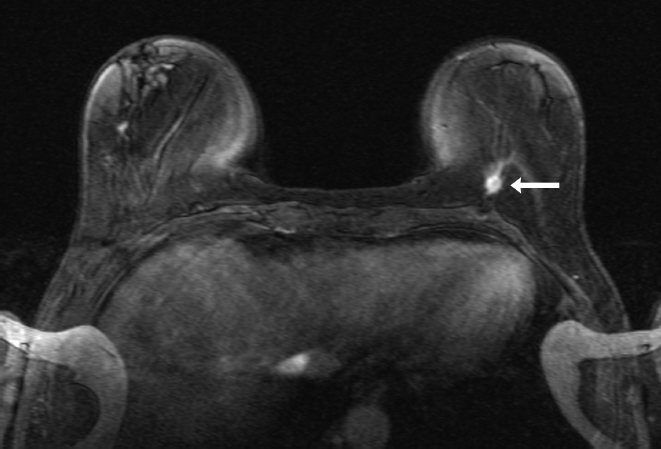
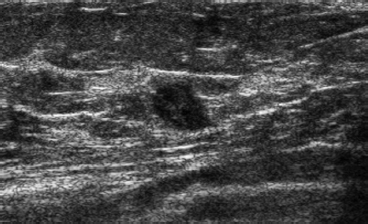
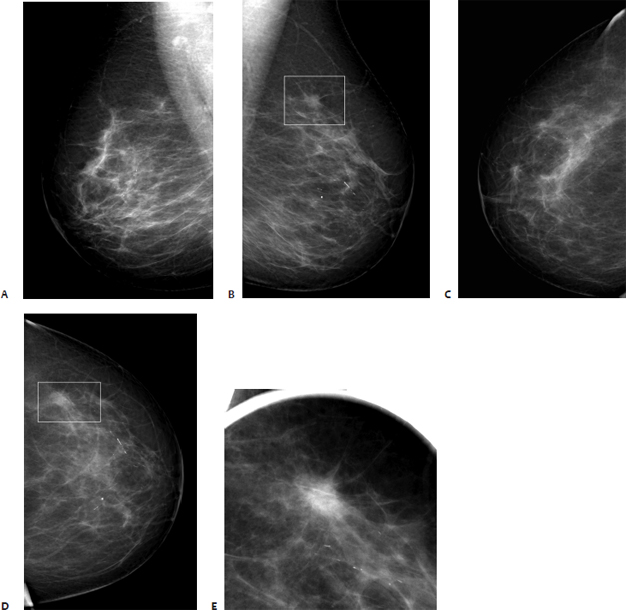
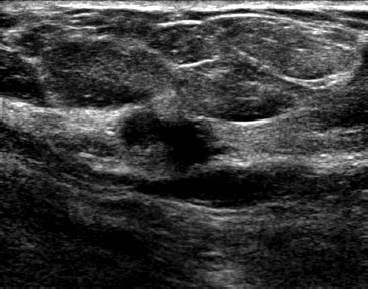
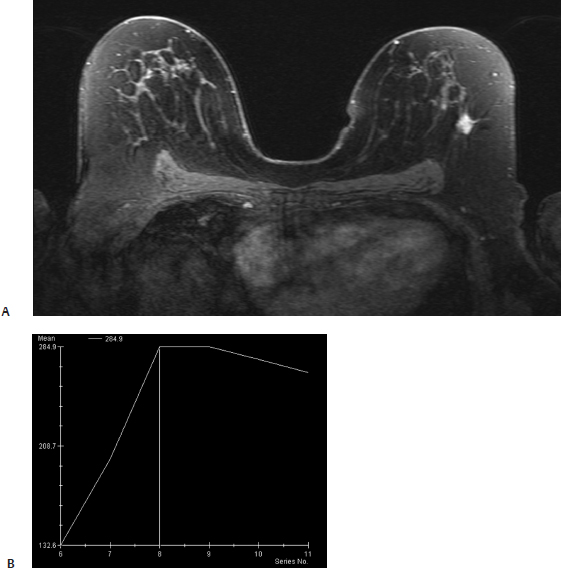
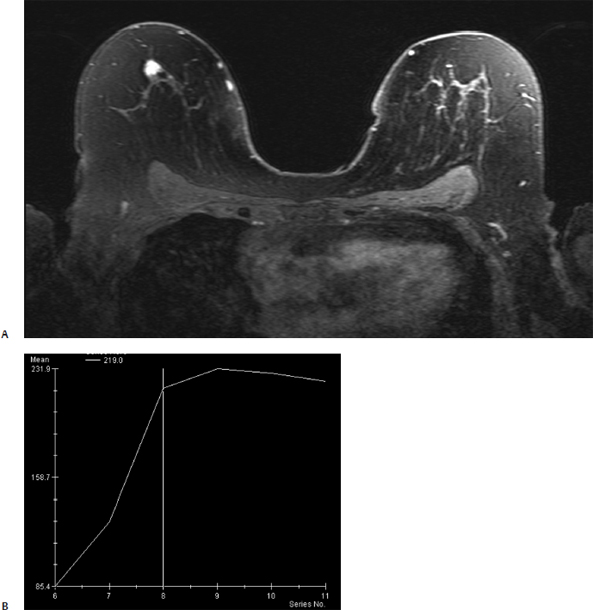
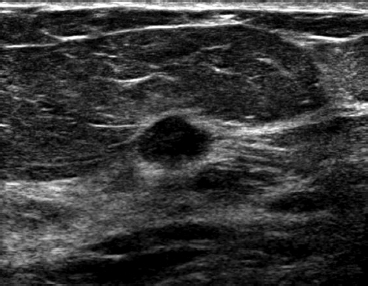
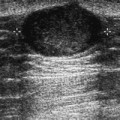
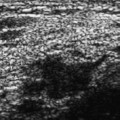
34 Mammographically Occult MRI Lesions A 56-year-old woman, status post–left lumpectomy, which was done at another institution, is seeking a second opinion. Microscopic examination suggests that the margins of the invasive malignancy are close to the surgical margins, so breast MRI is performed. • Left breast: healing lumpectomy site • Right breast: normal Fig. 34.1 After contrast injection, there is no abnormal enhancement associated with the rim of the left lumpectomy cavity. However, in the right upper outer quadrant, there is a 7 mm irregular, rapidly enhancing mass that appears as a spiculated solid mass on the T1 image, which does not have fat suppression (square). (A) Dynamic bolus T1-weighted, 2-minute subtraction axial bilateral breast MRI. (B) T1-weighted axial bilateral breast MRI. • Left breast: reexcision of the lumpectomy cavity; no residual malignancy • Right breast: radial scar • Right MRI enhancing mass: BI-RADS assessment category 4, suspicious; biopsy should be considered. • Radial scars that are surrounded by fat appear as solid spiculated masses on T1-weighted images that are not fat suppressed. With contrast, radial scars exhibit variable enhancement characteristics; they may or may not enhance. If they enhance, then they appear as highly suspicious spiculated masses on T1 fat-suppressed images. Small series do not appear to identify characteristics that differentiate benign radial scars from those associated with malignancy. Therefore, once identified, these lesions should be completely excised. Berg WA. Radial scar. In: Berg WA, Birdwell RL, Gombos EC, Wang S-C, Parkinson BT, Raza S, Green GE, Kennedy A, Kettler MD, eds. Diagnostic Imaging Breast. Altona, Manitoba: Friesens; 2006:IV-2-84-89 Nunes LW, Schnall MD, Orel SG, et al. Correlation of lesion appearance and histologic findings for the nodes of a breast MR imaging interpretation model. Radiographics 1999;19:79–92 Pediconi F, Occhiato R, Venditti F, et al. Radial scars of the breast: contrast-enhanced magnetic resonance mammography appearance. Breast J 2005;11:23–28 A 51-year-old woman presents for screening MRI. She has the BRCA1 gene. She had right breast cancer 14 years prior and left breast cancer 15 years prior. She is status post–bilateral lumpectomy, radiation therapy, and axillary dissections. Her previous breast MRI (1 year prior) and bilateral mammograms (8 months prior) were negative. • Normal exam • Normal exam Fig. 34.2 The patient has a lumpectomy scar in the left upper outer quadrant. (A) Left MLO mammogram. (B) Left CC mammogram. Other Modalities: MRI and Second Look Sonography (Figs. 34.3 and 34.4) Fig. 34.3 Bilateral contrast-enhanced axial breast high-resolution MRI, delayed image. At the 7 o’clock position of the left breast, there is a new enhancing oval mass (arrow). Fig. 34.4 Left radial breast sonogram at the 7 o’clock position. This sonogram was performed as a result of the abnormal screening MRI. There is an oval hypoechoic solid mass, which corresponds to the screening MRI mass. • Infiltrating ductal carcinoma, grade 3 • Left breast MRI enhancing mass: BI-RADS assessment category 4, suspicious; biopsy should be considered. • BRCA1 and BRCA2, genes that normally suppress cell growth, are on chromosomes 17 and 13, respectively. Patients with mutated BRCA1 and BRCA2 genes have a higher risk of breast, ovarian, and prostate cancer. The prevalence of BRCA1 in women with breast cancer is 5.3% in patients younger than 40 years, 2.2% between ages 40 and 49 years, and 1.1% between ages 50 and 70 years. The lifetime risk of breast cancer in patients with BRCA1 or BRCA2 is 85%. • The American Cancer Society has recommended MRI screening for patients with a lifetime risk greater than 20 to 25%. This recommendation is based on the results of multiple screening studies, which have found that for high-risk women, MRI has a higher sensitivity than mammography (77–100% vs 16–40%). MRI specificities are slightly lower than mammography in this group (81–99% vs 93–99%). Besides women with BRCA1 and BRCA2, women who have received chest radiation therapy treatment for Hodgkin’s disease should also be screened by MRI. Other possible screening candidates are women with increased risk due to strong personal and family history. • Patients with BRCA1 and BRCA2 have a greater risk of high-grade carcinoma, which commonly appears as enhancing oval or lobulated masses on MRI and sonographically simulate complex cysts (oval or lobulated, mildly hy poechoic with increased acoustic transmission) or appear similar to fibroadenomas. Therefore, biopsy should not be deferred if a new sonographic benign-appearing mass is detected in a patient with elevated genetic breast cancer risk. Causer PA, Jong RA, Warner E, et al. Breast cancers detected with imaging screening in the BRCA population: emphasis on MR imaging with histopathologic correlation. Radiographics 2007;27(Suppl 1): S165–S182 Lee JM, Kopans DB, McMahon PM, et al. Breast cancer screening in BRCA1 mutation carriers: effectiveness of MR imaging—Markov Monte Carlo decision analysis. Radiology 2008;246:763–771 Lehman CD, Isaacs C, Schnall MD, et al. Cancer yield of mammography, MR, and US in high-risk women: prospective multi-institution breast cancer screening study. Radiology 2007;244:381–388 Lynch HT, Lemon SJ, Marcus JN, Lehman C, Lynch J, Narod S. Breast cancer genetics: heterogeneity, molecular genetics, syndrome diagnosis, and genetic counseling. In: Bland KI, Copeland EM, eds. The Breast. 2nd ed. Philadelphia: WB Saunders; 1998:370-394 Riedl CC, Ponhold L, Flöry D, et al. Magnetic resonance imaging of the breast improves detection of invasive cancer, preinvasive cancer, and premalignant lesions during surveil-lance of women at high risk for breast cancer. Clin Cancer Res 2007;13): 6144–6152 Saslow D, Boetes C, Burke W, et al. American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin 2007;57:75–89 Schrading S, Kuhl CK. Mammographic, US, and MR imaging phenotypes of familial breast cancer. Radiology 2008;246:58–70 Stavros AT. Ultrasound of solid breast nodules: distinguishing benign from malignant. In: Stavros AT, Breast Ultrasound. Philadelphia: Lippincott Williams & Wilkins; 2004:445-527 Willey SC, Cocilovo C. Screening and follow-up of the patient at high risk for breast cancer. Obstet Gynecol 2007;110:1404–1416 An 81-year-woman presents for screening mammography. • Normal examination Mass (Fig. 34.5) • Margin: spiculated • Shape: irregular • Density: high Fig. 34.5 In the left upper outer quadrant, there is a spiculated mass (square). (A) Right MLO mammogram. (B) Left MLO mammogram. (C) Right CC mammogram. (D) Left CC mammogram. (E) Left CC spot compression mammogram. Frequency (Fig. 34.6) • 14 MHz Fig. 34.6 Left radial sonogram. In the upper outer quadrant, there is a solid, hypoechoic, irregular solid mass with a hyperechoic haze and spiculations, which corresponds to the left mammographic spiculated mass. Other Modalities: MRI and Second Look Sonography (Figs. 34.7, 34.8, and 34.9) Fig. 34.7 The left mammographic mass corresponds to a homogeneous irregular spiculated mass that exhibits fast initial enhancement that peaks at 2 to 3 minutes, then exhibits washout (type III kinetic curve). (A) Bilateral contrast-enhanced axial breast high-resolution MRI. (B) Signal-intensity time curve of the left MRI mass. Fig. 34.8 In the right upper outer quadrant, there is an oval mass with irregular margins and homogeneous enhancement. This mass exhibits fast initial enhancement with a plateau curve in the later contrast phases (type II kinetic curve). (A) Bilateral contrast-enhanced axial breast high-resolution MRI. (B) Signal-intensity time curve of the right MRI mass. Fig. 34.9 Right radial sonogram. This sonogram is performed to identify the MRI mass for sonographic biopsy. In the upper outer quadrant, there is a hypoechoic oval mass with a hyperechoic haze and spiculations, which corresponds to the right breast MRI mass. This mass was not identified mammographically. • Left breast: invasive lobular carcinoma • Right breast: invasive ductal carcinoma, grade 1 • Left mammographic and sonographic mass: BI-RADS assessment category 5, highly suggestive of malignancy • Right MRI and sonographic mass: BI-RADS assessment category 5, highly suggestive of malignancy • Besides morphology, enhancement kinetics may be helpful in characterizing a mass. There are three types of kinetic curves. Type I curves exhibit continuous increasing enhancement with time. Type II curves reach maximum signal intensity approximately 2 to 3 minutes after injection, then plateau and remain constant. Type III curves reach a maximum enhancement after 2 to 3 minutes, then rapidly decrease in signal. This decrease in signal is called “washout.” In general, type I curves are associated with benign lesions. Malignant lesions are associated with type II and type III curves.
Case 34.1: Benign MRI Mass
Case History
Physical Examination
Other Modalities: MRI (Fig. 34.1)
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 34.2: Malignant MRI Mass
Case History
Physical Examination
Mammogram (Fig. 34.2)
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 34.3: Malignant MRI Mass
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine