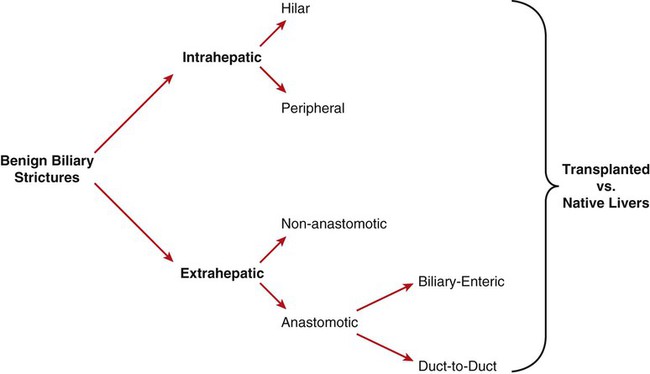
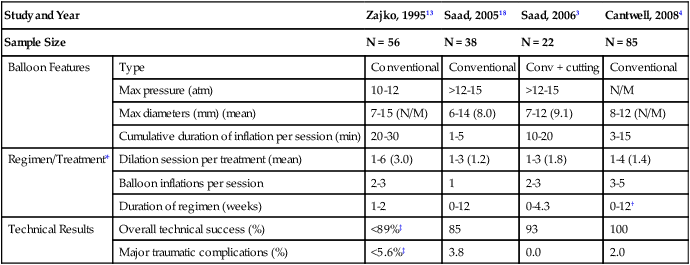
Management of benign biliary strictures (whether surgical, percutaneous-transhepatic, or by endoscopic means) is difficult.1–4 These lesions are formed of cicatricial fibrosis and are recalcitrant to many minimally invasive techniques.1–3 They can be a contributing factor to recurrent cholangitis, hepatic segmental atrophy, hepatic graft dysfunction (in cases of transplanted livers), and in the long-run, obstructive biliary cirrhosis.2–4 Benign biliary strictures are a heterogenous group of lesions that differ in demographics (patient types), locations within the biliary tract, etiology, and disease process (pathology). Firstly, there are pediatric transplant recipients, adult transplant recipients, and adult non-transplant patients with native livers. Pediatric transplant recipients have smaller ducts than adults (transplanted or native livers), and transplant recipients (pediatric or adults) have transplanted livers that have a relatively compromised arterial supply compared to most patients with native livers (see Outcomes for relevance). Secondly, they vary in morphology and location (Fig. 135-1). Thirdly, they vary in etiology and pathogenesis, including inflammatory processes, infectious processes, inflammatory-ischemic processes, thermal injuries from laparoscopic complications, surgical-technical complications at surgical anastomoses (scarring), and (less commonly) radiation injury.1,5–11 Many key studies amalgamate disease processes, and/or transplant versus non-transplants, and/or stricture locations (peripheral vs. anastomotic), and/or types of anastomoses (duct-to-duct vs. biliary-enteric anastomoses (see Fig. 135-1).4,12–13 As a result, it is difficult to discuss anatomic and functional (clinical) outcomes specific to a uniform population or a particular pathologic-anatomic biliary stricture. Indications include cholangitis with or without biliary stones, biliary stones, cholestasis with pruritus, abnormal liver function tests with concern for developing biliary cirrhosis, and hepatic graft dysfunction. The most definitive treatment of central strictures is a hepaticojejunostomy.4,14–16 However, redo hepaticojejunostomies have a lower clinical success rate.4,17 Difficult hepaticojejunostomy candidates (candidates for percutaneous or endoscopic management) include poor surgical candidates owing to comorbidities, patients refusing surgery, numerous adhesions and inflammatory process in the porta hepatis, and short biliary stumps in patients with preexisting hepaticojejunostomies.4 This includes standard internal-external as well as external PTBDs to establish and maintain percutaneous transhepatic access to the biliary tract. Small-caliber, high-pressure (>12 atm), noncompliant balloons are used. The balloon is sized 100% to 110% of the target biliary duct and probably does not exceed 5 to 6 mm.2,13 Remember that right or left main bile duct (hilar) strictures are included in central benign biliary strictures (see later). This includes standard internal-external as well as external PTBDs to establish and maintain percutaneous transhepatic access to the biliary tract. High-pressure (>12 atm) noncompliant balloons are used. The balloon is sized 100% to 125% of the target biliary duct and usually ranges from 6 to 15 mm (Table 135-1).2–3,13,18 Pediatric and adult split-graft transplant recipients usually require smaller balloons (6-10 mm) compared to whole grafts or native livers (7-15 mm).2 TABLE-135-1 ‡Overall technical success rate and complication rates by Zajko et al. amalgamated intrahepatic peripheral lesion dilation and extrahepatic anastomotic dilations. Modified from Saad WEA. Percutaneous management of postoperative anastomotic biliary strictures. Tech Vasc Interv Radiol 2008;11:143–53. Unconventional balloons that have been used include the cutting balloon (Boston Scientific, Natick, Mass.). This is a noncompliant balloon with four microsurgical blades (atherotomes) mounted longitudinally along the outer surface of the balloon. The atherotomes are 1.5 to 2.0 centimeters in length and are 0.127 in depth for all balloon sizes.3 The cutting balloon comes in diameters from 5 to 8 mm and requires use of a coaxial 0.018-inch wire. The 7- and 8-mm diameters require a 7F introducer sheath.3 A drawback is that available diameters of this balloon are limited; 40% of lesions have been found to require balloon sizes greater than 8 mm, which are not available for cutting balloons.3 The PolarCath (for cryoplasty) from Boston Scientific has been mentioned as a potential tool for managing benign biliary strictures,2–3 but to the best of our knowledge, its use has not been published. Covered stents (stent-grafts) can also be used.19 There are two commercially available stent-grafts that can be placed percutaneously or endoscopically but are mostly removed by endoscopic means. However, they can be removed transhepatically, but not by design. These two stents-grafts are the VIABIL (W.L. Gore & Associates, Flagstaff, Ariz.) and the WallFlex (Boston Scientific). The primary step of percutaneous transhepatic management of benign biliary strictures is establishing transhepatic access by an initial percutaneous transhepatic cholangiogram (PTC) followed by PTBD placement.20 The details of the procedure(s) required for access will not be discussed in this chapter. Only the focus of transhepatic management is described. The traditional school has an admirable thought process, but it has two problems. The first is the high patient morbidity (patient discomfort) of a chronically indwelling large drain in patients who are otherwise healthy and active.2–4
Management of Benign Biliary Strictures
Introduction
Indications
Peripheral Intrahepatic Benign Biliary Strictures
Central Benign Biliary Strictures (Anastomotic and Nonanastomotic)
Equipment
Peripheral Intrahepatic Benign Biliary Strictures
Central Benign Biliary Strictures (Anastomotic and Non-anastomotic)
Study and Year
Zajko, 199513
Saad, 200518
Saad, 20063
Cantwell, 20084
Sample Size
N = 56
N = 38
N = 22
N = 85
Balloon Features
Type
Conventional
Conventional
Conv + cutting
Conventional
Max pressure (atm)
10-12
>12-15
>12-15
N/M
Max diameters (mm) (mean)
7-15 (N/M)
6-14 (8.0)
7-12 (9.1)
8-12 (N/M)
Cumulative duration of inflation per session (min)
20-30
1-5
10-20
3-15
Regimen/Treatment*
Dilation session per treatment (mean)
1-6 (3.0)
1-3 (1.2)
1-3 (1.8)
1-4 (1.4)
Balloon inflations per session
2-3
1
2-3
3-5
Duration of regimen (weeks)
1-2
0-12
0-4.3
0-12†
Technical Results
Overall technical success (%)
<89%‡
85
93
100
Major traumatic complications (%)
<5.6%‡
3.8
0.0
2.0
Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine