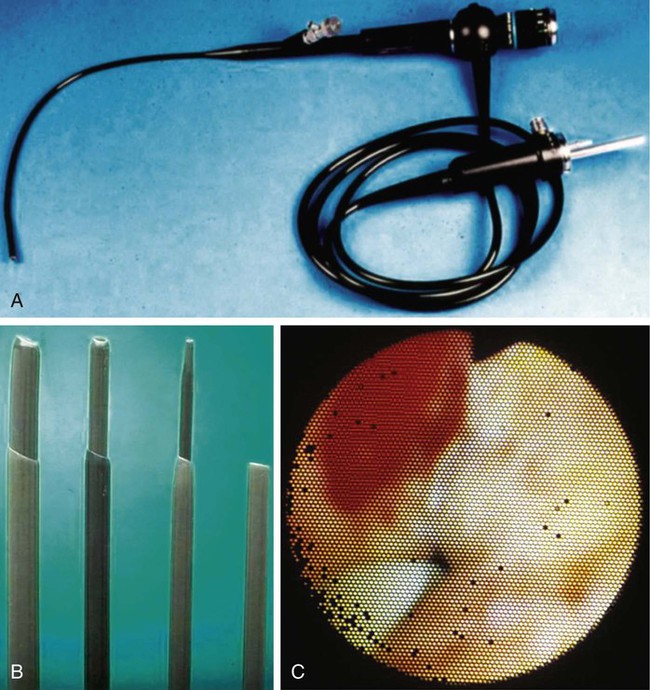
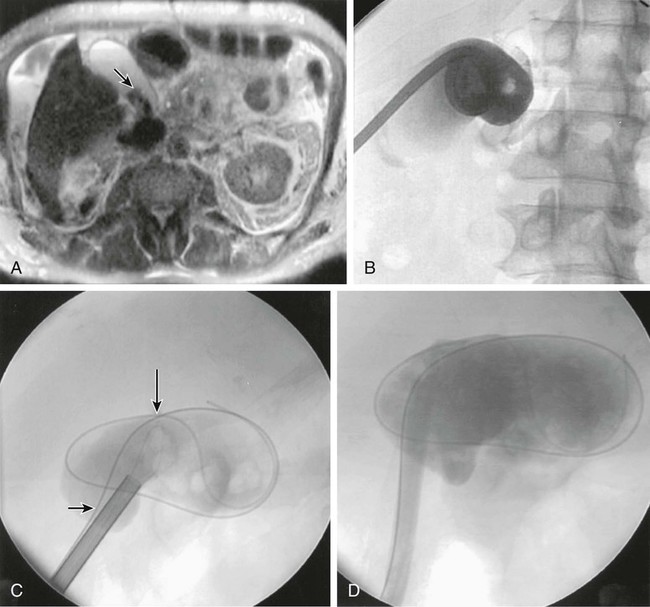
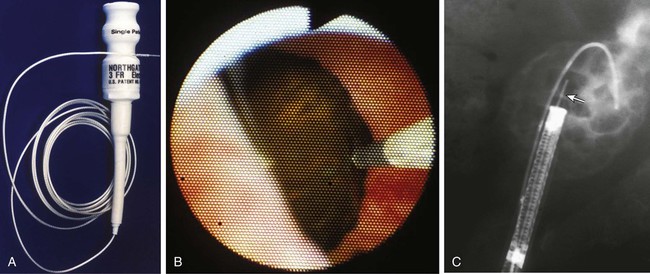
Symptomatic gallstones affect 260,000 Americans every year.1 The majority of patients are treated definitively with surgery, and with the advent of laparoscopic cholecystectomy, surgeons can treat patients less invasively and allow for a quicker recovery. Even in the setting of laparoscopic cholecystectomy, significant medical comorbidities will make some patients unsuitable candidates for surgery. This group can greatly benefit from percutaneous drainage and staged stone extraction. Patients with symptomatic gallstones often simultaneously have calculi in the intrahepatic or extrahepatic bile ducts. Endoscopic retrograde cholangiopancreatography (ERCP) is the principle technique to clear these stones in the majority of patients.2 However, in patients with challenging anatomy (duodenal diverticulum, impacted stones > 15 mm), endoscopic techniques are more prone to failure. Finally, patients who have undergone previous biliary reconstruction as part of a Billroth II or Roux-en-Y anastomosis may be inaccessible via endoscopy, and intrahepatic calculi in these patients may require percutaneous removal. The primary absolute contraindication is the presence of an uncorrectable coagulopathy; bleeding complications are a significant source of morbidity when using large-bore percutaneous transhepatic tracts. Relative contraindications include a nondistensible gallbladder and the presence of active infection. Gallstone extraction can be challenging if not impossible in a chronically diseased, contracted gallbladder. Lack of distensibility can limit needle access and tract dilation. In patients with active infection related to stone disease, appropriate drainage catheter(s) must be placed, with a “cooling off” period to limit septicemia during or following stone extraction. One author has reported successful treatment of a patient with unrelenting fevers secondary to an infected stone burden.3 Only clearance of the stones allowed this patient’s fever to clear. In the majority of patients, drainage and appropriate antibiotics for 24 to 48 hours will allow recovery to perform stone extraction. To perform stone removal, we use a 15F flexible choledochoscope (model CHF-4B [Olympus, New Hyde Park, N.Y.]) (Fig. 138-1, A). The scope contains a working channel that allows use of standard instruments measuring up to 5F in diameter, including graspers and baskets. The existing tube tract is dilated to 18F with a series of Teflon dilators (Cook Medical, Bloomington, Ind.) (Fig. 138-1, B). The outer Teflon sheath allows easy passage of the choledochoscope into the biliary tree, providing a large-bore access to flush out stone debris during the procedure. The scope is connected to continuous normal saline irrigation during use. A principal advantage of the choledochoscope is that it allows the operator to characterize filling defects identified at cholangiography as stones, mucus, air bubbles, clots, or soft-tissue masses (Fig. 138-1, C). Others have described use of an 11F choledochoscope (URF type P2 [Olympus]). Potential advantages of the smaller device are that it requires a smaller percutaneous access (14F) to use and may pass more easily beyond strictures within the intrahepatic biliary ducts. The working channel of this scope is 3F. Authors using it described use of a coumarin green pulsed dye laser (MDL-1 LaserTripter [Candela Laser, Wayland, Mass.]) to fracture resistant stones. The laser operates at a wavelength of 504 nm, and power output is between 40 and 100 mJ. A downside of this device is a smaller working channel to pass baskets and other tools. Additionally, the laser-based equipment is more costly than EHL. Use of ultrasound lithotripters has been described, but the access required for application is prohibitively large (24F) for most operators and has a small field of view.4 Patients are sedated and given intravenous antibiotics (3.375 g of piperacillin/tazobactam or 3 g ampicillin/sulbactam) prior to the procedure. Some operators may prefer administration of atropine (0.6-1 mg) to limit the potential of a vagal response secondary to gallbladder dilation. Initial access may be either transhepatic or transperitoneal, although the latter approach is more commonly associated with acute pain during catheter placement. The gallbladder may be targeted with any combination of fluoroscopic, computed tomographic (CT), or ultrasonic guidance. Optimally the route of entry will be at the end of the gallbladder fundus to simplify reaching calculi with the EHL probe and to ease clearance of the entire lumen of calculi with baskets. Via the Seldinger technique, a 10F to 14F retention loop catheter is placed (Fig. 138-2). In patients with chronic cholecystitis, tract dilation and stone extraction is performed the following day. Patients who have drains placed for acute cholecystitis should recover from their presenting symptoms prior to stone removal. A safety wire is left in the gallbladder lumen outside the 18F working access. In cases where tract dilation is difficult, removable T-tac fasteners are available.5 Stones too large to remove via the sheath and resistant to basket fragmentation can be broken up with the EHL probe. Important factors to consider when using EHL are that the probe has to be 1 to 2 mm beyond the tip of the scope to avoid damaging the choledochoscope (Fig. 138-3). The probe has to be in direct contact with the stone and not the gallbladder wall. Activation of the EHL probe while in contact with the biliary endothelium can lead to bleeding or bile leakage that will make visualization difficult for the remainder of the case. When the operator believes all stones have been removed, final choledochoscopy is performed to ensure no residual stones remain. Contrast cholangiography is performed to evaluate the cystic and biliary ducts. Calculi are identified in cystic and biliary ducts 28% and 24% of the time, respectively.6 Stones in these structures are removed via the gallbladder access if possible or by ERCP if necessary. Calculi in the cystic duct are often impossible to ensnare in a basket or treat with EHL. We have found that leaving an internal-external biliary drain through the gallbladder and cystic duct into the common bile duct and duodenum will usually passively fragment the stones and allow them to pass into the duodenum or out the cholecystostomy catheter. At the end of the procedure, a retention loop catheter is again left in the gallbladder (14F-16F). A large-bore catheter is left in place to tamponade the tract used for endoscopy and allow drainage of any residual “gravel” from calculus fragmentation. The catheter is left to gravity drainage.
Management of Biliary Calculi
Clinical Relevance
Contraindications
Equipment
Technique
Percutaneous Cholecystolithotomy
Management of Biliary Calculi