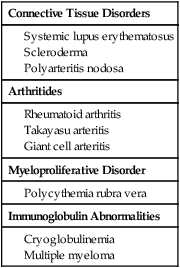
Noninvasive imaging, including duplex sonography, computed tomography (CT) and magnetic resonance imaging (MRI), are used for diagnosis and detection of disease activity. High-resolution B-mode ultrasound can detect intima media thickness (IMT) with or without obstructive stenosis. Increased IMT may suggest presence of active disease.1 Maeda et al. reported circumferential arterial wall thickening of the common carotid arteries, which may or may not be bilateral.2 MRI and CT have both been used to demonstrate arterial wall thickness. Noncontrast CT scans may show a high-density wall of variable thickness in the aorta or its branches, along with calcification if present. CT post contrast may show enhancement of the thickened aortic wall in patients with active inflammation.3 MRI shows subtle wall thickening, and T2-weighted images may show bright signal due to edema in the inflamed vessel. During the acute phase, enhancement of the aortic wall and peri-adventitious soft tissues can also be observed.4 It has been suggested that contrast-enhanced MRI may be more sensitive than serologic markers of clinical activity in this disease. Overall, these MR criteria are not highly sensitive but are highly specific for disease activity. We have observed that the sensitivity of T2-weighted imaging in detecting active disease seems inferior to contrast-enhanced T1-weighted imaging. Aortic wall thickness by itself may also reflect disease activity.5 Most of our patients with inactive disease had a wall thickness of less than 4 mm, and most of them with acute or chronic active disease had a wall thickness greater than 5 mm. The differential diagnosis includes a variety of conditions that can cause vasculitis. These are summarized in Table 42-1. TABLE 42-1 Potential Underlying Systemic Illnesses in Upper Limb Arterial Disease Renovascular hypertension (RVH) is the most common form of treatable clinical presentation of this disease. It is usually due to obstructing lesions involving the aorta and renal arteries.6,7 Takayasu disease is a common cause of RVH in India. Chugh et al.8 studied the causes of RVH in India and reported that nonspecific aortoarteritis was responsible for 61%, fibromuscular dysplasia (FMD) for 28%, and atherosclerosis for 8% of cases. Some form of revascularization is necessary to relieve ischemia secondary to a hemodynamically significant stenosis. The complexity of pathologic changes in the wall of the aorta and the widespread nature of involvement make surgical revascularization difficult. There is also a high prevalence of graft occlusion or aneurysm formation at the treatment site.9–11 Because of this, nonsurgical revascularization techniques have been increasingly used to treat this disease.6,7,12–22 Percutaneous transluminal angioplasty (PTA) for treatment of aortic stenosis in the presence of nonspecific aortitis has been infrequently reported.7,17,23 In these patients, the angiographic morphology of 140 stenoses has been correlated with the outcome of balloon angioplasty. Patients with short-segment (<4 cm) stenosis show better overall results than those with long-segment (>4 cm) stenosis. The angiographic features, including eccentricity of the stenosis and presence of diffuse adjacent disease, location of the stenosis in the juxtadiaphragmatic segment of the aorta, and presence of calcification adversely affect the outcome of PTA, with most patients developing large intimal flaps. Such patients should be electively treated by stent placement. Stents have also been used as a “bailout” measure in salvaging an obstructive dissection.22,23 Our results show that stents provide immediate relief of symptomatic obstructive dissection and are also useful to treat recurrent stenosis after successful angioplasty. Except for the situations just mentioned, we do not advocate elective use of stents because of the young age of patients, cost involved, and lack of knowledge about the long-term behavior of stents in the aorta at a growing age. Various methods have been used to identify active disease. Constitutional signs and symptoms include fever, anorexia, arthralgia, limb ischemia, hypertension, and raised ESR. These acute-phase features may be present in 50% of patients. The other 50% of patients present with advanced obstructive changes with no acute-phase symptoms. Surgical biopsy specimens from patients with clinically inactive disease showed histologically active disease in as many as 44%.24 From a study in 1998, researchers concluded that no known serologic test could supplant vascular histopathologic examination in determining disease activity. Similarly, 61% of patients with remitting disease showed new lesions on angiography, emphasizing the need for more reliable and accurate markers for disease activity. The National Institutes of Health describes “active” disease as fresh onset or progression of at least two of the following features25: • Signs and symptoms of vasculitis or ischemia (claudication, feeble or absent pulses, differential blood pressure in extremities, bruits, or carotidynia) • Systemic symptoms such as fever, polyarthralgia, or polymyalgia A study by the International Network for the Study of the Systemic Vasculitides (INSSYS) enlisted 29 patients with Takayasu arteritis and 26 healthy controls. Activity was assessed based on Birmingham vasculitis activity scores.26 Serologic tests including ESR, C-reactive protein, tissue factor, von Willebrand factor, thrombomodulin, tissue plasminogen activator (tPA), intercellular adhesion molecule-1, vascular cell adhesion molecule-1, E-selectin, and platelet endothelial cell adhesion molecule-1 were performed on all patients but could not reliably differentiate between healthy volunteers and patients with Takayasu arteritis. Clinical and biochemical markers remain poor predictors of clinical activity, but patients with an elevated ESR and/or positive C-reactive protein test are considered to have active arteritis and are not accepted for this treatment. Standard angioplasty techniques are employed. • Arterial sheath: for placement in both femoral arteries • Pigtail catheter: to be placed in the abdominal aorta above the origin of the renal arteries for continuous pressure measurement and diagnostic digital subtraction angiography • Selective angiographic catheter: for transstenotic gradient measurement It has been traditionally reported that nonspecific aortoarteritis involves all layers of the vessel wall.27,28 Histopathologic findings are characterized by inflammatory changes, with marked tissue destruction and connective tissue proliferation initiated at the junction of the media and adventitia or the outer layer of the media. There is an endarteritis obliterans or onion skin–type fibrosis in the vasa vasorum. Thickening of the intima results from an increase in ground substance and proliferation of connective tissue.27–30 Underlying chronic inflammation, extensive periarterial fibrosis, thickening, and adhesions combine to produce tough, noncompliant, rigid vessel walls. The morphologic pattern of involvement in Takayasu disease shows racial and geographic differences.31 In Japan, thoracic aortic involvement is more common, and neck vessels are most often involved.28 In most other Asian countries, the abdominal aorta is most frequently affected, with the renal and subclavian arteries being the most commonly involved branches.32 Although pulmonary artery involvement is common in most studies, among Indian patients it is less frequent. In a prospective study, we found pulmonary arterial involvement in 14.9% of patients.33 Reports of familial incidence of Takayasu arteritis may point to a genetic origin. In Japan, 16 families with familial Takayasu arteritis have been reported.34 In India, Mehra et al.35 studied 104 patients and suggested an association of this disease with human immune response genes, namely HLA-B5 and its serologic subtypes B51 and B52. In HLA B52–positive patients, aortic regurgitation, ischemic heart disease, and pulmonary infarction are more common. Renal artery stenosis is reported more frequently in HLA B39–positive patients. The human leukocyte antigen association is thought by some to strengthen the argument in favor of an autoimmune pathogenesis. However, no specific autoantigens have been identified, and for any adaptive immune response to occur, whether against exogenous or endogenous antigen, presentation of antigen to T cells in the context of the major histocompatibility complex is central. The predominant involvement of females has prompted investigators to study the role of sex hormones. In one study, urinary estrogens were elevated in 80% (16 of 20) of patients, compared with healthy controls.36 In most studies that have evaluated the angiographic morphology, obstructive lesions predominate.27,28,32,37 When present, aneurysmal lesions also show distinct geographic predilections. There is a disproportionately high incidence of these lesions in the Philippines, Thailand, Israel, Japan, and Western India.38,39
Management of Vascular Arteritides
Imaging
Connective Tissue Disorders
Arthritides
Myeloproliferative Disorder
Immunoglobulin Abnormalities
Indications
Contraindications
Equipment
Technique
Anatomy and Approaches
Controversies
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine






