Presentation and Presenting Images
( ▶ Fig. 37.1, ▶ Fig. 37.2, ▶ Fig. 37.3, ▶ Fig. 37.4, ▶ Fig. 37.5, ▶ Fig. 37.6, ▶ Fig. 37.7)
A 36-year-old female with a strong family history of breast cancer presents for high-risk screening mammography.
37.2 Key Images
( ▶ Fig. 37.8, ▶ Fig. 37.9, ▶ Fig. 37.10, ▶ Fig. 37.11, ▶ Fig. 37.12, ▶ Fig. 37.13)
37.2.1 Breast Tissue Density
There are scattered areas of fibroglandular density
37.2.2 Imaging Findings
There is a 1.3-cm oval mass (circle in ▶ Fig. 37.8 and ▶ Fig. 37.9) in the retroareolar region of the right breast. Additionally, there is 1.5-cm asymmetry located 9 cm from the nipple in the inferior aspect of the left breast, seen only on the mediolateral oblique (MLO) view (box in ▶ Fig. 37.10).
The right craniocaudal (RCC) views ( ▶ Fig. 37.8 and ▶ Fig. 37.5, conventional mammogram and tomosynthesis movie , respectively) are ill-positioned with the nipple not in profile. On these views, it is easy to mistake the mass (circle) for the nipple (arrow) ( ▶ Fig. 37.8). Only the conventional imaging was repeated, to reduce the amount of radiation exposure ( ▶ Fig. 37.11).
The left breast asymmetry does not persist on tomosynthesis. The right breast mass is demonstrated on tomosynthesis ( ▶ Fig. 37.12 and ▶ Fig. 37.13) as a well-circumscribed mass in the retroareolar region. Ultrasound is recommended for further evaluation.
37.3 BI-RADS Classification and Action
Category 0: Mammography: Incomplete. Need additional imaging evaluation and/or prior mammograms for comparison.
37.4 Diagnostic Images
( ▶ Fig. 37.14, ▶ Fig. 37.15, ▶ Fig. 37.16, ▶ Fig. 37.17)
37.4.1 Imaging Findings
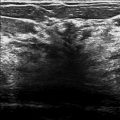
Ultrasound of the right breast reveals a well-circumscribed oval hypoechoic mass in the retroareolar region ( ▶ Fig. 37.16 and ▶ Fig. 37.17) that corresponds to the mammographic and tomosynthesis findings.
37.5 BI-RADS Classification and Action
Category 2: Benign
37.6 Differential Diagnosis
Fibroadenoma: Cystic and solid masses may have the same appearance on mammography. Sonography can reliably differentiate between cystic and solid masses. This is a solid, well-circumscribed oval hypoechoic mass on ultrasound.
Cyst: This mass does not have the sonographic characteristics of a cyst.
Breast cancer (invasive ductal carcinoma [IDC]): High-grade carcinomas and medullary carcinomas can mimic complicated cysts. These carcinomas may be markedly hypoechoic and have a round shape.
37.7 Essential Facts
Cystic and solid masses may have the same appearance on mammography, but sonography can reliably differentiate between cystic and solid masses.
Sonography may be used to guide a biopsy of indeterminate and suspicious lesions. If ultrasound had not identified this mass and biopsy was deemed necessary, tomosynthesis-directed stereotactic biopsy could also have been performed.
Fibroadenomas are very common benign masses. Options for diagnosis are image-guided biopsy, excision, or sequential follow-up imaging that demonstrates stability for 2 years. Any lesion that is being followed must adhere to strict criteria and not have a positive predictive value (PPV) greater than 2%, thus not satisfying the BIRADS 3 assessment category.
37.8 Management and Digital Breast Tomosynthesis Principles
Tomosynthesis is not just helpful in finding abnormalities in patients with denser breast tissue but also in patients with scattered breast parenchyma.
The detection of lesions obscured by overlapping breast tissue is a limitation of conventional mammography. Imagers may have difficulty identifying abnormalities. In some cases, lesions may go undetected.
Tomosynthesis helps imagers to identify true mass lesions and to dismiss pseudomasses or summation artifacts.
Radiologists must avoid dismissing well-circumscribed masses as benign. Additional studies evaluating circumscribed cancers on tomosynthesis need to be performed to identify commonalities among these malignant lesions that would help with their identification as malignant.
Positioning is just as important on tomosynthesis as it is on conventional mammography. The first RCC view in this case (conventional mammogram and tomosynthesis movie) is ill-positioned with the nipple not in profile. In fact, this view is more of a right laterally exaggerated craniocaudal (XCCL) view than a CC view. The mass (circle) could have been mistaken for the nipple (arrow). Only the conventional imaging was repeated to reduce the amount of radiation exposure.
37.9 Further Reading
[1] Rafferty EA, Park JM, Philpotts LE, et al. Assessing radiologist performance using combined digital mammography and breast tomosynthesis compared with digital mammography alone: results of a multicenter, multireader trial. Radiology. 2013; 266(1): 104‐113 PubMed
[2] Rose SL, Tidwell AL, Bujnoch LJ, Kushwaha AC, Nordmann AS, Sexton RJr. Implementation of breast tomosynthesis in a routine screening practice: an observational study. AJR Am J Roentgenol. 2013; 200(6): 1401‐1408 PubMed

Fig. 37.1 Right craniocaudal (RCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree