Presentation and Presenting Images
A 43-year-old female presents for screening mammography.
31.2 Key Image
( ▶ Fig. 31.3)
31.2.1 Breast Tissue Density
There are scattered areas of fibroglandular density.
31.2.2 Imaging Findings
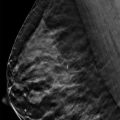
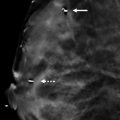
In the posterior and lateral region of the left breast on the craniocaudal (CC) view ( ▶ Fig. 31.1), there is an oval mass. This is confirmed on the digital breast tomosynthesis (DBT) images, as seen on slice 1 of the DBT images ( ▶ Fig. 31.3). The DBT images are oriented from superior to inferior; thus, the mass is located in the upper outer quadrant of the left breast. A correlate is not seen on the mediolateral oblique (MLO) mammogram ( ▶ Fig. 31.2) or MLO DBT image (not shown).
31.3 BI-RADS Classification and Action
Category 0: Mammography: Incomplete. Need additional imaging evaluation and/or prior mammograms for comparison.
31.4 Diagnostic Images
( ▶ Fig. 31.4, ▶ Fig. 31.5, ▶ Fig. 31.6)
31.4.1 Imaging Findings
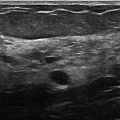
The diagnostic imaging demonstrates not one but two masses in the posterior depth of the upper outer quadrant ( ▶ Fig. 31.4 and ▶ Fig. 31.5). To see these masses on the MLO view ( ▶ Fig. 31.5), more lateral tissue of the breast was included. For this reason, the nipple is not seen in profile given it was rolled medially. The images confirm that the circumscribed masses are located in the left breast at the 1 o’clock location, 11 cm from the nipple. The ultrasound was performed confirming two masses ( ▶ Fig. 31.6). The larger mass is 0.9 cm and the adjacent smaller mass is 0.5 cm in size. Both masses are hypoechoic with central echogenic region.
31.5 BI-RADS Classification and Action
Category 2: Benign
31.6 Differential Diagnosis
Lymph node: By location, a lymph node is the most likely diagnosis. However, the mass does not have the classic appearance to dismiss it as a lymph node on the screening mammogram. The DBT images confirm the circumscribed margins expected of a lymph node but do not offer information about a fatty hilum.
Fibroadenoma: This can present as a circumscribed mass on mammography, however, it often requires an ultrasound to make this diagnosis. The ultrasound in this case does not support this diagnosis.
Carcinoma: Breast cancer can occur anywhere in the breast tissue. At the margins of the breast tissue or at the margins of the image are the most common locations in imaging for missed cancers. The initial imaging could not dismiss this as not being a cancer. The subsequent imaging determined it to be benign and not a cancer.
31.7 Essential Facts
This mass, because it was only seen on the CC view (FFDM and DBT), could be located anywhere along the lateral aspect of the breast. However, the CC DBT image localized the mass to the slice 1. This localizes this mass to the upper outer quadrant.
DBT allows for triangulation of lesions only seen well on one view.
The stack of images from DBT is designated as being head to foot or medial to lateral, depending on whether it is a CC or MLO projection. Once the slice number of the stack that the lesion is located within is identified, then the location in the orthogonal plane can be determined. Knowing where to look in the orthogonal view will further assist in characterizing the lesion.
31.8 Management and Digital Breast Tomosynthesis Principles
DBT triangulation techniques will assist in localizing a lesion prior to a diagnostic ultrasound evaluation. This should improve the success of finding a lesion on ultrasound.
DBT triangulation localization techniques can help determine if a lesion is within the breast parenchyma or within the skin.
Although DBT can aid in localizing a lesion in the orthogonal imaging plane, this does not mean that only one DBT view is needed. Studies have shown that DBT in both the CC and MLO projections yield higher accuracy in localizing lesions.
31.9 Further Reading
[1] Conant EF. Clinical implementation of digital breast tomosynthesis. Radiol Clin North Am. 2014; 52(3): 499‐518 PubMed
[2] Roth RG, Maidment AD, Weinstein SP, Roth SO, Conant EF. Digital breast tomosynthesis: lessons learned from early clinical implementation. Radiographics. 2014; 34(4): E89‐E102 PubMed

Fig. 31.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree