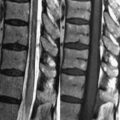
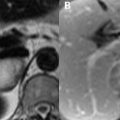
21 Meningitis Clinically, meningitis presents as a combination of headache, nuchal rigidity, fever, and altered mental status. Infections of the meninges are most commonly of hematogenous origin, but may result from trauma, surgery, or the extension of local infections. Bacterial etiologies vary by age: neonates are affected most commonly by Escherichia coli and group B Streptococcus, older children by Neisseria meningitidis, Streptococcus pneumoniae, and type B Haemophilus influenza, and adults by Streptococcus and N. meningitidis. MRI and CT may be performed prior to lumbar puncture to rule out masses and assess for SAH. Nonenhanced MRI is relatively insensitive to the detection of meningitis, particularly aseptic (usually viral) forms, but due to the necessity of early antibiotic treatment, when present, these features must be recognized. An early MRI finding of meningitis is subarachnoid distension, most prominently seen as widening of the interhemispheric fissure and basilar cisterns. FLAIR is the most sensitive nonenhanced sequence, the higher protein content of the subarachnoid space manifesting as high SI compared to the normally low SI CSF. Figure 21.1A demonstrates posterior cortical sulci with normal low SI on FLAIR along with the high SI sulci (black arrow
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree