Fig. 15.1
(a, b) Right perirectal node 3 mm (arrow) with homogeneous signal. (c, d) Right obturator node 9 mm (arrow) with inhomogeneous signal
Fig. 15.2
(a, b) Gleason 4 left base (arrows) and Gleason 5 right base. (c, d) Right periprostatic 3 mm node (arrow). (e, f) Right perirectal node and left obturator nodes (arrow). (g, h) Bilateral vascular obturator nodes (arrows) and bone metastases. (i, j) Bilateral vascular internal iliac nodes (arrows) and bone metastases. (k, l) Bilateral vascular external iliac nodes (arrows) and bone metastases
Fig. 15.3
(a, b) Right perirectal node 6 mm (arrow) with homogeneous signal. (c, d) Left perirectal node 3 mm (arrow); note 2 anterior vessels
Fig. 15.4
(a, b) Left 3 mm perirectal node (arrow)—avascular
Fig. 15.5
(a, b) Left 3 × 5 mm perirectal node (arrow)—vascular
Fig. 15.6
(a, b) Right perirectal vascular node (arrow) from squamous cell carcinoma; note massive rectal invasion
Fig. 15.7
(a, b) Right perirectal node (arrow) with massive rectal invasion. (c, d) Seminal vesicle invasion with left perirectal node (arrow)
Fig. 15.8
(a, b) September 2006 avascular retropubic 4 mm right anterior lymph node in the space of Retzius (arrow). (c, d) Nine-month follow-up (June 2008) retropubic node increased to 6 mm (arrow) with increased perfusion
15.2 Bladder Invasion
The bladder may be involved by direct invasion of cancers in the base of the prostate gland or rarely by hematogenous spread. It is important to verify if the bladder mass is a calculus (attached to the wall or mobile), a blood clot, or a true bladder tumor. Rotation of the patient may demonstrate movement of the lesion confirming a stone or a clot. Stones generally are rounded and a calcific rim or heavy internal microcalculi will often produce a distinct sonic shadow.
Blood clots tend to resolve with time and may have different echo patterns depending on the degree of clot contraction/fibrosis or clot dispersion (Figs. 15.9a, b and 15.10a, b). Rarely, a ureteral tumor will prolapse into the bladder lumen. Oftentimes a dilated ureter or hydronephrosis will be present, entering the base of the prolapsed portion (Figs. 15.11a, b, 15.12a, b, 15.13a, b, 15.14a, b, and 15.15a, b). MRI and 3DPDS may image polypoid lesions 3 mm and larger. Sessile or surface lesions may be missed. This resolution may be used as a screening test for bladder neoplasms that protrude into the lumen. Internal irregularities may be falsely exaggerated with a partially distended bladder.
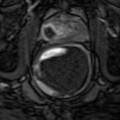
Fig. 15.9
(a) MRI dark oval left stone (arrow). (b) Left bladder stone not imaged on DCE
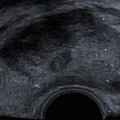
Fig. 15.10
(a) MRI Superior bladder tumor (arrow) R DOME. (b) DCE-MRI enhancing transitional cell carcinoma