Fig. 22.1
(a) Prior to CIRT the CT images show the primary tumor. (b) Tumor shrinkage was shown 20 months after CIRT. (c) The CT and PET images show the pre-tracheal lymph node before CIRT. (d) Twenty months after CIRT, lymph node swelling and the accumulation of C11-met PET appeared
In this case, EBUS-TBNA was performed, and nodal metastasis was proven pathologically. The patient was also treated with C-ion RT for the nodal metastasis using 48.0 GyE in 12 fractions over 3 weeks (Fig. 22.2).
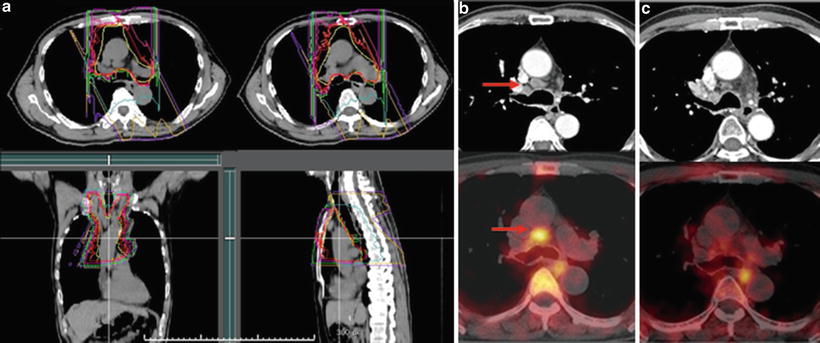
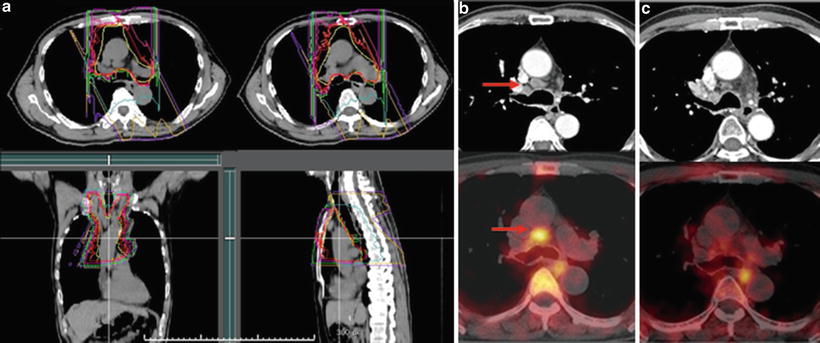
Fig. 22.2
(a) The planning CT for the treatment of the mediastinal and hilar lymph node metastases. (b) The arrow shows the lymph node metastasis. (c) CT and PET images 3 months after CIRT
22.2.3 Results
Thirty-six patients were treated between January 2000 and December 2010. The first therapy for the primary lung cancer was surgery or C-ion RT or conventional radiotherapy, and the number of patient treated using these modalities was 10, 25, and 1, respectively.
The 36 metastatic lesions were treated by carbon ion beam irradiation alone using a total dose of 48.0 GyE in 12 fractions over 3 weeks. The mean age of the patients was 69.7 years (38–87), and the gender breakdown was 16 females and 20 males. By histological type, there were 24 adenocarcinomas, 11 squamous cell carcinomas, and 1 large cell carcinoma.
The statistical 3-year overall survival rate of the 36 patients was 52.9 %, with a median observation period of 13.5 months (range, 2.9–114.8 months). The 3-year local control rate was 100 %. The toxicities to the skin and lungs caused by C-ion RT were assessed according to the NCI-CTC (early) and RTOG/EORTC (late). No adverse events greater than grade 2 were detected among any of these reactions.