This article reviews the features that should prompt consideration of diseases that mimic acquired demyelinating syndromes and multiple sclerosis using vignettes to highlight unusual clinical and radiologic features. Cases of transverse myelitis, spinal infarction, acute disseminated encephalomyelitis, fever-induced refractory epileptic encephalopathy in school-aged children, small-vessel vasculitis, Griscelli syndrome type 2, cysticercosis, vitamin B12 deficiency, and chronic relapsing inflammatory optic neuropathy are presented.
Key points
- •
Demyelination of the optic nerves, spine, and brain may occur as a monophasic or transiently multiphasic illness without chronic relapsing demyelination typical of multiple sclerosis (MS). To date, no biomarker or magnetic resonance (MR) imaging pattern reliably identifies such individuals.
- •
Asymptomatic brain lesions outside of the optic nerve or spinal cord strongly favor MS.
- •
Anterior horn cell involvement can be prominent in both vascular and demyelinating disorders of the spinal cord.
- •
Diffusion restriction can be detected in the spinal cord but it is not pathognomonic for infarction in this region; diffusion restriction within the cord has been reported in transverse myelitis.
- •
Ring enhancement differentials include infections, granulomatous disease and neoplasms, but can be seen in patients with demyelination. Open-ring enhancement is more typical of demyelinating lesions. When open-ring sign is present in the brain, demyelination is much more likely than neoplasm or infection.
Introduction
Acquired demyelinating syndromes (ADS) of the central nervous system (CNS) are characterized by acute neurologic deficits, magnetic resonance (MR) imaging findings of focal or multifocal areas of abnormal signal on T2-weighted images in the brain, optic nerves, or spinal cord, and a response to corticosteroids. The clinical features of ADS relate to the localization of areas of inflammation. Common ADS presentations include optic neuritis (ON), transverse myelitis (TM), brainstem syndromes, polyfocal neurologic deficits, and polyfocal deficits accompanied by encephalopathy (termed acute disseminated encephalomyelitis [ADEM]). For some patients, ADS occurs as a monophasic illness, whereas for others it represents the first clinical manifestation of multiple sclerosis (MS). Table 1 provides a diagnostic evaluation for children suspected of having an acquired demyelinating syndrome or MS.
| The following investigations should be performed, as clinically indicated: | |
| MR imaging | Brain MR imaging in all children Spine MR imaging in all children with clinical spine involvement Orbital MR imaging for children with visual loss The following MR imaging sequences are suggested: FLAIR or T2-weighted sequences in at least 2 planes Pre- and postgadolinium T1-weighted images Diffusion-weighted sequences |
| Evoked potentials | VEPs SSEPs |
| Laboratory screening for NMO and MAS | Serum NMO IgG CSF NMO IgG (if serum negative) Ferritin Triglycerides |
| Infection screening | CBC + differential Serum viral serologies (EBV, mycoplasma, HSV serology) VDRL Lyme disease (seasonal) Cysticercosis (based on travel to endemic areas only) HTLV (based on travel to endemic areas only) |
| Endocrine | TSH, T4, anti-TPO antibodies if Hashimoto encephalopathy is a consideration |
| Mitochondrial lactate serum + CSF | Pyruvate; if higher than normal lactate, calculate lactate to pyruvate ratio DNA studies, skin and muscle biopsy if mitochondrial disease strongly suspected |
| Rheumatologic disease | ESR, CRP ANA, dsDNA Anticardiolipin and antiphospholipid antibodies Angiotensin-converting enzyme CXR (if sarcoidosis is strongly suspected) |
| Nutritional | Vitamin B12 (serum) 25-hydroxyvitamin D (25(OH)D) |
| CSF studies | Glucose Lactate Protein Cell count Culture and sensitivity, Gram stain when appropriate Oligoclonal bands (compared with concurrently obtained serum) a CSF viral cultures + PCR herpesviruses Cytology (if indicated) |
a The accuracy of oligoclonal band measurement depends on the diagnostic test used and on the experience of the laboratory performing the test. Isoelectric focusing has the highest sensitivity.
Although well characterized clinically and radiologically, the clinical features of acute demyelination are not specific. Clinicians must be alert to other neurologic disorders with similar signs. The diagnosis of monophasic ADS and MS requires exclusion of other diagnoses. Table 2 highlights some of the MR imaging features that should prompt clinicians to consider diagnoses other than ADS and MS. This article reviews the features that should prompt consideration of diseases that mimic ADS and MS, using vignettes to highlight unusual clinical and radiologic features.
| MR imaging | Leptomeningeal enhancement | SVcPACNS Infection Tumor HLH | Leptomeningeal enhancement is not a feature of MS in adults, and emerged as a red flag for vasculitic or malignant processes in the pediatric cohort |
| Lesion expansion | Tumor Lymphoma PML Sarcoidosis | Increased size of T2 lesions on serial imaging is well recognized in MS, although this should always prompt consideration of malignancy. Increasing size of a white matter–predominant lesion without lesion enhancement in a patient treated with immunosuppressant therapy (or a patient with known HIV) should prompt consideration of PML. PML is a risk for MS patients exposed to more intense immunosuppressive therapies | |
| Hemorrhage | ANE Stroke Cerebellitis AHLE Large-vessel CNS vasculitis SVcPACNS | Although susceptibility-weighted imaging reveals tiny microfoci of hemosiderin in MS patients, hemorrhage large enough to be visible on conventional MR imaging sequences is not a feature of ADS or MS, and should prompt consideration of disorders in which the cerebral vasculature is specifically involved |
Introduction
Acquired demyelinating syndromes (ADS) of the central nervous system (CNS) are characterized by acute neurologic deficits, magnetic resonance (MR) imaging findings of focal or multifocal areas of abnormal signal on T2-weighted images in the brain, optic nerves, or spinal cord, and a response to corticosteroids. The clinical features of ADS relate to the localization of areas of inflammation. Common ADS presentations include optic neuritis (ON), transverse myelitis (TM), brainstem syndromes, polyfocal neurologic deficits, and polyfocal deficits accompanied by encephalopathy (termed acute disseminated encephalomyelitis [ADEM]). For some patients, ADS occurs as a monophasic illness, whereas for others it represents the first clinical manifestation of multiple sclerosis (MS). Table 1 provides a diagnostic evaluation for children suspected of having an acquired demyelinating syndrome or MS.
| The following investigations should be performed, as clinically indicated: | |
| MR imaging | Brain MR imaging in all children Spine MR imaging in all children with clinical spine involvement Orbital MR imaging for children with visual loss The following MR imaging sequences are suggested: FLAIR or T2-weighted sequences in at least 2 planes Pre- and postgadolinium T1-weighted images Diffusion-weighted sequences |
| Evoked potentials | VEPs SSEPs |
| Laboratory screening for NMO and MAS | Serum NMO IgG CSF NMO IgG (if serum negative) Ferritin Triglycerides |
| Infection screening | CBC + differential Serum viral serologies (EBV, mycoplasma, HSV serology) VDRL Lyme disease (seasonal) Cysticercosis (based on travel to endemic areas only) HTLV (based on travel to endemic areas only) |
| Endocrine | TSH, T4, anti-TPO antibodies if Hashimoto encephalopathy is a consideration |
| Mitochondrial lactate serum + CSF | Pyruvate; if higher than normal lactate, calculate lactate to pyruvate ratio DNA studies, skin and muscle biopsy if mitochondrial disease strongly suspected |
| Rheumatologic disease | ESR, CRP ANA, dsDNA Anticardiolipin and antiphospholipid antibodies Angiotensin-converting enzyme CXR (if sarcoidosis is strongly suspected) |
| Nutritional | Vitamin B12 (serum) 25-hydroxyvitamin D (25(OH)D) |
| CSF studies | Glucose Lactate Protein Cell count Culture and sensitivity, Gram stain when appropriate Oligoclonal bands (compared with concurrently obtained serum) a CSF viral cultures + PCR herpesviruses Cytology (if indicated) |
a The accuracy of oligoclonal band measurement depends on the diagnostic test used and on the experience of the laboratory performing the test. Isoelectric focusing has the highest sensitivity.
Although well characterized clinically and radiologically, the clinical features of acute demyelination are not specific. Clinicians must be alert to other neurologic disorders with similar signs. The diagnosis of monophasic ADS and MS requires exclusion of other diagnoses. Table 2 highlights some of the MR imaging features that should prompt clinicians to consider diagnoses other than ADS and MS. This article reviews the features that should prompt consideration of diseases that mimic ADS and MS, using vignettes to highlight unusual clinical and radiologic features.
| MR imaging | Leptomeningeal enhancement | SVcPACNS Infection Tumor HLH | Leptomeningeal enhancement is not a feature of MS in adults, and emerged as a red flag for vasculitic or malignant processes in the pediatric cohort |
| Lesion expansion | Tumor Lymphoma PML Sarcoidosis | Increased size of T2 lesions on serial imaging is well recognized in MS, although this should always prompt consideration of malignancy. Increasing size of a white matter–predominant lesion without lesion enhancement in a patient treated with immunosuppressant therapy (or a patient with known HIV) should prompt consideration of PML. PML is a risk for MS patients exposed to more intense immunosuppressive therapies | |
| Hemorrhage | ANE Stroke Cerebellitis AHLE Large-vessel CNS vasculitis SVcPACNS | Although susceptibility-weighted imaging reveals tiny microfoci of hemosiderin in MS patients, hemorrhage large enough to be visible on conventional MR imaging sequences is not a feature of ADS or MS, and should prompt consideration of disorders in which the cerebral vasculature is specifically involved |
Typical features of pediatric demyelination on MR imaging
As detailed in the article elsewhere in this issue by Verhey and colleagues, MR imaging plays an increasingly important role in the diagnosis of monophasic ADS and MS. The MR imaging appearance of childhood MS is characterized by multiple white matter lesions, which are of increased signal on T2-weighted and fluid-attenuated inversion recovery (FLAIR)-weighted images. Lesions may enhance with administration of gadolinium. However, enhancement may be absent even in acute lesions. Areas of hypointensity on T1-weighted images may reflect acute lesions or areas of long-standing regional tissue loss. Younger children often exhibit larger and more diffuse, bilateral white matter lesions with ill-defined borders that are frequently confluent at disease onset. Despite the important role played by MR imaging in the diagnosis of ADS and MS, it must be used in conjunction with clinical features.
Distinguishing acute demyelination from acute vascular insult in the spinal cord
Acute neurologic deficits prompt consideration of vascular occlusion and cerebral or spinal cord infarction, key differentials of ADS. In patients with infarction, the rapid development over minutes to hours of maximal deficit favors vascular occlusion. However, acute deficits can occur in patients with ADS, particularly those with TM. MR imaging lesions that conform to specific vascular distributions in the brain or anterior spinal artery of the spinal cord would support vascular causes. As emphasized by the following 2 vignettes, distinguishing vascular from demyelinating disease can be difficult.
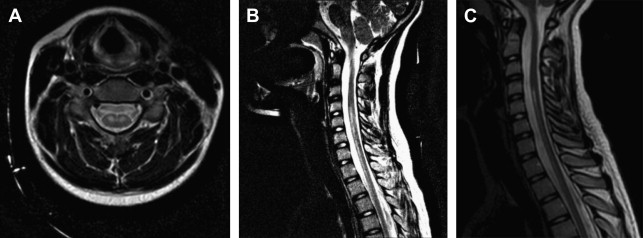
An 11-year-old girl presented with acute onset of back pain, shooting pain down her legs, loss of bowel and bladder control, and 4-limb weakness that developed over 1 to 2 hours. Weakness then worsened progressively to complete paralysis over the next 5 days with concomitant respiratory failure. MR imaging of the spine on day of onset revealed a focal hyperintensity on T2-weighted images in the anterior aspect of the cervical cord, more prominently involving the anterior horn cells, extending from the C3 level to the T2/T3 level with no diffusion restriction ( Fig. 1 A, B). Repeat MR imaging on day 5 showed expansion of the cord from C3 to T2. MR imaging of the brain was normal. Spinal fluid analysis revealed a normal protein and cell count. Serum coagulation profile was normal.