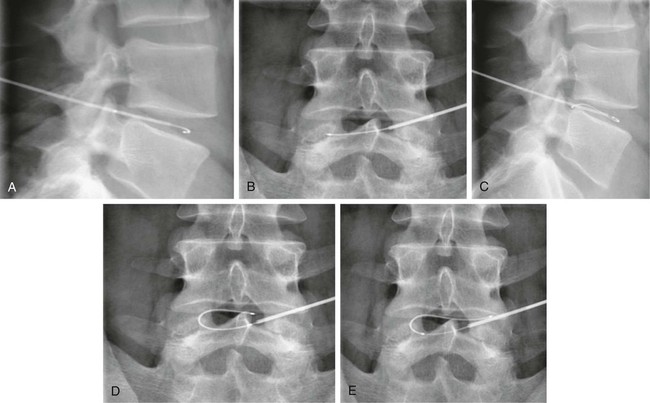
When medical treatment has been unsuccessful for patients with low back pain (LBP) due to a small or contained herniated disk, minimally invasive techniques have recently been developed as “alternative” treatments to surgical intervention. Outcomes of these alternative treatments depend on the characteristics of the herniation itself and on the chosen technique.1 Techniques include: • Chemodiscolysis with chymopapain (no longer used) • Automated percutaneous lumbar discectomy (APLD), developed by Onik • Percutaneous laser disk decompression (PLDD) • Intradiscal electrothermal therapy (IDET) • Percutaneous coblation nucleoplasty • Dekompressor percutaneous diskectomy • Chemodiscolysis with O2-O3 mixture, with periradicular and periganglionic infiltration All techniques can be performed under computed tomography (CT) or fluoroscopic guidance with the patient in prone position and under local anesthesia.2 They offer good results, good patient compliance, low cost, and low complication rates. Patients need a short period of hospitalization, but most procedures can be performed in day surgery, and in cases of failed treatment, all techniques can be repeated once without interfering with surgery at a later date. All procedures can be performed at either cervical or lumbar levels. The rationale of all percutaneous treatments is to reduce the intradiscal pressure in different ways, creating the space required to decompress retropulsion or mass affect of the disk. • Clinical criteria: LBP and sciatica resistant to conservative medical therapy, physiotherapy, and other interventions for a period not shorter than 2 to 3 months • Neurologic criteria: paresthesia or altered sensitivity over the dermatome involved, mild muscle weakness, and signs of root ganglion irritation • Psychological criteria: a firm resolve on the part of the patient to recover, with a commitment to cooperate and undergo subsequent physiotherapy with postural and motor rehabilitation • Small and medium-sized herniated disks correlating with the patient’s symptoms, with or without degenerative disk-vertebra disease complicated by intervertebral disk changes (protrusion, herniation) • Pain provoked by low-pressure contrast injection in the compromised disk during diskography for IDET, nucleoplasty, and APLD techniques • Residua of surgical (micro)-diskectomy, with herniation recurrence and/or hypertrophic fibrous scarring All techniques require specific radiologic guidance with CT or fluoroscopy (DSA, C-arm). The choice among different techniques depends on personal preference and availability. Generally, all procedures can be performed under fluoroscopic guidance or CT without any significant difference. Use of CT helps identify the presence of bowel loops behind the psoas muscle, an absolute contraindication for any oblique approach to the disk.2 This technique is indicated for all types and locations of disk protrusions or herniations without extrusion or free fragments. The success rate is about 70% to 80%. If the exclusion criteria are not considered, the success rate drops to 49.4%. When the procedure is not performed correctly, it may damage nerve roots or dural tissue. The most serious complication reported with this procedure is cauda equina syndrome, characterized by saddle anesthesia of the perineal region, retention or urine/fecal incontinence, and bilateral hyposthenia.3–5 If the disk herniation is not contained but still connected to the intervertebral disk, it is better to perform the decompression procedure under CT guidance to better assess the connection of the disk and hernia portions. In this way, the laser energy can be released in multiple locations of the herniated disk, obtaining better vaporization and retraction of the hernia, with resultant root decompression and resolution of symptoms. The outcomes reported are success rates between 75% and 87% of cases, with an immediate reduction of back pain in 48% of cases. Septic and aseptic diskitis are the most common complications, with an average occurrence of 0% to 1.2% of cases. Septic diskitis is caused by introduction of microorganisms during positioning of the needle into the disk. Sterile technique is required. Aseptic diskitis is caused by the action of the laser itself on the disk and the adjacent vertebral plate.6–12 IDET acts on the posterior aspect of the fibrous annulus, unlike other techniques where the action is on the nucleus pulposus. Under fluoroscopic guidance, a trocar is introduced into the intervertebral disk, then an electrothermal flexible catheter is introduced between the nucleus pulposus and annulus. The tip of the catheter has a resistor that, once placed near the posterior margin of the annulus, is warmed to 90°C for 16 to 17 minutes and then removed (Fig. 161-1). Warming the fibrous annulus reduces symptoms and stabilizes the disk lesion by reorganizing collagen fibers, strengthening the disk, cauterizing ring fissures, and ablating pain receptors. IDET is indicated for treatment of a bulging disk or contained herniated disk without root compression symptoms and resistance to pharmacologic therapy and physiotherapy for more than 6 months. To obtain a better evaluation of a contained hernia, disk compression, or disk pressure, a previous diskography may be needed. The complication rate is 0.8%, with high frequency of osteonecrosis post IDET. The success rate is between 40% and 71% of cases.12–17
Minimally Invasive Disk Interventions
Introduction
Indications and Contraindications
General Exclusion Criteria
General Inclusion Criteria
Choice of Radiologic Guidance
Technique
Automated Percutaneous Lumbar Discectomy
Percutaneous Laser Disk Decompression
Intradiscal Electrothermal Therapy
Minimally Invasive Disk Interventions