• A direct or indirect lung insult resulting in diffuse alveolar damage • ARDS and acute lung injury (ALI) describe the same clinicopathological process – the difference is merely one of severity
Miscellaneous ITU chest conditions
LUNG TRANSPLANTATION
LUNG TRANSPLANTATION
Get Clinical Tree app for offline access
ACUTE RESPIRATORY DISTRESS SYNDROME (ARDS)
ACUTE RESPIRATORY DISTRESS SYNDROME (ARDS)
DEFINITION
 the increased pulmonary microvasculature permeability allows protein-rich fluid to pass into the alveolar spaces at normal hydrostatic pressures
the increased pulmonary microvasculature permeability allows protein-rich fluid to pass into the alveolar spaces at normal hydrostatic pressures

 idiopathic pulmonary fibrosis
idiopathic pulmonary fibrosis  sarcoidosis
sarcoidosis  lymphangioleiomyomatosis
lymphangioleiomyomatosis bronchiectasis
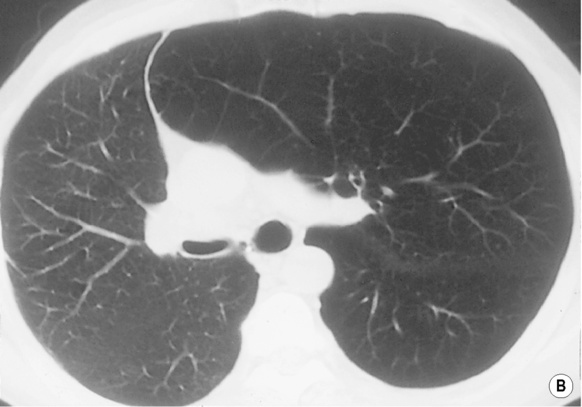
bronchiectasis CT chest
CT chest  quantitative ventilation–perfusion scintigraphy
quantitative ventilation–perfusion scintigraphy causes include interruption of the donor lung lymphatic drainage, underlying donor lung injury, surfactant deficiency and pulmonary capillary ischaemic damage
causes include interruption of the donor lung lymphatic drainage, underlying donor lung injury, surfactant deficiency and pulmonary capillary ischaemic damage linear or reticular shadowing is also common
linear or reticular shadowing is also common  peak shadowing is seen at day 4 and has usually cleared by day 10 post-op
peak shadowing is seen at day 4 and has usually cleared by day 10 post-op a lost cough reflex
a lost cough reflex  impaired mucociliary function (as the transplanted lung is denervated)
impaired mucociliary function (as the transplanted lung is denervated) Pseudomonas
Pseudomonas  Aspergillus
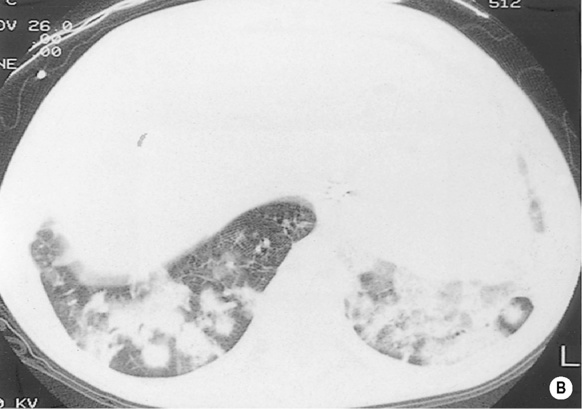
Aspergillus ground-glass opacification
ground-glass opacification  septal thickening
septal thickening  multiple or single nodules
multiple or single nodules  pleural effusions
pleural effusions the majority respond to IV methylprednisolone
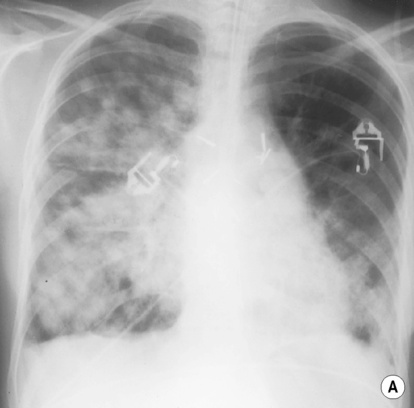
the majority respond to IV methylprednisolone it can demonstrate new or persisting airspace opacities 5–10 days following transplantation
it can demonstrate new or persisting airspace opacities 5–10 days following transplantation  there may be pleural effusions and interstitial lines without other signs of heart failure
there may be pleural effusions and interstitial lines without other signs of heart failure ground-glass opacification or septal lines may be the predominant finding
ground-glass opacification or septal lines may be the predominant finding acute allograft rejection
acute allograft rejection  low cardiac output
low cardiac output  prolonged postoperative ventilation
prolonged postoperative ventilation episodes of acute rejection increase the likelihood of developing OB
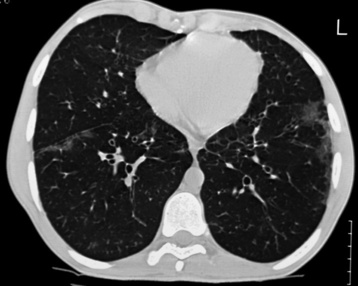
episodes of acute rejection increase the likelihood of developing OB there can be signs of lung overinflation and subtle attenuation of the peripheral airways as the disease progresses
there can be signs of lung overinflation and subtle attenuation of the peripheral airways as the disease progresses air trapping at end expiration
air trapping at end expiration  mosaic perfusion
mosaic perfusion  bronchiectasis is commonly present
bronchiectasis is commonly present it usually occurs during the 1st year post transplant (affecting 5–20% of patients)
it usually occurs during the 1st year post transplant (affecting 5–20% of patients)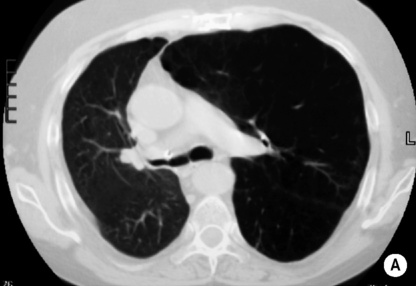

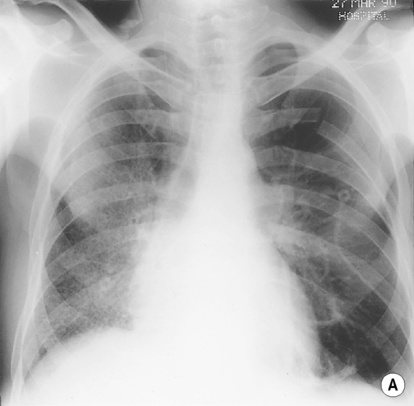


 a diminished pulmonary compliance
a diminished pulmonary compliance  normal pulmonary capillary wedge pressures
normal pulmonary capillary wedge pressures







