Occupational lung and pleural diseases remain an important part of thoracic imaging, particularly in regions with extensive industrial activity. Modern CT and MRI provide the detail needed to recognize subtle structural changes, characterize tissue patterns, and separate benign abnormalities from early signs of more serious disease. Accurate interpretation helps clinicians plan appropriate follow-up and supports long-term management. This article reviews key imaging features associated with occupational exposures and highlights practical considerations that support clear, consistent reporting.
Understanding Occupational Lung and Pleural Disease in Imaging Practice
Radiologists often encounter findings that suggest exposure to airborne particles or fibers, even when the clinical history is incomplete. Many exposure-related conditions progress slowly, and early abnormalities may appear mild or nonspecific. Dusts, fibers, fumes, and chemical agents produce a wide range of radiographic and tomographic findings, from faint interstitial markings to focal pleural changes.
Patterns often reflect the type of exposure. Fibrogenic materials such as silica or asbestos typically cause persistent alterations in the pleura and interstitium. Organic exposures may produce more airway-centered findings. Even when symptoms are limited, CT can reveal subtle details such as thin subpleural lines, parenchymal bands, or early pleural thickening. Identifying these early features helps establish a baseline for future comparison.
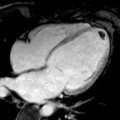
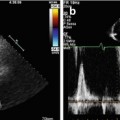
MRI contributes valuable information in specific scenarios. Tissue characterization sequences help distinguish fibrotic change from inflammation, and evaluation of the pleural surfaces can be more informative than on CT alone. MRI is particularly useful when questions arise about chest wall involvement or characterization of complex pleural masses.
Common Occupational Lung and Pleural Diseases Seen in Imaging
A variety of occupational conditions produce recognizable imaging patterns. Awareness of these helps radiologists interpret studies with greater confidence.
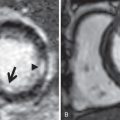
Asbestosis may present with subpleural reticulation, parenchymal bands, and traction bronchiectasis. Pleural plaques remain a classic indicator of prior exposure and often appear as sharply defined areas of pleural thickening.
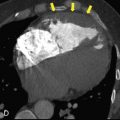
Silicosis often affects the upper lobes, with small nodules that may progress to larger masses. Hilar node calcification is a well-known associated finding that appears in a minority of cases.
Coal worker’s pneumoconiosis produces small, rounded opacities in the upper lobes and can resemble silicosis. Advanced disease may show conglomerate fibrosis with distortion of surrounding structures.
Talcosis produces high-attenuation nodules or interstitial thickening on CT. Some cases show mixed emphysematous and fibrotic changes.
Benign pleural thickening and plaques are common results of long-term exposure to fibrous materials or irritant dusts. Even thin, well-defined areas of pleural thickening can be useful clues when assessing work-related disease.
Additional patterns and considerations appear in this comprehensive review of pleural disease imaging, which outlines features often seen in the context of prior occupational exposure.
Key CT and MRI Findings Radiologists Should Recognize
CT remains the primary modality for assessing occupational lung and pleural conditions because it provides high-resolution evaluation of parenchymal and pleural structures. Thin-section CT helps radiologists visualize early interstitial abnormalities, small plaques, and faint lines adjacent to the pleura. Distribution is an important consideration. Upper-lobe nodularity suggests silicosis or coal worker’s pneumoconiosis, while lower-lobe reticulation is more consistent with asbestosis.
Pleural thickening varies in appearance. Smooth, localized thickening along the parietal pleura often reflects previous exposure, while nodular, irregular, or circumferential thickening warrants closer assessment. Irregular thickening involving the mediastinal pleura or producing contour distortion may indicate a more advanced or aggressive process.
MRI broadens the evaluation in select situations. T2-weighted sequences help separate fluid-rich inflammation from fibrotic tissue. Diffusion-weighted imaging can highlight areas of restricted diffusion that merit closer review. MRI also provides useful detail when assessing possible chest wall involvement, especially when CT findings remain unclear.
PET/CT can contribute metabolic information in cases with indeterminate pleural abnormalities. Uptake patterns should be interpreted carefully because benign inflammatory changes may show increased activity.
Avoiding Misdiagnosis: Distinguishing Benign Thickening From Malignant Progression
Pleural abnormalities associated with occupational exposures often remain stable for long intervals. When they change more quickly, or when thickening develops an irregular or nodular surface, the differential broadens. Malignant pleural processes may progress gradually, and early findings can be subtle. Thickening involving the diaphragmatic pleura or extending into fissures warrants careful evaluation. New parenchymal volume loss or adjacent soft-tissue components can increase concern.
Comparing current studies with prior imaging helps radiologists understand the significance of small differences in thickness, contour, or symmetry. Smooth, symmetric thickening often suggests a benign process. Asymmetry, nodularity, or rapid change may support further investigation. When findings remain indeterminate, follow-up imaging or tissue sampling may be considered depending on the clinical picture.
Knowledge of exposure-related disease patterns contributes to confident interpretation. Further context appears in asbestos-related health effects, which outlines clinical and pathological changes that often align with imaging findings.
How Regional Patterns Shape Exposure History and Reporting
Work history remains central to understanding pleural and parenchymal findings associated with occupational conditions, and regional variation plays an important role. States with extensive manufacturing backgrounds often show higher rates of exposure-related imaging abnormalities. Illinois is a familiar example. Industrial sites in and around Chicago contributed to long-term asbestos use across multiple trades, resulting in a wider range of pleural findings among individuals with past exposure.
Other states present different patterns. Pennsylvania’s mining and steel production history often corresponds with both pneumoconiosis and pleural scarring. Coastal areas of California have a long history of shipbuilding and large construction projects, conditions that have produced their own forms of exposure. Michigan’s automotive manufacturing legacy has produced a mix of airway and pleural abnormalities. States with less heavy industry, such as Colorado, generally show lower overall exposure rates, although isolated cases still appear depending on local occupations.
Understanding how exposure patterns vary helps radiologists interpret subtle findings, especially when patients provide only general information about their work history. The level of detail in a report can influence subsequent decisions. When pleural thickening, plaques, or other features suggest prior exposure, individuals sometimes seek clarification about the significance of those findings. In Illinois, this occasionally includes contacting a Chicago mesothelioma lawyer to understand how documented exposure relates to their broader medical situation. These conversations occur outside the radiologist’s role but highlight the value of clear, well-structured reporting.
Strengthening Reporting Practices for Occupational Lung and Pleural Disease
Clear reporting supports clinical decision-making and helps ensure continuity of care. When describing pleural thickening, details such as thickness, extent, and location help clinicians determine whether the appearance aligns with known exposure patterns. Distinguishing focal plaques from more diffuse thickening, or noting irregular margins when present, provides meaningful context for follow-up.
Radiologists can also highlight imaging features that suggest the nature of a prior exposure. Parietal pleural plaques often reflect contact with fibrous materials, while upper-lobe nodules may point toward a dust-related process. These interpretations do not replace a thorough occupational history, but they can prompt the clinical team to ask more targeted questions during follow-up visits.
Follow-up intervals should reflect the level of concern raised by imaging findings. Long-standing, stable plaques may not require additional imaging, whereas new nodularity or irregular thickening may warrant closer monitoring. Structured reporting templates support consistency, although clear descriptive habits achieve similar goals when templates are not used. Consistent reporting practices help clinicians accurately compare studies, even when examinations are performed at different facilities.
Conclusion
Occupational lung and pleural diseases produce a wide range of imaging findings that reflect the type and duration of exposure. CT and MRI play a central role in identifying subtle abnormalities, distinguishing benign patterns from more concerning features, and guiding appropriate follow-up. A clear understanding of exposure-related patterns, combined with attention to morphology and distribution, supports accurate and reliable reporting. These practices provide meaningful value to clinicians and patients who rely on thoracic imaging to gain insight into conditions shaped by past occupational environments.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree