Case presentation
A 2-day-old patient is referred to the emergency department for failure to pass meconium. He was born at home and had prenatal care, although this was not consistent, as the mother had missed some of her appointments. The delivery was at term (38 weeks gestation), vaginal, and apparently uncomplicated. The infant was vigorous and did not require resuscitation other than standard drying and stimulation. The mother’s serologies were negative. He has been breastfeeding for 10–15 minutes’ total time, approximately every 2–3 hours. He appears to feed well. He has had some small voids.
Physical examination reveals an afebrile, vigorous child. Heart rate is 150 beats per minute, respiratory rate is 30 breaths per minute, and a blood pressure is 75/50 mm Hg. He has an overall normal examination, but there is abdominal fullness. There is no hepatosplenomegaly, apparent tenderness, or discoloration of the abdomen. He has a patent anus and appears to have decreased rectal tone with digital rectal examination.
Imaging considerations
Plain radiography
Plain radiography is an excellent first-line imaging modality in patients where a bowel obstruction, either mechanical or functional, is suspected. It is the initial imaging modality typically used in the evaluation of patients with suspected meconium ileus or meconium plug syndrome. In patients with suspected Hirschsprung disease, radiographs of the abdomen may demonstrate marked gaseous distension of the colon with an undilated rectum with a transition zone in-between. , This modality has the advantage of detecting free air and calcifications and evaluating bowel gas patterns.
Contrast enema
After initial plain radiography is performed, contrast enema with water-soluble iodinated contrast is the imaging modality of choice for further evaluation of the newborn with failure to pass meconium and/or abdominal distension and dilated bowel loops suggestive of lower gastrointestinal obstruction. Water-soluble enema can be therapeutic for meconium ileus and immature left colon syndrome (also called small left colon syndrome or meconium plug syndrome). An enema for this indication should only be performed by a pediatric radiologist or a radiologist otherwise experienced in neonatal fluoroscopy, as there is a risk of bowel perforation.
Computed tomography (CT)
In neonates with failure to pass meconium and suspected bowel obstruction, CT is not utilized.
Ultrasound (US)
Prenatal sonography can show findings of gastrointestinal obstruction, including findings suggestive of meconium ileus and Hirschsprung disease. However, ultrasound is generally not utilized as a first-line study in the evaluation of newborns with failure to pass meconium.
Imaging findings
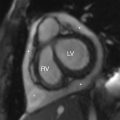
The history of delayed passage of meconium was concerning in this child. Plain abdominal radiography was obtained. These images demonstrated a very abnormal bowel gas pattern, with dilated bowel loops suggestive of a distal small bowel or proximal colonic obstruction, very suspicious for meconium ileus considering the mottled soap bubble-like appearance of gas in the right abdomen ( Fig. 9.1 ).

Case conclusion
The child was admitted to the neonatal intensive care unit; multiple subspecialists, including pediatric surgery, pediatric gastroenterology, and medical genetics, were consulted. The patient underwent a contrast enema, which demonstrated a nondilated and patent, but empty, colon, with reflux of contrast into nondilated distal ileum, without meconium in the visualized distal ileum. As differential considerations included total colonic Hirschsprung disease, a rectal biopsy was performed, revealing no ganglion cells in the rectum. Further evaluation showed no ganglion cells in the colon, or ileum. At surgery, the transition zone was in the distal jejunum/proximal ileum. This was consistent with long-segment Hirschsprung disease. A distal jejunostomy was created with a total abdominal colectomy and ileal resection, as well as a Hartmann pouch of the rectum; the child ultimately had a pull-through procedure. He has had a difficult clinical course, with several admissions for enterocolitis and dehydration. The child underwent genetic testing and was found to have a genetic profile consistent with long-segment Hirschsprung disease.
When a neonate fails to pass meconium, cystic fibrosis with meconium ileus, Hirschsprung disease, and meconium plug syndrome should be considered as possible etiologies, but metabolic disorders (thyroid disease), genetic disorders (Down syndrome), and intestinal disorders (e.g., intestinal atresia) are also in the differential diagnosis. Meconium ileus is a functional obstruction at the level of the terminal ileum that is caused by inspissated meconium. Immature left colon syndrome (small left colon or meconium plug syndrome) is a benign cause of functional large bowel obstruction in the neonatal period that presents with delayed passage of meconium. A water-soluble contrast enema is often needed for resolution, although meconium plug syndrome can resolve on its own. , In most cases, after the therapeutic effect of the enema, there are no further issues.
Imaging in meconium ileus will demonstrate a normal-length, small-caliber colon (microcolon), with inspissated meconium in the terminal ileum, and dilation of the small bowel proximal to the obstruction. In patients with immature left colon syndrome, the descending colon and rectosigmoid are normal in caliber, with transition to dilated more proximal colon at the splenic flexure, and scattered pellets of meconium are seen in the colon. Almost all patients with meconium ileus will be found to have cystic fibrosis, and repeat enemas may be necessary to treat meconium ileus. If enemas fail to relieve the obstruction, surgical management may become necessary.
Contrast enema is also the diagnostic imaging modality of choice in patients with suspected Hirschsprung disease. Findings consistent with Hirschsprung disease on enema include a normal caliber rectum and colon distal to the transition between the normally innervated colon and the more distal aganglionic segment. Bowel proximal to the transition is dilated. Rarely, Hirschsprung disease can involve the entire colon or the small bowel. Retention of contrast in the bowel 24 hours after the enema on the delayed radiograph can be seen with Hirschsprung disease or other motility disorders.
Hirschsprung disease was first described in 1886. The etiology of Hirschsprung disease is due to both cellular and genetic factors, with an incidence of 1 in 5000 births. Early arrest of the migration of neural-crest—derived neuroblasts to the developing intestine leads to an agangliotic segment. , , , This impedes the propagation of peristaltic waves due to the absence of parasympathetic intrinsic ganglion cells, causing functional obstruction. , There are multiple genetic factors that influence the development of Hirschsprung disease, and having siblings with a history of Hirschsprung disease is associated with an increased risk of the condition in subsequent children. , The majority of patients are diagnosed in the neonatal period (90%), but diagnosis may be delayed and can present outside of the neonatal period as chronic constipation. , , In addition to delayed meconium passage, feeding intolerance, vomiting, and abdominal distention are also presenting symptoms; abdominal distention and emesis are particularly common symptoms in children with Hirschsprung disease. Infants with fever, diarrhea, and abdominal distention should be carefully evaluated for Hirschsprung-associated enterocolitis, which, if not recognized and appropriately treated with fluid resuscitation, antibiotics, and emergent surgical consultation, can progress to toxic megacolon, which has a high mortality. ,
The diagnosis of Hirschsprung disease can be confirmed by several methods. Initial testing is accomplished with contrast enema, anorectal manometry, and either full-thickness rectal biopsy or rectal suction biopsy. The sensitivity and specificity for Hirschsprung disease have been reported to be 65%–80% and 61%–100%, respectively, for contrast enema; 75%–100% and 85%–97%, respectively, for anal manometry; and 90%–100% for surgical diagnosis. , ,
The management of Hirschsprung disease should begin with a thorough history and physical examination. If there are signs of Hirschsprung-associated enterocolitis (fever, diarrhea, and abdominal distention), aggressive resuscitation, antibiotics, and prompt surgical consultation are indicated; this entity can occur both before and after repair and can be fatal. , Surgical repair of Hirschsprung disease has traditionally involved a several-staged repair, but one-stage transanal laparoscopic pull-through techniques have been developed and utilized as well. , , Outcomes are generally good. Patients with long-segment disease and those with Down syndrome tend to have poorer outcomes. Postoperative complications include early complications (wound infection, wound dehiscence, and bowel obstruction) and late complications (bowel obstruction, stricture, incontinence, and enterocolitis), but there is clinical overlap between the two. ,