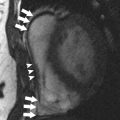
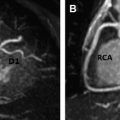
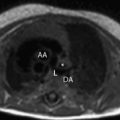
Abnormal thickening or rigidity of the pericardium may compromise normal cardiac function. This condition is known as pericardial constriction, or constrictive pericarditis. Several imaging modalities are used to evaluate the pericardium, including MR, computed tomography, and echocardiography, which can all play a complementary role aiding diagnosis. This article focuses on MR imaging and its role in the detection and evaluation of pericardial constriction. MR imaging has many advantages compared with other modalities including precise delineation of the pericardial thickness, evaluation of ventricular function, detection of wall motion abnormalities, and provision of information about common (and potentially harmful) sequelae of pericardial constriction. The pericardium is an important component of the heart, with both anatomic and physiologic roles that are critical to ensuring normal cardiac function. Pericardial constriction has many causes and is often a source of significant morbidity and mortality. Cardiac MR imaging provides clinicians with comprehensive information, both about the pericardium and its effect on cardiac function, in addition to ancillary findings that may be missed by other modalities. Multiple other imaging techniques, such as computed tomography, echocardiography, and cardiac catheterization, are often used with clinical findings to provide a confident diagnosis. Accurate diagnosis of pericardial constriction and differentiation from restrictive cardiomyopathy are vital to provide prompt and appropriate treatment. The pericardium is a component of the heart with multiple anatomic and physiologic roles critical to ensuring normal cardiac function. One of its major roles is acting as a barrier to inflammatory disease, which constitutes a spectrum from acute pericarditis to chronic constriction. Some additional roles include maintaining normal heart positioning within the chest, limiting acute myocardial distention, and enhancing the normal interaction of the ventricles. These roles make the pericardium, both its anatomic and physiologic properties, a vital part of normal heart health. Comprehensive evaluation of both the pericardium and the heart as a whole is an invaluable tool for clinicians faced with treating pericardial constriction and differentiating it from a restrictive cardiomyopathy, which can have a similar presentation but a different management strategy. Pericardial constriction is commonly an idiopathic phenomenon. The 2 most common known causes of pericardial constriction in the developed world are prior cardiac surgery (18%), particularly coronary artery bypass grafting, and radiation therapy (13%), especially when the mediastinum is directly within the treatment field. In the past, infection (particularly tuberculosis) was the most common cause and remains the most common cause in developing countries and immunosuppressed patients. Overall, infectious pericarditis of all types, including both viral and fungal organisms, accounts for up to 16% of cases according to some estimates. The pericardium is inelastic and made up of 2 layers: the visceral pericardium (which is adherent to the epicardium) and the more fibrous parietal layer. These layers are separated by a potential space that can normally contain up to 50 mL of fluid. This potential space is tolerant of slow filling with fluid, explaining why large effusions (>50 mL) often do not have immediate deleterious effects on cardiac motion or result in cardiac tamponade. The pericardium surrounds the heart and also encases portions of the great vessels with normal attachments to both the sternum and diaphragm. The pericardium is normally 2 to 3 mm thick, as seen in Figs. 1 and 2 . Abnormal thickening is defined as greater than 4 mm. Pericardial constriction is defined as abnormal thickening and adhesion of the pericardial layers that limits normal ventricular distention and results in impaired ventricular filling. On histology, this thickening represents fibrosis and scarring. The abnormal thickening may be seen diffusely throughout the pericardium, or focally, frequently along the right ventricular free wall. When the pericardium becomes thickened and noncompliant the result is uniformly increased filling pressures in all cardiac chambers. For example, increased filling pressure in the left atrium results in rapid left ventricular filling, particularly in early diastole. Overall stroke volumes throughout the heart are decreased, primarily because of reduced preload. There is also increased ventricular interdependence through septal interactions, which results in the characteristic septal bounce on imaging, as detailed later. In addition, normal respiratory transmission of intrathoracic pressure changes to the cardiac chambers is lost. However, contractility is preserved. Therefore, there is an exaggerated respiratory variation in both inflow velocity and ventricular filling in patients with constrictive pericarditis. MR imaging has become the gold standard for the complete evaluation of the pericardium and the physiologic effects of pericardial constriction. A typical protocol is detailed in Table 1 . Advantages include the noninvasive technique, lack of ionizing radiation, and providing detailed physiologic information regarding cardiac function and wall motion in addition to anatomic evaluation of the pericardium. The high temporal/spatial resolution and exceptional soft tissue differentiation provide an excellent evaluation of the pericardium. Disadvantages include cost as well as being a more technically difficult examination to perform: both for the patient because of numerous breath holds and long acquisition time relative to computed tomography (CT), and also for the technologist and/or physician performing the study because of the complexity of cardiac MR imaging. One significant disadvantage is the poor ability of MR imaging with respect to detecting even large amounts of calcification. However, this limitation may be negligible, because many cases of constriction have no calcification present.
Key points
Introduction
Causes
Anatomy/physiology


MR Imaging Evaluation