T1 mapping, one form of tissue characterization performed with a parametric approach, has been gaining rapid popularity, as different sequences have been developed to integrate image acquisition into a clinical routine. This technique allows fast progression from the basics of sequence development to its application in normal individuals and distinct diseases, sometimes overriding the more gradual steps taken with other cardiovascular magnetic resonance advances. In this review, the state-of-the-art in T1 mapping is examined, focusing on its techniques, sequences, comparison of native versus extracellular volume fraction measurements, and the current and future clinical applications of the method. T1 mapping techniques have evolved along the years and become more simplified to be integrated into a clinical cardiovascular magnetic resonance examination. Native T1, postcontrast T1, and extracellular volume maps can be acquired and postprocessed manually or automatically in the scanner, simplifying the work flow. Longitudinal follow-up and comparison with normal values must be performed using the same T1 mapping method along with similar scanning parameters. Cardiovascular magnetic resonance (CMR) has evolved significantly in the last decade from a method restricted to anatomic imaging into a fully functional technique, incorporating in 1 single examination the possibility of looking at the many different facets of cardiovascular diseases with significant clinical impact. Tissue characterization by CMR has been a key component in these many options afforded by the examination, one that is truly unique compared with other methods. However, until recently, this examination could be performed only in a qualitative or semiquantitative way, depending on the delimitation of user-selected thresholds and standard deviation curves, compared with supposedly normal tissue or in simple visual assessment. This situation is especially the case when considering how late gadolinium enhancement (LGE) or edema imaging has been used; both techniques work well in regional lesions but fail to fully describe the more subtle involvement of the myocardium in diffuse disease. T1 mapping, 1 form of tissue characterization performed with a parametric approach, has been gaining rapid popularity, as different sequences have been developed to integrate image acquisition into a clinical routine. This technique allows fast progression from the basics of sequence development to its application in normal individuals and distinct diseases, sometimes overriding the more gradual steps taken with other CMR advances. In this review, state-of-the-art in T1 mapping is examined, focusing on its techniques, sequences, comparison of native versus extracellular volume (ECV) fraction measurements, as well as the current and future clinical applications of the method. T1 maps can be acquired using either inversion recovery (IR) or saturation recovery (SR) techniques. Both methods use a first pulse to change the original longitudinal magnetization followed by acquisition of images along the relaxation curve and a fitting model to derive T1 values. Table 1 summarizes current T1 map techniques and their advantages/disadvantages. Look and Locker developed the first IR sequences, which were applied clinically many years ago, but this technique has limited use in the heart and does not allow pixelwise fitting, because it requires continuous acquisition throughout the cardiac cycle. An advancement of this method to incorporate a segmented approach with a fixed acquisition period evolved into a modified Look-Locker IR (MOLLI) scheme. In MOLLI, multiple inversion times (TIs) are used with different trigger delays. These inversion pulses are interleaved with recovery periods to establish a more homogeneous initial magnetization along different heartbeats. The original MOLLI sequence used 17 heartbeats with acquisition of 3-3-5 images, with 3 heartbeats for recovery between each experiment: 3 (3)3 (3)5 notation. This first method suffered from a few problems, which were dealt with in subsequent developments of the initial principles. First, in some patients, the acquisition times could still take a long period of breath holding, resulting in subpar results. Second, because the readout for MOLLI uses a steady state free precession technique, it underestimates the final T1 value (generating in effect a T1* time), with need for a correction factor. Third, the fitting parameters were also dependent on heart rate (consequently on the inversion/recovery periods) and could vary significantly, especially in situations of extreme T1 values. To correct for these factors, new mixes in inversion/recovery times and number of heartbeats of the original sequences were proposed: for precontrast (native) acquisitions, a 5 (3)3 model has been proposed, with only 8 heartbeats and less dependence on the heart rate ; for postcontrast acquisitions, a 4 (1s)3 (1s)2 format may be used, because the recovery time can be shortened to only 1 second, as noted. For the blood pool, in which new fresh blood is entering the image plane, it is recommended that the original images be used without the correction factor (actual T1* images). Another approach to the IR method using a faster acquisition protocol is shortened MOLLI (shMOLLI). This sequence requires only 9 heartbeats using a 5 (1)1 (1)1 scheme, with conditional fitting of the last 2 images after relatively short TIs, depending on the length of the T1 (shorter T1s use all samples; longer T1s use only the first 5 images). This situation results not only in shorter overall acquisitions but also in less dependency on heart rate and on precontrast and postcontrast situations with wide ranges of T1 times. In exchange for these advantages, the shMOLLI sequence is known to underestimate the true T1 times by 4% when this value is more than 800 milliseconds, as well as presenting less signal-to-noise ratio (SNR) compared with the original MOLLI scheme. Apart from the first IR sequences, SR alternatives have been proposed in the light of their increased accuracy in exchange for shorter range of T1 values measured. The first technique to be applied clinically is saturation recovery single shot acquisition (SASHA), which acquires 1 image before any saturation followed by multiple SR pulses with different trigger delay times. There is no dependency on the readout for SASHA, so larger flip angles can be used, although this necessitates the fitting parameters to be altered, with a loss of precision. Moreover, because the SNR in these sequences is reduced compared with the IR sequences, there is an additional loss in precision with more artifacts. Because of its less widespread use in different clinical scenarios compared with MOLLI techniques, this technique might need more clinical validation studies but certainly holds promise as an alternative method for T1 mapping. Two recently published techniques might also add options to the T1 map sequence menu. The first one is a combined SR/IR sequence called saturation pulse prepared heart rate independent inversion recovery, which, as the name implies, is not sensitive to variations in rate at the expense of slightly longer acquisition times. The second is a new SR technique in which each RR interval receives a saturation pulse with the acquisition of longer delay times in the recovery curve performed across multiple heart beats (SMART 1 Map). This technique obviates T1* correction as in MOLLI and makes the sequence less sensitive to other imaging parameters. Two additional points are worth mentioning when discussing T1 mapping techniques. First, in principle, motion correction can be applied to all sequences described earlier, which should help with the creation of automatic pixel-fitted color maps. Second, many factors still influence the T1 results, and even small changes in parameters might hinder the possibility of T1 comparison among different time points or individuals. Therefore, it is essential in longitudinal studies to stick to the same original sequence used instead of changing many parameters or type of sequence designs. When performing T1 mapping, there are many choices for how to evaluate the myocardium with the previously described sequences. The simplest form is by running the sequences without any contrast and obtaining the native T1 measures (also previously called precontrast or noncontrast). Many investigators have described the use of native T1 in different clinical scenarios, as explained later; this setting is particularly useful in patients with renal disease, for example. Another way to apply T1 mapping is through the injection of gadolinium-base contrast media at doses that vary from 0.15 to 0.2 mmol/kg, with subsequent imaging of the myocardium after at least 15 minutes from the bolus injection. This approach seems to offer similar results compared with the alternative equilibrium contrast infusion and is more easily applicable in daily practice. Both techniques allow for the quantification of postcontrast T1 values in comparable ways. Although both native and postcontrast T1 measurements show promising clinical applications, by measuring both values along with the T1 figures for the blood pool and the patient’s hematocrit (Ht) level, the ECV of the myocardium can then be calculated, which is more stable over time and may have more relevance in clinical practice. ECV can be automatically calculated inline by the scanner, but this usually needs to be performed manually during postprocessing: the partition coefficient λ is calculated from (1/T1 pre Gd – 1/T1 post Gd) myocardium /(1/T1 pre Gd – 1/T1 post Gd) blood , where Gd is gadolinium; the ECV is then calculated as λ (1-Ht). The normal myocardial structure contains both myocytes and connective tissue, with cardiac myocytes representing most of the myocardial mass. Therefore, intracellular space corresponds to most of the myocardial volume. Cardiomyopathies, despite their multiple causes and complex processes causing the myocardial injury, have a usual final pathway that involves myocardial fibrosis deposition and increase in extracellular space. Myocardial fibrosis can be classified in several subtypes, such as reactive interstitial fibrosis, infiltrative interstitial fibrosis, and replacement or scarring fibrosis. These processes can cause a change in the ratio of myocytes to interstitial volume, may occur diffusely on the myocardium, and may be an early abnormality in some cases. As we previously commented, this diffuse change on the extracellular space is missed by techniques depending on regional heterogeneity of myocardial abnormalities, such as LGE, and can be detected only by measurements of myocardium longitudinal relaxation time before and after contrast and estimation of myocardium ECV. Several cardiomyopathies have been investigated in the recent literature, with a variety of different T1 mapping techniques. Despite the lack of standard measurements, the available data have repeatedly shown that changes in the T1 and ECV are present in the diseased myocardium and might have clinical and prognostic significance. Most of these data are reviewed in the following section. Myocardial fibrosis detectable by LGE has been reported in patients with severe aortic valve disease. The presence and magnitude of myocardial fibrosis correlated with clinical prognosis after aortic valve replacement. Moreover, the presence of myocardial fibrosis by LGE correlated with the burden of interstitial myocardial fibrosis measured by pathology on myocardium samples obtained during aortic valve replacement surgery. This finding might suggest that measurements of interstitial diffuse fibrosis would add significant clinical information. In 2006, a pilot study reported shorter T1s in 8 patients with aortic regurgitation compared with controls. In a more recent technical validation study, patients with severe aortic stenosis showed moderate correlation between ECV calculated by 2 T1 mapping sequences before and after contrast and collagen volume fraction derived from myocardial biopsy samples. The ability to obtain myocardial biopsies during aortic valve replacement surgery also provided further histologic validation of ECV in patients with severe aortic stenosis. In contrast, native T1 in patients with aortic stenosis were not different from normal controls. In a larger study, ECV in 66 patients with severe aortic stenosis correlated with end-systolic volume index and aortic valve area measured by echocardiography. Only 42% of these patients had some degree of LGE in the left ventricular (LV) myocardium. Optimization of the T1 techniques in 3 T are still being investigated, using patients with aortic stenosis as the validation group. T1 mapping and ECV are altered in patients with severe aortic stenosis and correlate to LGE presence and a variety of clinical and imaging parameters of disease severity. Techniques are not standardized; there are no histologic validation data other than in severe aortic stenosis with indication to surgery, such as mild, moderate, or severe and asymptomatic patients; scarce data available on aortic regurgitation; and barely any data on clinical significance or prognosis of ECV in patients with aortic valve disease. Although these data are promising, additional clinical data are needed to bring T1 mapping and ECV calculation to clinical use. Myocardial fibrosis has been shown to be an important feature of hypertrophic cardiomyopathy (HCM), which can differentiate this disease from other causes of myocardial hypertrophy in pathology. Although fibrosis is not specific to HCM, its quantification and regional distribution provide useful information in the pathophysiology. Recent CMR studies have shown that myocardial fibrosis in patients with HCM correlate with disease severity and prognosis. However, approximately 65% of patients with HCM have any degree of LGE and, therefore, a threshold for myocardial fibrosis that indicates worse prognosis and that implantable cardioverter-defibrillator (ICD) implantation is still needed. Recently, an initial attempt of validation was performed using myocardial delayed enhancement by multidetector computed tomography, resulting in a cutoff of 18 g or 14% of LV mass for higher rates of appropriate therapy by ICD in patients with HCM. In a recent personal communication of data (Martin Maron, 2014) on a multicenter prospective trial using LGE by magnetic resonance imaging in patients with HCM, Dr Martin Maron reported that an LGE cutoff of 15% of LV mass indicates a worse prognosis in HCM. Therefore, the myocardial fibrosis process is critical in HCM and has established clinical and prognostic significance. Investigation of T1 values on HCM is still in its infancy. Native T1 values are higher in patients with HCM compared with controls, even in LV segments without LGE, but not different from patients with dilated cardiomyopathy (DCM). Although the differences in T1 values were small, T1 values provided an index with high diagnostic accuracy for the detection of diffusely diseased myocardium. Initial data in 2009 using T1 scout (Look-Locker) sequences in patients with HCM suggested that 10-minute postcontrast T1 values could identify dispersed myocardial damage. A technique of equilibrium contrast was first tested and validated in patients with HCM and was able to measure diffuse myocardial fibrosis, using multiple breath-hold acquisition of standard LGE with different TIs and also using single breath-hold shMOLLI for the calculation of ECV. The equilibrium technique in HCM was shown to be comparable with bolus only technique for a wide range of T1 values and ECV. The calculation of ECV in patients with HCM showed that the area of ECV greater than a fix threshold of 30.4% was consistently larger than the area of LGE measured as greater than 2 standard deviations of the remote nonenhanced myocardium. In patients with HCM, ECV did not correlate to any other CMR parameters (LV ejection fraction [LVEF] and volume indexes), except moderately with the percentage of LGE ( r = 0.48), but were larger than in normal individuals (0.291 ± 0.005 vs 0.250 ± 0.023, P <.001). This finding may be helpful in differentiating patients with HCM from those with other diseases that are usually confounded using regular techniques, such as athlete’s heart ( Fig. 1 ). This observation is especially true because the heterogeneity of scar and its diffuse distribution in patients with HCM makes definition of normal myocardium challenging in this disease and, thus, hampers the measurements of myocardial fibrosis based on LGE and standard deviation thresholds over the normal myocardial. In this scenario, T1 maps and, particularly ECV are a more attractive option and potentially more accurate for estimating disease severity. Yet, the clinical and prognostic value of T1 mapping and ECV calculation over the standard LGE still needs to be shown.
Key points
Introduction
T1 sequences
Sequence
Type
Number of Heartbeats
Advantages
Disadvantages
MOLLI (original)
IR
17: 3 (3)3 (3)5
First MOLLI sequence developed
Heart rate dependence
Long acquisition times
Underestimation of true T1 value (especially at fast heart rates)
MOLLI (native T1)
IR
8: 5 (3)3
No heart rate dependency
Fast acquisition
Underestimation of true T1 because of magnetization transfer effects
MOLLI (postcontrast)
IR
9: 4 (1s)3 (1s)2
No heart rate dependency
Fast acquisition
Less recovery phase needed with short T1
Few validation studies
MOLLI (T1*)
IR
Any of the above without need for correction
Used for LV blood assessment, with new inflow blood (eg, for ECV calculation)
shMOLLI
IR
5: (1)1 (1)1
No heart rate dependency
Accurate in both precontrast and postcontrast situations
Less signal-to-noise ratio compared with MOLLI
More prone to artifacts
Systematic underestimation of true T1 for values >800 ms (corrected by formula)
SASHA
SR
10
No T1* effect
No heart rate dependence
No T2 sensitivity in 3-parameter fit
Less sensitive to off-resonance effects
Less signal-to-noise ratio compared with IR sequences
Less precision if used in a 2-parameter fit model
Native, postcontrast, and extracellular volume fraction maps
Clinical applications of T1 mapping
Aortic valve disease
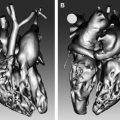
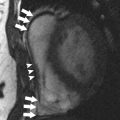
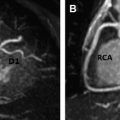
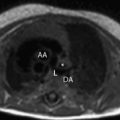
Hypertrophic cardiomyopathy