Magnetic resonance (MR) imaging should be part of the routine workup in suspected inflicted brain injury. The inclusion of diffusion-weighted MR imaging is essential for assessment of acute hypoxic-ischemic brain injury because of its sensitivity to delineate the extent of the lesions and because of its prognostic significance. MR imaging may offer additional help in dating the intracranial hemorrhages, but a precise timing is often difficult if not impossible.
The estimated incidence of nonaccidental or inflicted brain injury is 0.2 in 1000 infants younger than 1 year, and is associated with a high morbidity and mortality. Radiologists play an important role in the workup of suspected child abuse because the clinical presentation can be nonspecific and/or misleading. In a large series on 173 children with inflicted brain injury, 31% were initially misdiagnosed. Therefore radiologists should be aware of the imaging protocol and the possible findings. Radiologists should clearly mention the possibility of nonaccidental head injury in the report whenever necessary. It cannot be sufficiently emphasized that the acute changes on imaging can be extremely subtle.
A recent systematic review investigating the features that distinguish accidental from nonaccidental injury found that apnea and retinal hemorrhages were most predictive of nonaccidental injury, followed by rib fractures. Apnea leads to hypoxic-ischemic (HI) damage, and this will usually determine the outcome of the abused child.
Computed tomography (CT) is recommended as the first examination and should be performed following a cranial trauma in any child younger than 2 years. Brain CT is sensitive to the detection of fresh hemorrhage and brain edema. Images at bone window setting will depict most skull fractures.
This article is limited to the role of magnetic resonance (MR) imaging in the diagnostic workup of a child with suspected inflicted brain injury.
The first issue to be addressed concerns the technique and timing of MR imaging in the workup of inflicted brain injury.
Sedation and/or general anesthesia will usually be required, and therefore the appropriate MR-compatible monitoring equipment should be available.
In addition to the standard sequences, T2-weighted, T1-weighted (fast) spin-echo, and fluid-attenuated inversion recovery (FLAIR) sequences, a T2∗ gradient echo sequence and a diffusion-weighted (DW) imaging sequence should always be included. Coronal and sagittal images are useful for delineating the extent of the lesions in different planes.
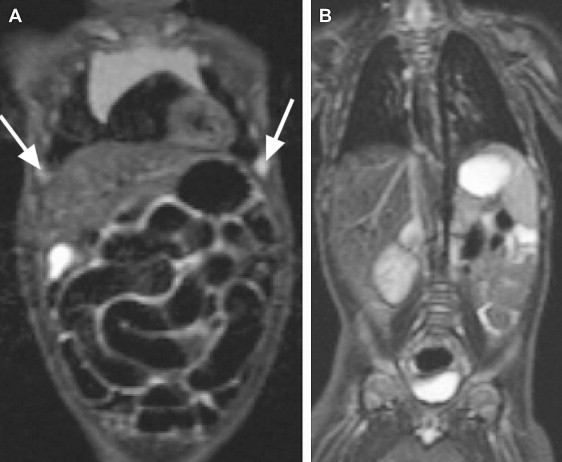
Three-dimensional susceptibility weighted (SW) imaging might replace T2∗ gradient echo sequences in the near future because of its superiority in depicting tiny hemorrhagic lesions. The number and size of the hemorrhages on SW imaging appear to correlate with the neurocognitive outcome. It has also been recommended to examine the cervical spine or even the whole spine, and the potential advantage of whole-body inversion recovery sequences to depict bone marrow edema is well known, although its value in inflicted brain injury remains to be proved ( Fig. 1 ). In a recent article it was shown that cervical cord injury is common whereas adjacent soft-tissue injury, fractures, and dislocations are often absent. The possible advantage of MR at 3 T in a child with nonaccidental intracranial injury remains to be assessed, but there seems to be a definite advantage because of the high field strength. MR venography can be used to confirm or demonstrate venous sinus thrombosis. The role of advanced MR techniques, such as MR spectroscopy, to demonstrate the presence of lactate, and diffusion tensor imaging to assess the extent of brain edema remains to be established.
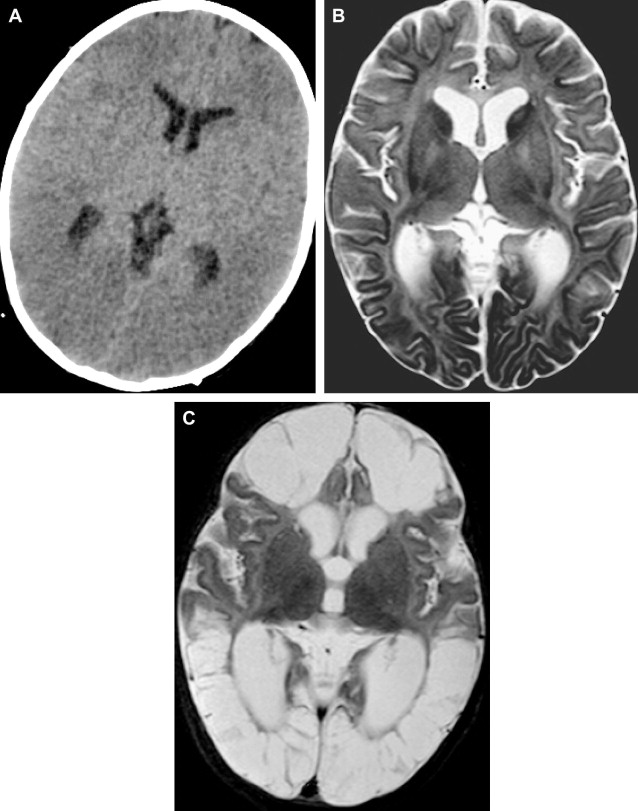
It has been suggested that the ideal timing of MR imaging would be 3 or 4 days after the admission of the abused child to the emergency department. A follow-up MR imaging 2 to 3 months later should be included whenever the first MR examination has demonstrated brain injury ( Fig. 2 ).
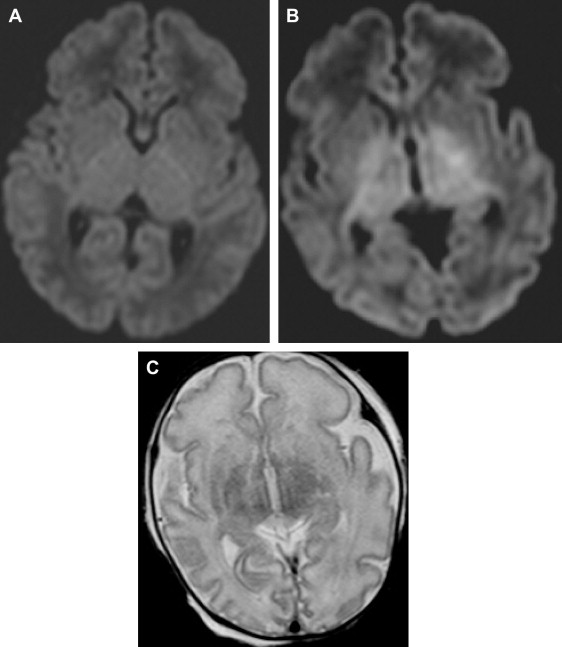
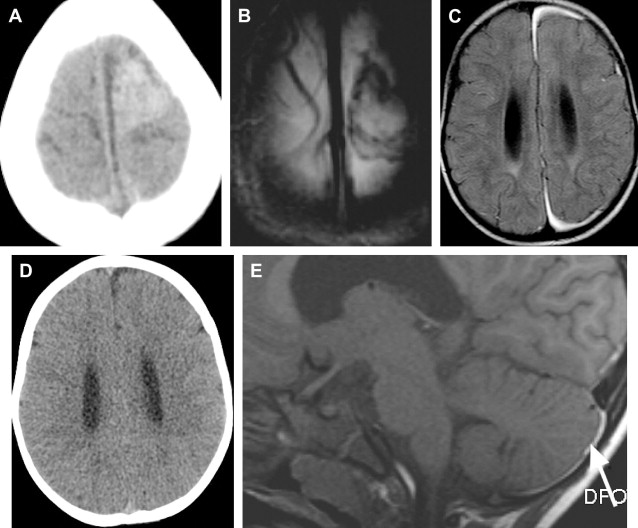
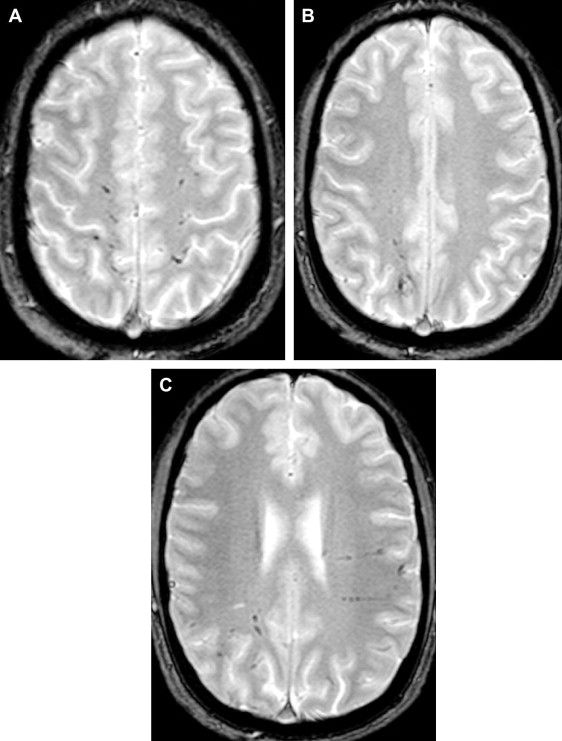
Several investigators have demonstrated the contribution of MR imaging in assessing a child with suspected inflicted brain injury, and have demonstrated the superiority of MR imaging over CT in children with inflicted brain injury. A recent systematic review on neuroimaging in inflicted brain injury recommends performing MR imaging in suspected head injury whenever the CT is abnormal or when there is clinical suspicion despite the normal initial CT. It is well known that early signs of HI brain injury and small subdural hemorrhages can be missed on CT ( Fig. 3 ). Additional information can be found on MR imaging in up to 25% of the children with abnormalities on CT. These findings may include additional subdural hemorrhages, subarachnoid hemorrhage, axonal shearing injury, ischemia, and contusions ( Fig. 4 ). In patients with a normal CT, MR imaging was abnormal in up to 50% of cases.
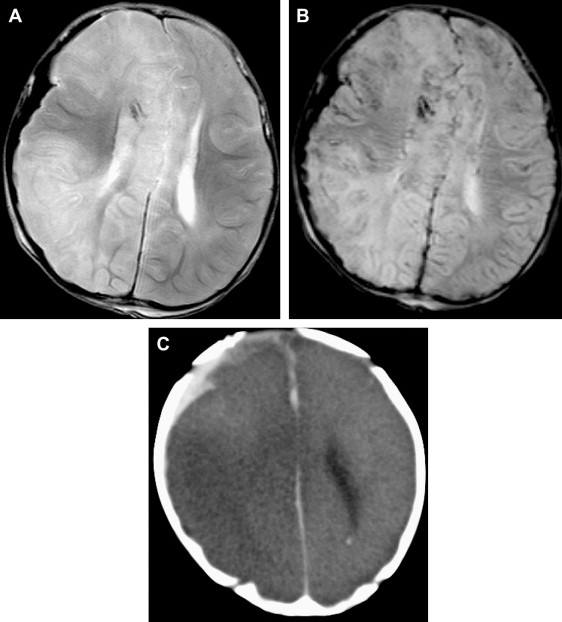
The authors also recommend postmortem CT and MR imaging to collect as much documentary evidence as possible for the forensic investigation. CT is more sensitive in demonstrating extracerebral hemorrhages, whereas MR imaging is superior in demonstrating parenchymal injuries ( Fig. 5 ).
The second issue is the contribution of DW imaging as part of the MR imaging protocol. DW imaging is a well-established technique that adequately depicts early changes associated with restricted diffusion due to cytotoxic edema. From the literature it is clear that DW imaging plays an important role in the delineation of the extent of HI damage to the brain. In perinatal asphyxia DW imaging is the most accurate technique to demonstrate acute brain damage ( Fig. 6 ). It has been suggested that an apparent diffusion coefficient value of more than 15% below the normal value (<85×10 −5 mm 2 /s) results in irreversible damage and a poor outcome ( Fig. 7 ). Whereas in adults HI lesions are usually confined to the cortex, it has been demonstrated that in the term infant the parasagittal regions are involved, and in severe hypotension the putamina, thalami, hippocampi, and peri-Rolandic area are also involved (see Fig. 6 ). HI injury has also been described in the globus pallidus, another region with high metabolic demand and vascular perfusion in watershed areas. Associated damage to the pars reticularis of the substantia nigra has been observed, and has been related to anemic anoxia due to decreased hemoglobin ( Fig. 8 ). Pallidoreticular damage has previously been reported in carbon monoxide intoxication.