Recent advances in noninvasive imaging methods, such as CT and MR imaging, have replaced most of invasive angiographic procedures in the diagnosis of acquired aortic disease, decreasing the cost and morbidity of diagnosis. This article reviews and illustrates present MR imaging methods for evaluation of the aorta. Common diseases of the aorta also are discussed with a focus on their unique morphologic and functional features and characteristic MR imaging findings. Knowledge of pathologic conditions of common aortic diseases and proper MR imaging techniques enables accurate and time-efficient aortic evaluation.
Acquired disease of the aorta is widespread. In the past invasive angiography was required to depict structural abnormalities. Recent advances in noninvasive imaging methods, such as CT and MR imaging, have replaced most of invasive angiographic procedures, thus decreasing the cost and morbidity of diagnosis. With its ability to delineate the intrinsic contrast between blood flow and vessel wall and to acquire images in multiple planes, MR imaging provides a high degree of reliability in the diagnosis of aortic diseases. Because of its noninvasive nature, MR imaging can be performed repeatedly, allowing the progression of the aortic disease to be evaluated over time. This article reviews and illustrates present MR imaging methods for evaluation of the aorta. Common diseases of the aorta also are discussed with a focus on their unique morphologic and functional features and characteristic MR imaging findings. Knowledge of pathologic conditions of common aortic diseases and proper MR imaging techniques enables accurate and time-efficient aortic evaluation.
Comparison with CT
Compared with MR angiography, CT angiography has the advantages of general availability and ease of performance, especially in urgent cases. Nevertheless, MR imaging has several distinct advantages over CT. First, MR imaging does not require the use of ionizing radiation. Because of the lack of radiation, MR imaging can be performed for repeatedly the follow-up of the patient without concern for radiation exposure. Second, unlike CT angiography, MR angiography dose not require the use of nephrotoxic iodinated contrast material. Nephrotoxicity is a particularly relevant issue, because patients who have acquired aortic disease frequently suffer from renal insufficiency. In particular, MR angiography has advantages for patients undergoing endovascular treatment. Preprocedural planning using MR angiography excludes concerns related to iodine load and impaired renal function, thus enabling same-day or close performance of endovascular treatment. Finally, cine MR imaging can be performed for dynamic evaluation of blood flow without using contrast material. Particularly, cine phase-contrast (cine PC) imaging can be used to determine flow velocity and direction. These cine MR techniques can be used to evaluate valvular and cardiac function.
Basic technical considerations
Several different MR imaging techniques are used to depict the arteries. These techniques include black-blood imaging (conventional spin echo, fast spin echo), bright-blood imaging (time-of-flight imaging, PC imaging), and contrast-enhanced MR angiography. Recent advances in fast imaging, such as steady state free precession (SSFP) and subsecond contrast-enhanced MR angiography, enable quick examinations for initial screening evaluations of the aorta within several minutes. These improvements in MR technology and the aforementioned advantages of MR imaging over CT evaluation have increased the role of MR angiography, even in the evaluation of some acute conditions.
Black-blood Vascular Imaging
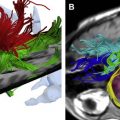
The aorta can be well illustrated using black blood methods, namely, ECG-gated spin echo or fast spin echo, that exploit the inherent contrast between rapidly flowing blood and the aortic wall. Unlike bright blood imaging, luminal signal void occurs because of the movement of spins and dephasing of turbulent flow. Spin echo imaging still constitutes the basis of any aortic study because this technique provides the best anatomic details of the aortic wall and pathologic conditions. Usually, a conventional study of the aorta in the axial plane is acquired first to display the orientation of the great arteries and to visualize mural lesions optimally perpendicular to their long axes. A main consideration in spin echo imaging is that each section corresponds to a different cardiac phase. Diastolic slow flow and entry or exit slice phenomena may produce high signal in the aortic lumen, which is difficult to differentiate from mural thrombus. Usually, T2-weighted imaging is of little usefulness in the study of the aorta because the low signal-to-noise ratio and the long acquisition time affect the image quality, mainly through motion artifact. With spin echo imaging the aortic caliber and also the vessel wall and perivascular tructures can be evaluated. Wall thickness can be demonstrated readily on T1-weighted imaging, and edema is seen as hyperintense intramural signal on T2-weighted imaging. Mural hyperenhancement of the vessel wall on T1-weighted images after injection of contrast material is considered to indicate active inflammation. ECG-gated double inversion recovery fast spin echo is a more recent black-blood method that allows breathhold acquisition. By applying a nonselective inversion pulse followed by a section-selective inversion pulse, double inversion recovery fast spin echo provides better suppression of the signal from flowing blood ( Fig. 1 ). This technique, however, is substantially less efficient in terms of scan time than fast spin echo technique because it is a sequential-slice imaging sequence.
Bright-blood Vascular Imaging
Several bright-blood techniques can be performed without the need for contrast agents. One of the oldest techniques is the time-of-flight (TOF) effect, which is based on the phenomenon of flow-related enhancement of spins entering into a partially saturated imaging section. These unsaturated spins give more signal than surrounding stationary spins. With the two-dimensional (2D) technique, multiple thin, sequential sections are acquired by using a flow-compensated gradient echo (GRE) sequence. The acquired sections are viewed individually or are reformatted with the maximum intensity projection (MIP) technique to obtain a three-dimensional (3D) image. TOF imaging has several limitations: (1) complex flow pattern producing loss of signal caused by intravoxel dephasing may mimic disease; (2) vessels not perpendicular to the acquired section plane may cause low signal intensity; (3) retrograde flow in collateral vessels may be saturated also, obscuring the true level of steno-occlusive lesions. Although arterial signal can be improved with cardiac gating, imaging times become long, and arterial signal on TOF MR angiography often remains inhomogeneous and unreliable for proper depiction of the aorta and its branches. Because of the long imaging times and aforementioned limitations, TOF imaging is being replaced rapidly with contrast-enhanced MR angiography.
The TOF effect can be useful when acquired in a 2D cine mode, for example, cine gradient echo (cine GRE). Cine GRE images are acquired with ECG gating, thus resulting in high temporal resolution throughout the cardiac cycle, and can be displayed in cine format. The recently introduced SSFP (commercially known as “true fast imaging with steady precession (FISP),” “fast imaging employing steady state acquisition (FIESTA),” or “balanced fast field echo (FFE”) technique, with shorter TE and TR sequences, has become more widely available. On SSFP, intraluminal signal generally is very high and homogenous even in cases of turbulent flow because this sequence depends mainly on a function of the T2/T1 ratio. Hence, in urgent situations, SSFP can be used to demonstrate quickly aortic abnormalities such as an intimal flap and a false lumen in aortic dissection.
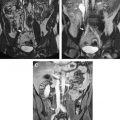
One critical advantage of flow-based bright-blood techniques is the ability to perform a functional assessment of blood flow. On cine GRE, turbulent flow produces rapid spin dephasing and results in flow jets extending distal to or downstream from the lesion, thus providing additional information in many pathologic conditions such as coarctation of the aorta, aortic valve insufficiency, and aortic dissection. Particularly in aortic dissection, the detection of entry and reentry sites is a special capability of this method that can be helpful in planning surgical and endovascular treatment. With the use of newer fast GRE pulse sequences with an ultrashort TR and TE, a flow jet may not be present despite the presence of a significant flow disturbance. The very short TE times may be insufficient for a sizable flow jet to form on this faster sequence. In cases of high suspicion, standard GRE sequences can be performed during free breathing ( Fig. 2 ). The longer TE will allow intravoxel dephasing to develop, and a flow jet should be seen if flow is turbulent.
Cine PC is another bright-blood technique that can be used for dynamic evaluation of blood flow. Cine PC depends on the phase shifts that flowing protons experience as they travel along the gradient field. The data obtained with cine PC are processed into two sets of images: magnitude and phase-contrast. PC images display the direction of flow as bright or dark pixels, with their relative signal intensity representing their velocity. Hence, PC images can be used to assess flow direction, which may be important information for proper identification of a vascular structure or for quantifying blood flow.
Contrast-enhanced MR Angiography
Contrast-enhanced MR angiography, which first was described for imaging of aortoiliac disease in 1993, is the most widely accepted method for comprehensive evaluation of the aortic disease. This technique can provide images that have high spatial resolution with a single breathhold and therefore is suitable for the depiction of aortic abnormalities such as aneurysm, dissection, penetrating atherosclerotic ulcer, and Takayasu arteritis.
Contrast-enhanced MR angiography uses the T1-shortening effect of a gadolinium-based contrast agent. By using a gadolinium chelate contrast agent, the T1 of blood is shortened so that the blood appears bright irrespective of flow patterns or velocities. Because signal enhancement and overall image quality of contrast-enhanced MR angiography depend on the intra-arterial concentration of the contrast agent, the correct timing of imaging after contrast material injection is crucial. Because image contrast depends mainly on central k-space data, collection of the central lines of k space during the plateau phase of arterial enhancement is essential for optimal contrast-enhanced MR angiography. The authors use 10 to 20 mL of contrast material delivered at a rate of 2 to 3 mL/s followed by 20 mL of saline solution delivered at the same rate. The dosage and delivery rate of the contrast material should be adjusted in individual patients, with special attention to the acquisition time. Several methods are used to determine the optimal delay between the start of intravenous contrast material injection and the start of image acquisition. Timing methods commonly used include injection of a test bolus using a small amount of contrast material, automatic triggering, and MR fluoroscopy.
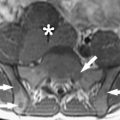
Imaging interpretation usually is done with the aid of a computer workstation on which individual source images are analyzed and postprocessing techniques, such as multiplanar volume reformation, MIP reformation, and volume rendering of the images, are performed. MIP images, in particular, can be obtained quickly, resemble catheter angiograms, and permit a 3D appreciation of anatomy ( Fig. 3 ).
Basic technical considerations
Several different MR imaging techniques are used to depict the arteries. These techniques include black-blood imaging (conventional spin echo, fast spin echo), bright-blood imaging (time-of-flight imaging, PC imaging), and contrast-enhanced MR angiography. Recent advances in fast imaging, such as steady state free precession (SSFP) and subsecond contrast-enhanced MR angiography, enable quick examinations for initial screening evaluations of the aorta within several minutes. These improvements in MR technology and the aforementioned advantages of MR imaging over CT evaluation have increased the role of MR angiography, even in the evaluation of some acute conditions.
Black-blood Vascular Imaging
The aorta can be well illustrated using black blood methods, namely, ECG-gated spin echo or fast spin echo, that exploit the inherent contrast between rapidly flowing blood and the aortic wall. Unlike bright blood imaging, luminal signal void occurs because of the movement of spins and dephasing of turbulent flow. Spin echo imaging still constitutes the basis of any aortic study because this technique provides the best anatomic details of the aortic wall and pathologic conditions. Usually, a conventional study of the aorta in the axial plane is acquired first to display the orientation of the great arteries and to visualize mural lesions optimally perpendicular to their long axes. A main consideration in spin echo imaging is that each section corresponds to a different cardiac phase. Diastolic slow flow and entry or exit slice phenomena may produce high signal in the aortic lumen, which is difficult to differentiate from mural thrombus. Usually, T2-weighted imaging is of little usefulness in the study of the aorta because the low signal-to-noise ratio and the long acquisition time affect the image quality, mainly through motion artifact. With spin echo imaging the aortic caliber and also the vessel wall and perivascular tructures can be evaluated. Wall thickness can be demonstrated readily on T1-weighted imaging, and edema is seen as hyperintense intramural signal on T2-weighted imaging. Mural hyperenhancement of the vessel wall on T1-weighted images after injection of contrast material is considered to indicate active inflammation. ECG-gated double inversion recovery fast spin echo is a more recent black-blood method that allows breathhold acquisition. By applying a nonselective inversion pulse followed by a section-selective inversion pulse, double inversion recovery fast spin echo provides better suppression of the signal from flowing blood ( Fig. 1 ). This technique, however, is substantially less efficient in terms of scan time than fast spin echo technique because it is a sequential-slice imaging sequence.
Bright-blood Vascular Imaging
Several bright-blood techniques can be performed without the need for contrast agents. One of the oldest techniques is the time-of-flight (TOF) effect, which is based on the phenomenon of flow-related enhancement of spins entering into a partially saturated imaging section. These unsaturated spins give more signal than surrounding stationary spins. With the two-dimensional (2D) technique, multiple thin, sequential sections are acquired by using a flow-compensated gradient echo (GRE) sequence. The acquired sections are viewed individually or are reformatted with the maximum intensity projection (MIP) technique to obtain a three-dimensional (3D) image. TOF imaging has several limitations: (1) complex flow pattern producing loss of signal caused by intravoxel dephasing may mimic disease; (2) vessels not perpendicular to the acquired section plane may cause low signal intensity; (3) retrograde flow in collateral vessels may be saturated also, obscuring the true level of steno-occlusive lesions. Although arterial signal can be improved with cardiac gating, imaging times become long, and arterial signal on TOF MR angiography often remains inhomogeneous and unreliable for proper depiction of the aorta and its branches. Because of the long imaging times and aforementioned limitations, TOF imaging is being replaced rapidly with contrast-enhanced MR angiography.
The TOF effect can be useful when acquired in a 2D cine mode, for example, cine gradient echo (cine GRE). Cine GRE images are acquired with ECG gating, thus resulting in high temporal resolution throughout the cardiac cycle, and can be displayed in cine format. The recently introduced SSFP (commercially known as “true fast imaging with steady precession (FISP),” “fast imaging employing steady state acquisition (FIESTA),” or “balanced fast field echo (FFE”) technique, with shorter TE and TR sequences, has become more widely available. On SSFP, intraluminal signal generally is very high and homogenous even in cases of turbulent flow because this sequence depends mainly on a function of the T2/T1 ratio. Hence, in urgent situations, SSFP can be used to demonstrate quickly aortic abnormalities such as an intimal flap and a false lumen in aortic dissection.
One critical advantage of flow-based bright-blood techniques is the ability to perform a functional assessment of blood flow. On cine GRE, turbulent flow produces rapid spin dephasing and results in flow jets extending distal to or downstream from the lesion, thus providing additional information in many pathologic conditions such as coarctation of the aorta, aortic valve insufficiency, and aortic dissection. Particularly in aortic dissection, the detection of entry and reentry sites is a special capability of this method that can be helpful in planning surgical and endovascular treatment. With the use of newer fast GRE pulse sequences with an ultrashort TR and TE, a flow jet may not be present despite the presence of a significant flow disturbance. The very short TE times may be insufficient for a sizable flow jet to form on this faster sequence. In cases of high suspicion, standard GRE sequences can be performed during free breathing ( Fig. 2 ). The longer TE will allow intravoxel dephasing to develop, and a flow jet should be seen if flow is turbulent.
Cine PC is another bright-blood technique that can be used for dynamic evaluation of blood flow. Cine PC depends on the phase shifts that flowing protons experience as they travel along the gradient field. The data obtained with cine PC are processed into two sets of images: magnitude and phase-contrast. PC images display the direction of flow as bright or dark pixels, with their relative signal intensity representing their velocity. Hence, PC images can be used to assess flow direction, which may be important information for proper identification of a vascular structure or for quantifying blood flow.
Contrast-enhanced MR Angiography
Contrast-enhanced MR angiography, which first was described for imaging of aortoiliac disease in 1993, is the most widely accepted method for comprehensive evaluation of the aortic disease. This technique can provide images that have high spatial resolution with a single breathhold and therefore is suitable for the depiction of aortic abnormalities such as aneurysm, dissection, penetrating atherosclerotic ulcer, and Takayasu arteritis.
Contrast-enhanced MR angiography uses the T1-shortening effect of a gadolinium-based contrast agent. By using a gadolinium chelate contrast agent, the T1 of blood is shortened so that the blood appears bright irrespective of flow patterns or velocities. Because signal enhancement and overall image quality of contrast-enhanced MR angiography depend on the intra-arterial concentration of the contrast agent, the correct timing of imaging after contrast material injection is crucial. Because image contrast depends mainly on central k-space data, collection of the central lines of k space during the plateau phase of arterial enhancement is essential for optimal contrast-enhanced MR angiography. The authors use 10 to 20 mL of contrast material delivered at a rate of 2 to 3 mL/s followed by 20 mL of saline solution delivered at the same rate. The dosage and delivery rate of the contrast material should be adjusted in individual patients, with special attention to the acquisition time. Several methods are used to determine the optimal delay between the start of intravenous contrast material injection and the start of image acquisition. Timing methods commonly used include injection of a test bolus using a small amount of contrast material, automatic triggering, and MR fluoroscopy.
Imaging interpretation usually is done with the aid of a computer workstation on which individual source images are analyzed and postprocessing techniques, such as multiplanar volume reformation, MIP reformation, and volume rendering of the images, are performed. MIP images, in particular, can be obtained quickly, resemble catheter angiograms, and permit a 3D appreciation of anatomy ( Fig. 3 ).