MR imaging has been increasingly used as a problem-solving adjunct after an initial ultrasound examination for a variety of penile disorders, and is the best cross-sectional imaging modality for the assessment of urethra and periurethral disease. Critical advantages of MR imaging for penile and urethra imaging include high soft tissue contrast resolution providing detailed anatomic evaluation, which is important for the demonstration and assessment of critical structures such as tunica albuginea or walls of the urethra, larger field of view for better evaluation of extent of disease, and demonstration of proteinaceous material and varying ages of the blood products.
Key points
- •
The use of appropriate MR imaging technique is critical for the assessment of penis, and male and female urethra because the demonstration of critical structures such as the tunica albuginea or walls of the urethra highly depend on the employment of appropriate imaging MR technique, including high-resolution T2-weighted turbo spin echo sequences.
- •
Penile fracture is characterized by discontinuation of normal low T2 signal intensity of tunica albuginea on high-resolution T2-weighted images with associated hematoma showing MR imaging signal, depending on the age of blood products.
- •
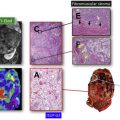
T staging of penile cancer and local extent of urethral carcinoma can be determined with MR imaging according to the extent of the disease on high-resolution T2-weighted images.
- •
MR imaging successfully demonstrates urethral diverticulum and its associated complications, and can differentiate the periurethral disease mimicking urethral diverticulum.
Introduction
Ultrasound examination is the initial and most of the time the primary modality for the evaluation of penis. However, it is limited owing to limited field of view (FOV), operator dependence, and low soft tissue contrast resolution. Therefore, MR imaging has been increasingly used as a problem-solving adjunct after an initial ultrasound study. Additionally, MR imaging is the best cross-sectional imaging modality for the assessment of urethra and periurethral disease owing to its high soft contrast resolution. MR imaging also provides larger FOV for better evaluation of the extent of the disease process, varying ages of the blood products, and critical anatomic structures such as the tunica albuginea.
The most common disease processes of the penis and urethra and their MR imaging findings are reviewed in this article.
Introduction
Ultrasound examination is the initial and most of the time the primary modality for the evaluation of penis. However, it is limited owing to limited field of view (FOV), operator dependence, and low soft tissue contrast resolution. Therefore, MR imaging has been increasingly used as a problem-solving adjunct after an initial ultrasound study. Additionally, MR imaging is the best cross-sectional imaging modality for the assessment of urethra and periurethral disease owing to its high soft contrast resolution. MR imaging also provides larger FOV for better evaluation of the extent of the disease process, varying ages of the blood products, and critical anatomic structures such as the tunica albuginea.
The most common disease processes of the penis and urethra and their MR imaging findings are reviewed in this article.
MR imaging technique
Imaging Technique of the Penis and Male Urethra
MR imaging is performed with the patient in a supine and feet first position on the table either at 1.5 T or 3.0 T magnets. The penis and scrotum should be elevated with a towel located under these structures between the upper thighs. The dorsiflexed penis should be taped against the anterior abdominal wall to prevent any motion. This positioning also enables a good view of anatomy of the penis because the penis is seen at its full length without any curves or folding. Another towel is also used to cover the penis and scrotum before the placement of phased array coil or coils, covering the whole pelvis and lower abdomen.
The examination is usually performed when the penis is in a flaccid state. It is possible to use intracavernosal prostaglandin E1 injections to enable imaging of the erect penis ; however, this usually slows the workflow and necessitates more rigorous workup and screening, we do not perform it at our institution routinely. Additionally, the use of prostaglandin E1 is contraindicated in patients with penile prosthesis and conditions predisposing priapism.
The examination includes 2 portions, including (i) imaging of the penis with sequences having high resolution and (ii) imaging of the whole pelvis extending from the iliac bifurcation to the inferior border of the scrotum with sequences having standard routine resolution. The details of the imaging technique is given in Table 1 .
| Sequence | Plane | TR | TE | Flip Angle | Thickness/Gap | FOV | Matrix |
|---|---|---|---|---|---|---|---|
| Localizer | 3-Plane | — | — | — | — | — | — |
| SS-ETSE | Coronal | 1500 a | 85 | 170 | 6 mm/20% | 350–400 | 192 × 256 |
| SS-ETSE | Axial | 1500 a | 85 | 170 | 6 mm/20% | 350–400 | 192 × 256 |
| SS-ETSE | Sagittal | 1500 a | 85 | 170 | 6 mm/20% | 350 | 192 × 256 |
| SS-ETSE fat suppressed | Axial | 1500 a | 85 | 170 | 8–10 mm/20% | 350–400 | 192 × 256 |
| T1 SGE in/out of phase | Axial | 170 | 2.2/4.4 | 70 | 7 mm/20% | 350–400 | 192 × 320 |
| T2 3D TSE | Axial | 1200 | 120 | 150 | 1.5 mm/— | 250 | 256 × 256 |
| T2 TSE | Axial/coronal/sagittal | 5000 | 80 | 90 | 4 mm/— | 230 | 256 × 256 |
| T2 TSE fat suppressed | Coronal/sagittal | 5000 | 89 | 90 | 4 mm/— | 230 | 256 × 256 |
| Diffusion-weighted imaging | Axial | 4500 | 88 | 90 | 4 mm/— | 270 | 128 × 128 |
| T1 3D GE FS pre | Axial | 3.8 | 1.7 | 10 | 3 mm/— | 350–400 | 160 × 256 |
| Postgadolinium sequences | |||||||
| T1 3D GE fat suppressed b | Axial/coronal/sagittal | 3.8 | 1.7 | 10 | 3 mm/— | 350–400 | 160 × 256 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree