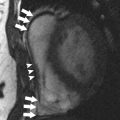
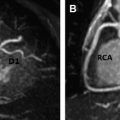
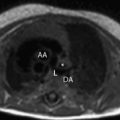
Because of its lack of ionizing radiation, MR imaging is increasingly used for patients with cardiovascular disease, including young women. However, the risks related to the MR environment need to be acknowledged and prevented. For women, there are unique gender-related safety issues that are important to address in cardiovascular MR examinations. This article familiarizes radiologists with MR safety issues and current, evidence-based recommendations for specific situations such as pregnancy or lactation and imaging of women who have pelvic gynecologic devices such as intrauterine devices. Practical algorithms to minimize risk and increase MR safety for these women are suggested. MR imaging has been increasingly used in cardiovascular imaging, especially in young women and during pregnancy, because of the lack of ionizing radiation. Cardiovascular MR scan of women poses gender-specific risks, such as those related to pregnancy, lactation, and use of intrauterine devices. To date, there is no evidence on the short-term and long-term adverse effects of the static magnetic field on human health. The American College of Radiology Guidance Document on MR Safe Practices (2013) states that pregnant patients should undergo MR imaging only if (1) the required information cannot be obtained via other nonionizing means, (2) the information is likely to alter patient care, and (3) the examination cannot wait until after completion of the pregnancy. At present, there is no scientific evidence contraindicating MR imaging in women bearing intrauterine devices. Magnetic Resonance (MR) imaging has been increasingly used in cardiopulmonary imaging, especially in young women and during pregnancy because cardiopulmonary disorders can affect up to 4% of all pregnancies in the industrialized world because of preexisting conditions or conditions acquired during pregnancy. The increased use of MR imaging for cardiovascular imaging in woman is mainly caused by the lack of ionizing radiation, which has made this technique preferable to computed tomography (CT). However, MR has general hazards related to the use of magnetic fields, which can be categorized as static, pulsed radiofrequency (RF), and time-varying gradient electromagnetic fields. The hazards for large static magnetic fields are the biological effects, projectile effect, and implant/monitoring device malfunction and/or displacement. The RF pulses pose problems of tissue and implant heating. For time-varying gradient electromagnetic fields, the hazards are mainly peripheral nerve stimulation and acoustic noise. These general MR hazards are routinely addressed by MR safety procedures, which are applied to prevent and reduce risk. However, there are also specific female gender–related MR hazards, which can be of concern for radiologists, MR technicians, and ordering physicians. This article focuses on familiarizing radiologists with MR safety issues and current, evidence-based recommendations for pregnant or lactating women and for women who have intrauterine devices (IUDs) in place. Practical algorithms to minimize risk and increase MR safety for women are also suggested. The MR system uses 3 types of magnetic fields simultaneously : Static magnetic fields (B 0 ) Time-varying magnetic field gradients RF magnetic fields The static or main magnetic field is used to align the hydrogen protons in the patient’s body. This strong magnetic field is always active, even when the MR scanner is not imaging. The strengths of the static magnetic fields used in clinical and research MR systems range between 1 T and 7 T. The most common systems are 1.5 T and 3 T and these represent 60% to 75% and 5% to 15% of the all MR imaging system in United States, respectively. There are 2 major safety issues related to high static magnetic field strength: attraction of ferromagnetic material toward the magnet and biological effects. Any object containing ferromagnetic material is pulled toward the core of the main magnet and this is known as the projectile effect. Anyone or anything in the direct trajectory of the object can be hit by the object moving toward the magnet, with the risk of severe injuries. Patients must be screened for MR compatibility before being allowed into the MR environment ( Box 1 ). However, current physiologic monitoring devices, instruments, and pacemakers are made to be MR compatible, so the risk of displacement in the body is negligible. Aneurism Clips, Carotid artery vascular clamps Biopsy needles, markers Breast tissue expanders and implants Bone and spinal fusion stimulators Cardiac pacemakers, electrocardiogram electrodes, heart valve prosthesis Cochlear implants, hearing aids Dental implants, devices, and materials Tattoos and permanent make-up Any devices that may contain ferromagnetic material The biological effects of static magnetic fields are still controversial. A review of the safety of high static magnetic field strength on human health concludes that there are no firmly established detrimental effects except for sensory effects, such as vertigo, metallic taste, and magnetophosphenes. The International Commission on Non-Ionizing Radiation Protection (ICNIRP) stated that there is no evidence on the short-term and long-term adverse effects of the static magnetic field on human health. The function of the time-varying magnetic field gradients in an MR system is to determine position-dependent variation in magnetic field strength. The main safety concerns with time-varying magnetic field gradients are related to biological effects and acoustic noise. Time-varying magnetic fields generate electric fields and circulating currents in conductive tissues of the human body and these induced electric currents could interfere with the normal function of nerve cells and muscle fibers. However, at the strength used in medical imaging, these effects are thought to be minimal and not harmful. A second problem related to the switching on and off of the gradient is the production of a substantial amount of acoustic noise. This noise is frequently described as tapping, knocking, or twitting sounds. Intensity and frequency of these noises vary accordingly to the MR imaging parameters and sequences and usually increase with reductions in slice thickness, field of view, repetition time, and echo time. Temporary hearing loss has been reported using conventional sequences. For this reason ear plugs or noise reduction headphones are routinely used for MR imaging examination. RF pulses are used in MR for nuclei excitation. RF pulses can interact with both tissues and any medical devices implanted in the patient. During an MR scan, a large part of RF pulse energy is transferred into the human body as heat. This tissue heating is largest at the body surface and minimal at the center of the body. The dosimetric parameter used to quantify RF energy deposition is represented in terms of specific absorption ratio (SAR), which is normally measured in Watts per kilogram. All MR systems monitor the level of SAR during image acquisition, and the admitted SAR is usually 4 W/kg for a whole-body scanner, calculated for a body temperature increase of up to 0.6°C and a scanning time of 20 to 30 minutes. For a given pulse sequence, the SAR depends on the static magnetic field strength, flip angle, number of RF pulses during each repetition time of the sequence, and spacing between the RF pulses. An increase in the first 3 parameters and a decrease in the last parameter can all cause an increase in SAR. Three operational levels of SAR are defined by the ICNIRP : The normal level, which causes no physiologic stress to patients The first level, which may cause physiologic stress to the patient that may need to be controlled by medical supervision The second level, in which a significant patient risk may be produced and for which explicit approval is required Note that it has been shown that, when the average whole-body SAR remains below the safety limits, hot spots can still occur; therefore the automatic control system of the scanner is not sufficient to ensure patient safety. Most of the reported accidents are burns caused by hot spots in the presence of conducting materials close to the patient, such as monitoring equipment, or in patients with tattoos and permanent cosmetics made with iron oxide or other metal-based pigments. Adverse reactions to gadolinium-based contrast agent (GBCA) are classified as renal and nonrenal. The main adverse renal reaction is nephrogenic systemic fibrosis (NSF), which is a serious medical condition associated with exposure to GBCAs in patients with renal insufficiency or on dialysis. Because NSF only occurs in patients with impaired renal function, GBCA administration is contraindicated in patients with chronic kidney disease (glomerular filtration rate [GFR] <30 mL/min/1.73 m 2 ) and in patients with acute kidney injury according the American College of Radiology (ACR) guidelines. In patients with GFR less than 60 mL/min/1.73 m 2 , a half dose of GBCAs should be considered. Nonrenal adverse reactions are mainly allergic reactions such as nausea, hives, taste disturbance, and anaphylactoid reactions. These reactions are rare, occurring in less than 0.01% of the patients. Special precaution is indicated in patients with asthma or history of allergies because the likelihood of adverse reactions is higher in these groups of patients. Gender-related issues that may affect MR safety include pregnancy, lactation, and the presence of IUDs. MR imaging is frequently used in pregnant patients when additional information is needed to guide management beyond that available with ultrasonography, which is usually the first-line imaging method. MR is preferred to CT because of the lack of ionizing radiation. Although MR imaging has not been shown to have any deleterious effects on the fetus, the safety of MR imaging during pregnancy has yet to be definitively established. There are 3 potential hazardous effects that MR imaging can have on the fetus : Potential biological damage related to cell migration, proliferation, and differentiation, possibly leading to miscarriage caused by exposure to the static magnetic field Tissue heating potential and secondary damage, particularly with regard to organogenesis caused by energy deposition by RF pulses Potential damage to the fetal ear (especially after 24 weeks’ gestation) caused by the high acoustic noise level in varying gradient electromagnetic fields, particularly with fast-acquisition sequences Although no harmful effects have been shown using diagnostic MR in pregnancy, the ACR Guidance Document on MR Safe Practices (2013) states that pregnant patients should undergo MR imaging only if (1) the required information cannot be obtained via other nonionizing means, (2) the information is likely to alter patient care, and (3) the examination cannot wait until after completion of the pregnancy. The static magnetic field of MR imaging can potentially alter cell migration, proliferation, and differentiation within the fetus, resulting in teratogenesis. Most of the studies supporting this have been performed in animals and with controversial results. Multiple studies in humans show no scientific evidence of teratogenesis up to 9 years after exposure to MR imaging in utero. In terms of risks of MR imaging exposure, the ACR does not distinguish between the first trimester of pregnancy and the second and third trimesters. As per the ACR White Paper, at any stage during pregnancy, a risk-benefit analysis should be performed before MR imaging. Because the risk of MR at 1.5 T is theoretic, if MR imaging information is needed for patient care, the risk-benefit analysis will decide in favor of performing the clinically indicated study. Human embryos and fetuses are vulnerable to chemical and physical insults during defined stages of development. As described earlier, exposure to RF pulses can cause tissue heating, with subsequent heating of fetal stem cells and, as a result, potential teratogenesis. The fetus is entirely dependent on maternal temperature as well as circulation to avoid hyperthermia. Spontaneous abortion and malformations in the fetus have been reported as a result of maternal fever (≥37.8°C) and hot tub use. In general, maternal temperature more than 2°C greater than normal for extended periods, or 2°C to 2.5°C greater than normal for 0.5 to 1 hour, have been reported in the literature as thresholds for heat-induced fetal abnormalities. The incidence of these abnormalities is directly proportional to the grade of temperature increase and exposure duration. This stage of organogenesis is most susceptible to hyperthermia because of rapid cell proliferation but the time window of the organogenesis varies according the organ considered. SAR units for MR imaging are regulated by the US Food and Drug Administration (FDA), which currently makes no specific recommendations for pregnant patients. For pregnant patients, ICNIRP guidelines state that exposure duration should be reduced to the minimum and only at the normal operation level. However, most heating created by MR imaging is superficial and is absorbed by the maternal body with only a fraction reaching the fetus. Further, in the study by Hand and colleagues, fetal SAR and fetal temperature were shown to be within international safety limits for MR imaging procedures compliant with the ICNIRP. An international consensus states that MR imaging of pregnant patients should be performed with up to 3.0 T magnets or less to minimize SAR. In summary, heating related to RF magnetic fields is unlikely to be teratogenic, but to date no epidemiologic studies are available to assess possible long-term health effects caused by these nonionizing MR radiations. By 24 weeks of pregnancy, the fetal ear develops and is able to hear noise. A study on noise exposure in pregnancy for the American Academy of Pediatrics found higher frequency hearing loss, shortened gestation, and decreased birth weight in the exposed group compared with the control group. The effect of MR imaging noise on the fetus is of concern because pregnant women are protected by headphones or earplugs, but the fetuses are not. The MR imaging noise level can be as high as 80 to 120 dB, but the maternal body attenuates the noise substantially, by at least 30 dB. This attenuation results in less than 90 dB of noise reaching the fetal ear. It is noteworthy that 90 dB is suggested by the American Academy of Pediatrics as the upper limit beyond which permanent damage to the fetal ear might be expected. To date, no scientific evidence of acoustic damage in human fetuses has been reported in association with MR imaging exposure. GBCAs injected intravenously cross the placenta by passive diffusion across the chorionic epithelium. The contrast is filtered through the kidneys and subsequently excreted into the amniotic fluid through the urine. Animal studies have shown that only 0.01% of the injected gadolinium dose was present in the fetus 4 hours after contrast injection, with only traces remaining after 24 hours; however, the half-life of gadolinium in the human fetus is unknown. Concern has focused on the toxic free gadolinium ion, which can be formed by dissociation of the ion from the chelating agent. Although the stability of the gadolinium-chelate complex is unknown, one study showed that, even in patients with severely reduced renal function, no free gadolinium ion could be measured in the blood on 5 consecutive days after the administration of contrast medium. Gadolinium has been shown in animal studies to have teratogenic effects when administered at high and repeated doses. Although no human studies have been conducted to assess the teratogenic effect of gadolinium in pregnant women, there have been no harmful events reported so far in human fetuses exposed to GBCAs in utero. In 2013, the ACR stated that GBCAs may be given to pregnant patients if needed, by joint decision of the radiologist and referring physician only when essential to the diagnosis, when no alternative imaging studies are available, and when delaying the MR imaging examination until after delivery would be impossible. The FDA states that GBCA should only be administered in pregnancy if the potential benefit justifies the potential risk to the fetus. No specific neonatal tests are necessary after delivery, because no adverse effects, teratogenesis, or acoustic damage have been documented in association with the use of GBCAs for medical imaging. Only minimal amounts of gadolinium-based contrast material are excreted through breast milk and absorbed by the infant bowel (0.01% of injected dose). This expected absorbed dose is less than 0.05% of the intravenous (IV) contrast amount recommended by the American Academy of Pediatrics for neonates undergoing a gadolinium-enhanced MR imaging study. Thus, as per the ACR Contrast Manual 2013, no interruption of lactation is required if IV gadolinium is administered to a nursing patient. The European Medicines Agency suggests that breastfeeding should be interrupted for more than 24 hours if the mother has been injected with the 3 least thermodynamically stable GBCAs: gadodiamide (Gd-DTPA-BMA), gadoversetamide (Gd-DTPA-BMEA), or gadolinium-diethylenetriamine penta-acetic acid (Gd-DTPA). To date, there is no evidence of adverse reactions occurring in infants who are breastfeeding from mothers previously injected with GBCAs. MR safety in women using IUDs depends on the device structure and composition ( Fig. 1 ). As previously described, the presence of a metallic device in a patient undergoing MR imaging may cause injury from movement or excessive heating of the object. Moreover, metallic devices can cause imaging artifacts, which can hamper the diagnostic accuracy. These artifacts, also known as magnetic susceptibility artifacts, consist of areas of focal loss of signal, surrounded by a hyperintense halo and associated with variable degrees of surrounding tissue distortion. The size and shape of the artifact depends on the size and shape, orientation, and nature of the ferromagnetic device, as well as the sequences used in the examination. IUDs can consist of nonmetallic or metallic components. The nonmetallic IUDs are usually made of plastic and are combined with progesterone. These devices do not pose any risk to women during MR imaging. Metallic IUDs usually contain copper (Cu), which is not ferromagnetic. The main concern in using Cu-IUDs is related to possible injuries to the endometrium or generation of imaging artifacts. Several studies have proved that Cu-IUDs are MR safe and do not produce dislocation, heating, or image artifact. Another metallic gynecologic device is the Essure system (Conceptus Inc, San Carlo, CA), a sterilization method that contains 2 metallic microimplants of stainless steel, nickel, and titanium. Essure has been proved to be safe at magnetic fields up to 3T. At present, there is no scientific evidence contraindicating MR imaging in women bearing gynecologic devices ( Table 1 ).
Key points
Introduction
General Safety Aspects of MR Imaging: Potential Generic Hazards in MR Imaging
Effects of static magnetic fields
Effects of time-varying magnetic field
Effects of radiofrequency fields
Hazard Related to Gadolinium-Based Contrast Agent Administration
Safety Aspects of MR Imaging in Women
MR imaging of pregnant patients
Teratogenesis
Tissue heating
Acoustic damage
Hazards Related to Intravenous Gadolinium-based Contrast Agent Administration During Pregnancy and Lactation
Gadolinium-based contrast agents during pregnancy
Gadolinium-based contrast agents during lactation
MR Safety and Intrauterine Devices